Healing is the replacement of dead or injured tissue by healthy tissue; this can be accomplished either by regeneration, when the damage is mild and cells can multiply to replace lost tissue, or by repair, which involves the formation of granulation tissue and then a scar. Repair occurs if there is extensive tissue injury or in permanent cell populations.
10.1. The healing process
For regeneration to occur two conditions must be fulfilled. First, there must be little or no disruption to the intercellular matrix, because the matrix provides the ‘scaffolding’ for new cells. Second, the damage must involve cell populations capable of dividing (i.e. labile or stable cell populations). Repair by scar tissue formation occurs if:
• there is significant disruption of the connective tissue matrix
• cells cannot divide to replace lost cells (this occurs in permanent cell populations such as the heart).
When does healing occur?
Healing occurs in damaged tissues. It begins early in the inflammatory reaction, when phagocytes clear dead cells and other debris. If the injury is mild then healing may take place by regeneration; there is replacement of injured tissue with cells of the same type and normal anatomy is restored, leaving no trace of damage. An example is resolution following lobar pneumonia; there is acute inflammation associated with extensive loss of alveolar cells, but there is typically no significant destruction of lung tissue matrix and thus healing by regeneration can take place.
If regeneration is not possible, there is repair by granulation tissue formation and subsequent fibrosis (scarring). This results in loss of specialised cells and hence loss of function. The anatomy is altered, although structural integrity is preserved.
Skin healing has been extensively studied and much of our understanding of the healing process comes from observation of surgical skin wounds. The central pathological process in healing by repair is the formation of granulation tissue.
What is granulation tissue?
This bright pink, granular tissue is seen, for example, in the base of a healing skin wound, and denotes the process of repair. Granulation tissue is composed of:
• small blood vessels (capillary-sized channels)
• proliferating fibroblasts and myofibroblasts
• inflammatory cells.
The development of new blood vessels is called angiogenesis or neovascularisation. Endothelial cells initially form solid cords, but they soon open into capillary loops at the edges of the lesion accompanied by new lymphatic channels. The endothelial cells derive firstly from sprouts produced by adjacent capillaries and secondly from endothelial precursor cells (EPCs) produced in the bone marrow. EPCs are mobilised from the marrow and circulate to the site of injury where they migrate into the tissues. New arterioles and venules are formed as the proliferating capillaries become surrounded by pericytes and smooth muscle cells.
Fibroblasts migrate to the area and produce collagen and other components of the extracellular matrix, such as fibronectin and proteoglycans. Type III collagen tends to be produced first; it is gradually replaced by type I collagen, which is stronger. Many fibroblasts also have significant contractile abilities due to the presence of muscle-type intracytoplasmic filaments; such cells are called myofibroblasts and contract to reduce the wound size. Consequently, the volume of a scar is generally less than the volume of the original tissue damage.
Granulation tissue also contains a variety of inflammatory cells, the types and proportions of which depend on the cause of the tissue damage. For example, granulation tissue surrounding an abscess is rich in neutrophils.
The transformation of necrotic material or fibrin to a fibrous scar by granulation tissue is called organisation. The granulation tissue grows into the dead tissue and eventually replaces it.
The cellular events in healing are orchestrated by a large number of cytokines. For example, epidermal growth factor (EGF), produced by epidermal cells around the damaged area, is important in stimulating regeneration of epithelial cells. Neovascularisation is triggered by fibroblast growth factor (FGF) and various endothelial growth factors, which are produced by macrophages. FGF and transforming growth factor beta (TGF-β), again derived from macrophages, and platelet-derived growth factor (PDGF) from platelets in the clot in the wound, are important mediators of fibroblast activity.
Scarring
Over the course of a few weeks granulation tissue matures into a scar. This process is called fibrosis. The inflammatory cells gradually disappear and the amount of collagen in the matrix increases, with type III collagen being replaced by type I. The new blood vessels are remodelled and the (myo)fibroblasts reduce in number. The final result is a mature scar mainly composed of collagen-rich matrix and scattered residual fibroblasts supplied by a new circulation. After the scar has formed, its strength increases over subsequent months through increased cross-linking of collagen and increased collagen fibre diameter. The collagen fibres also align themselves along lines of stress. This remodelling of the scar requires the production of metalloproteinases, a family of enzymes that degrade collagen, by fibroblasts and other cells such as macrophages.
Scarring provides benefit by restoring the integrity of the damaged tissue but it may have significant complications. Scar tissue tends to contract with time and will not function in the same way as the original tissue. Examples of consequences arising from fibrosis include:
• cosmetic problems produced by unsightly scar tissue
• skin contractures following severe burns that can limit movement
• obstruction of tubular structures due to fibrous narrowing (stricture formation), e.g. duodenal obstruction following healing of a peptic ulcer
• heart failure due to impaired left ventricular function following myocardial infarction and scarring
• adhesion formation – adhesions are scars that stick serosal surfaces together; they can follow organisation of fibrinous exudates in serosal cavities (occasionally, peritoneal adhesions can cause bowel obstruction).
