Chapter 8 Heart
Methods of imaging the heart
ANGIOCARDIOGRAPHY
Indications
Equipment
Technique
Image acquisition
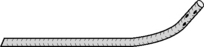
Using digital angiography at 30 frames s−1 with axial alignment of the heart, i.e. the X-ray beam is aligned perpendicular to the long axis of the heart (Fig. 8.4). The long axis of the heart is usually oblique to the long axis of the patient’s body and cardiac angiography suites have movable C-arms which allow correct positioning by movement of the equipment alone without disturbing the patient (Fig. 8.4b). Further rotation of the direction of the X-ray beam is used to profile those areas of the heart under examination. Useful views are:
CORONARY ARTERIOGRAPHY
Indications
Diagnostic arteriography can be supplemented by intravascular ultrasound (US) to determine the nature and extent of plaque within the vessel wall or angioscopy in some centres.
Equipment
Technique
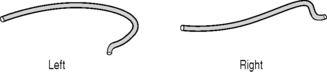
The catheter is introduced using the Seldinger technique via the radial, brachial or femoral artery and advanced until its tip lies in the ostium of the coronary artery.
Image acquisition
Angiography (30 frames s−1) is performed in the following positions:
CARDIAC COMPUTED TOMOGRAPHY (INCLUDING CORONARY COMPUTED TOMOGRAPHIC ANGIOGRAPHY)
As a result of advances in CT technology, non-invasive cardiac imaging is becoming central to the diagnosis and management of patients with cardiac disease. This is the result of fast scan times and cardiac gating facilities available with multidetector CT scanners. Whilst the examination is tailored to assessment of the cardiac structures, CT imaging gives the benefit over conventional cardiac and coronary angiography of demonstrating clinically significant non-cardiac findings within the adjacent mediastinum, lungs or upper abdomen,1 and can give additional information regarding plaque characterization.
Cardiac CT may be performed as:
The coronary artery calcium (CAC) score is calculated from the volume of calcium present in the coronary arteries. A high score indicates an increased risk of adverse coronary events and CAC scoring has been used as a screening tool for subclinical cardiac disease. Absence of coronary artery calcification does not exclude atheroma but is associated with a low risk of adverse coronary event. Evidence shows that scores will probably need to be matched to age, sex and ethnic background.2
Coronary computed tomographic angiography
Documented mean effective radiation dose for coronary CTA ranges from 6 to 25 mSv3 and reported mean effective dose for conventional catheter angiography is 5.6 mSv.4 Further improvements in CT technology continue to reduce effective dose but there must be constant awareness with attempt to minimize dose wherever possible. Tailored coronary CTA is well-documented to have a high negative predictive value for coronary artery stenosis.5,6
Indications
Technique
The exact technique will depend on individual CT scanner technology and requires a multidetector CT which is 16 slice or above. Each CT manufacturer will advise scan protocols tailored to their specific scanners; however, general parameters useful for coronary artery assessment cardiac CT are as follows:7
1 Weinreb J.C., Larson P.A., Woodard P.K., et al. American College of Radiology clinical statement on noninvasive cardiac imaging. Radiology. 2005;235:723-727.
2 Preis S.R., O’Donnell C.J. Coronary heart disease risk assessment by traditional risk factors and newer subclinical disease imaging: is a ‘one-size-fits-all’ approach the best option? Editorial. Arch. Intern. Med.. 2007;167(22):2399-2401.
3 Mahesh M., Cody D.D. AAPM/RSNA physics tutorial for residents: physics of cardiac imaging with multiple-row detector CT. RadioGraphics. 2007;27:1495-1509.
4 Coles D.R., Smail M.A., Negus I.S., et al. Comparison of radiation doses from multislice computed tomography coronary angiography and conventional diagnostic angiography. J. Am. Coll. Cardiol.. 2006;47:1840-1845.
5 Abdulla J., Abildstrom S.Z., Gotzsche O., et al. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur. Heart J.. 2007;28(24):3042-3050.
6 Nieman K., Cademartiri F., Lemos P.A., et al. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002;106:2051-2054.
7 Schoepf U.J., Zwerner P.L., Savino G., et al. Coronary CT angiography: how I do it. Radiology. 2007;244:48-63.
8 Earls J.P., Berman E.L., Urban B.A., et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology. 2008;246:742-753.
9 Pugliese F., Mollet N.R., Hunink M.G., et al. Diagnostic performance of coronary CT angiography by using different generations of multisection scanners: single center experience. Radiology. 2008;246:384-393.
Gershlick A.H., de Belder M., Chambers J., et al. Role of non-invasive imaging in the management of coronary artery disease: an assessment of likely change over the next 10 years. A report from the British Cardiovascular Society Working Group. Heart. 2007;93:423-431.
Vanhoenacker P.K., Heijenbrok-Kal M.H., Van Heste R., et al. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology. 2007;244:419-428.
Radionuclide Ventriculography
Patient preparation
Technique
Gated blood-pool study
List mode is best, where individual events are stored as their x, y coordinates along with timing and gating pulses. This allows maximum flexibility for later manipulation and framing of data. Around 5 million counts should be acquired. However, MUGA mode is adequate, and is still the most commonly used. In this, the start of an acquisition cycle is usually triggered by the R wave of the patient’s ECG. A series of 16–32 fast frames are recorded before the next R wave occurs. Each of these has very few counts in from a single cycle, so every time the R wave trigger arrives another set of frames is recorded and summed with the first. The sequence continues until 100–200 kilo-counts per frame have been acquired in about 10 min. Some degree of arrhythmia can be tolerated using the technique of ‘buffered bad beat rejection’, where cardiac cycles of irregular length are rejected and the data not included in the images. The length of time to acquire an image set increases as the proportion of rejected beats rises.
First-pass radionuclide angiography
Images
Additional techniques
1 Metcalfe M.J. Radionuclide ventriculography. In: Sharp P.F., Gemmell H.G., Murray A.D., editors. Practical Nuclear Medicine. London: Springer, 2005.
2 Friedman J.D., Berman D.S., Borges-Neto S., et al. First-pass radionuclide angiography. J. Nucl. Cardiol.. 2006;13(6):e42-e55.
3 Williams K.A. Measurement of ventricular function with scintigraphic techniques: part 1 imaging hardware, radiopharmaceuticals, and first-pass radionuclide angiography. J. Nucl. Cardiol.. 2005;12(1):86-95.
4 Konishi T., Koyama T., Aoki T., et al. Radionuclide assessment of left ventricular function during dobutamine infusion in patients with coronary artery disease: comparison with ergometer exercise. Clin. Cardiol.. 1990;13:183-188.
5 Fukuoka S., Maeno M., Nakagawa S., et al. Feasibility of myocardial dual-isotope perfusion imaging combined with gated single photon emission tomography for assessing coronary artery disease. Nucl. Med. Commun.. 2002;23(1):19-29.
6 Anagnostopoulos C., Underwood S.R. Simultaneous assessment of myocardial perfusion and function: how and when? Eur. J. Nucl. Med.. 1998;25:555-558.
Radionuclide Myocardial Perfusion Imaging
Radiopharmaceuticals1,2
Equipment
Technique
The principal of the technique is to compare myocardial perfusion under conditions of pharmacological stress or physical exercise, with perfusion at rest. Diseased but patent arterial territories will show lower perfusion under stress conditions than healthy arteries, but will show relatively improved perfusion at rest. Infarcted tissue will show no improvement at rest. Hence, prognostic information on the likelihood of adverse cardiac events and the benefits of revascularization can be gained.4
Stress regime
Pharmacological stress has become increasingly widely used instead of physical exercise.5 The optimal stress technique aims to maximize coronary arterial flow. The preferred pharmacological stressing agent is adenosine infusion (0.14 mg kg−1 min−1 for 6 min).6 Adenosine is a potent coronary vasodilator. It reproducibly increases coronary artery flow by more than maximal physical exercise (which often cannot be achieved in this group of patients). It has a short biological half-life of 8–10 s, so most side-effects are reversed simply by discontinuing infusion. Stressing with adenosine has now largely replaced dipyridamole, which will not be discussed here.
There are circumstances where adenosine is contraindicated, e.g. asthma, second-degree heart block or systolic blood pressure <100 mmHg. Dobutamine stress may be employed in these circumstances.7 Dobutamine acts as a ß1 receptor agonist, increasing contractility and heart rate. Under continuous monitoring, the dose is incrementally increased from 5 to 20 μg kg−1 min−1, infusing each dose for 3 min. The infusion is terminated when S-T segment depression of >3 mm, any ventricular arrhythmia, systolic blood pressure >220 mmHg, attainment of maximum heart rate, or any side-effects occur. Dobutamine is contraindicated in patients with aortic aneurysm. New, more specific targeted agents such as regadenoson (A2A adenosine receptor agonist) are being developed which could be used in asthmatic patients rather than dobutamine.8
99mTc-MIBI or tetrofosmin rest/stress test
Because MIBI and tetrofosmin have minimal redistribution, separate injections are needed for stress and rest studies. Two-day protocols are optimal, but it is often more convenient to perform both studies on the same day. A number of groups have shown that this is possible without significantly degrading the results, most effectively when the resting study is performed first.9
2-Day protocol (stress/rest)
1-Day protocol (stress/rest)
201Tl stress/rest test
Images
Spect
Analysis
Additional techniques
1 Reyes E., Loong C.Y., Harbinson M., et al. A comparison of Tl-201, Tc-99m sestamibi, and Tc-99m tetrofosmin myocardial perfusion scinitgraphy in patients with mild to moderate coronary stenosis. J. Nucl. Cardiol.. 2006;13(4):488-494.
2 Kapur A., Latus K.A., Davies G., et al. A comparison of three radionuclide myocardial perfusion tracers in clinical practice: the ROBUST study. Eur. J. Nucl. Med. Mol. Imaging. 2002;29(12):1608-1616.
3 Nandalur K.R., Dwamena B.A., Choudhri A.F., et al. Diagnostic performance of positron emission tomography in the detection of coronary artery disease: a meta-analysis. Acad. Radiol.. 2008;15(4):444-451.
4 Travin M.I., Bergmann S.R. Assessment of myocardial viability. Semin. Nucl. Med.. 2005;35(1):2-16.
5 Travain M.I., Wexler J.P. Pharmacological stress testing. Semin. Nucl. Med.. 1999;29:298-318.
6 Takeishi Y., Takahashi N., Fujiwara S., et al. Myocardial tomography with technetium-99m-tetrofosmin during intravenous infusion of adenosine triphosphate. J. Nucl. Med.. 1998;39:582-586.
7 Verani M.S. Dobutamine myocardial perfusion imaging. J. Nucl. Med.. 1994;35:737-739.
8 Iskandrian A.E., Bateman T.M., Belardinelli L., et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J. Nucl. Cardiol.. 2007;14(5):645-658.
9 Tadehara F., Yamamoto H., Tsujiyama S., et al. Feasibility of a rapid protocol of 1-day single-isotope rest/adenosine stress Tc-99m sestamibi ECG-gated myocardial perfusion imaging. J. Nucl. Cardiol.. 2008;15(1):35-41.
10 Lavalaye J.M., Shroeder-Tanka J.M., Tiel-van Buul M.M., et al. Implementation of technetium-99m MIBI SPECT imaging guidelines: optimizing the two-day stress-rest protocol. Int. J. Card. Imaging. 1997;13:331-335.
11 Thorley P.J., Sheard K.L., Wright D.J., et al. The routine use of sublingual GTN with resting 99 Tcm-tetrofosmin myocardial perfusion imaging. Nucl. Med. Commun.. 1998;19:937-942.
12 Travin M.I., Heller G.V., Johnson L.L., et al. The prognostic value of ECG-gated SPECT imaging in patients undergoing stress Tc-99m sestamibi myocardial perfusion imaging. J. Nucl. Cardiol.. 2004;11(3):253-262.
13 Schwaiger M., Melin J. Cardiological applications of nuclear medicine. Lancet. 1999;354:661-666.
14 Banzo I., Pena F.J., Allende R.H., et al. Prospective clinical comparison of non-corrected and attenuation- and scatter-corrected myocardial perfusion SPECT in patients with suspicion of coronary artery disease. Nucl. Med. Commun.. 2003;24(9):995-1002.
15 Kim Y., Goto H., Kobayshi K., et al. A new method to evaluate ischemic heart disease: combined use of rest thallium-201 myocardial SPECT and Tc-99m exercise tetrofosmin first pass and myocardial SPECT. Ann. Nucl. Med.. 1999;13:147-153.
Magnetic Resonance Imaging of the Cardiac System
One of the earliest applications of cardiac MRI was the anatomical delineation of congenital heart disease when the pathology could not be completely evaluated by echocardiography. More recently cardiac MRI has been found to be a very effective method of functional assessment of the heart. Not only has it an important role in the assessment of ventricular function, myocardial mass and myocardial viability,1,2 but it is also increasingly used for clinical rest and stress perfusion measurements. It is particularly valuable in distinguishing ischaemic from non-ischaemic cardiomyopathy.3
1 Berman D.S., Hachamovitch R., Shaw L.J., et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: assessment of patients with suspected coronary artery disease. J. Nucl. Med.. 2006;47(1):74-82.
2 Weinreb J.C., Larson P.A., Woodard P.K., et al. American College of Radiology clinical statement on noninvasive cardiac imaging. Radiology. 2005;235:723-727.
3 Jackson E., Bellenger N., Seddon M., et al. Ischaemic and non-ischaemic cardiomyopathies – cardiac MRI appearances with delayed enhancement. Clin. Radiol.. 2007;62:395-403.