Examples of types of tissue healing
Skin wound healing
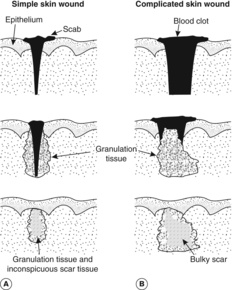
There are two pathways by which skin wounds are repaired, named primary and secondary union. Similar principles apply elsewhere in the body. A simple incised surgical wound will heal by primary union (also called healing by primary intention). This means that the clean edges of a wound once placed together (apposed) will heal quickly with minimal granulation tissue formation and thus minimal scarring (Figure 25A). There are several stages:
1. Blood escapes from damaged vessels and fills the gap.
2. Fibrin clot binds the edges together loosely and dries on the surface, forming a scab.
3. An acute inflammatory reaction develops around the wound in 24 hours and the exudate adds more fibrin, polymorphs and macrophages to the wound. These produce lytic enzymes which start to digest any clot and remove any debris from the wound site.
4. Epithelial cells start to regenerate and bridge the gap within 48 hours.
5. Fibrin in the wound provides stability so that blood vessels can regrow. Only a small amount of granulation tissue forms and the final scar will be thin and inconspicuous.
If the wound is large and gaping, infected, or there is substantial tissue loss, e.g. a large burn or ulcer, then healing by secondary union (secondary intention) takes place (Figure 25B). Granulation tissue forms at the base of the wound and fills it up. Epithelial cells can then regenerate over this ‘bridge’. Fibroblasts migrate into the wound and, by about day 4, begin producing type III collagen, which has a relatively low tensile strength but forms a scaffolding for other cells. Later, the stronger type I collagen is the dominant form. The resulting scar is broad and conspicuous since a large amount of granulation tissue was formed.
Bone fracture healing
When a bone breaks, haematoma (blood clot) forms around the broken ends of the bone. Healing occurs through organisation of this haematoma by granulation tissue. However, this process is modified because the granulation tissue contains proliferating cells derived from the periosteum and endosteum which differentiate into chondroblasts and osteoblasts that lay down new cartilage and immature (woven) bone. The result is hard tissue called callus surrounding and joining the broken ends of the bone. Bony union occurs when new bone produced in the callus links the bone fragments together. The cartilage and woven bone are gradually replaced by lamellar bone (the type found in mature bone). This new bone can be remodelled so that the anatomy can return close to normal. However, the fractured bone fragments must be aligned and placed together (apposed) for optimum healing to occur, otherwise the callus may not adequately bridge the gap between them, resulting in permanent deformity.
Note that normal fracture healing does not result in a fibrous scar, because of the modified nature of the granulation tissue.
Gastrointestinal tract
An ulcer is a defect in an epithelial surface. In the gastrointestinal tract, an ulcer confined to the mucosa is often called an erosion; such lesions can heal by regeneration. In contrast, an ulcer that extends beyond the mucosa will heal by granulation tissue formation and scarring with re-epithelialisation of the surface.
10.2. Factors affecting wound healing
Ideally, healing occurs quickly with resolution or the formation of a strong scar. However, a variety of factors will adversely affect this process.
Local factors
Tissue apposition
The edges of a wound or a broken bone need to be closely aligned for healing to be most effective. Otherwise, large amounts of granulation tissue are required to bridge the gap.
Infection
An infected wound or tissue will take longer to heal because the persistent inflammation associated with host defence will prevent regeneration and inhibit scar formation.
Dead tissue
This must be removed surgically (debridement) or naturally by phagocytosis (macrophages, neutrophils) before healing can be completed. Persistence of necrotic tissue inhibits healing.
Blood supply
Ischaemic tissues do not heal properly because blood brings the cells involved in healing to the site and provides oxygen for their high metabolic demands.
Foreign body
A foreign body, whether introduced accidentally at the time of injury or a prosthesis introduced surgically, can have an adverse effect on healing. In part, this is because the foreign object acts as a ‘sanctuary site’ where bacteria can grow partially protected from the host defence mechanisms.
General factors
Diet
An adequate diet is important to ensure healing processes can occur. For example, vitamin C deficiency (scurvy) leads to inadequate collagen formation and poor healing. Generalised starvation/malnutrition is associated with lack of dietary proteins and depression of immunity, causing poor wound healing.
Therapy
Many modern therapeutic treatments may adversely affect a particular stage of the healing process. Steroids inhibit the growth of new blood vessels and many macrophage functions. Immunosuppressive drugs prevent the natural immune response involved in healing. Many anti-cancer drugs inhibit stages in the cell cycle or kill cells involved in active proliferation – healing can be profoundly affected because it involves the multiplication of many different cells. Likewise, radiotherapy also destroys actively dividing cells.
Blood supply
Blood brings many of the vital ingredients of the healing process, e.g. inflammatory cells and EPCs, immunoglobulins and acute phase proteins, and oxygen and nutrients. Tissue that has a poor blood supply tends to heal poorly. Thus, severe atherosclerosis leads to an inadequate blood supply to wounded tissues (commonly seen in the distal lower limb), and heart failure can cause generalised poor perfusion.
Self-assessment: questions
One best answer questions
2. In which of the following circumstances is healing by resolution most likely?
a. a 10cm diameter full-thickness burn to the forearm
b. a 5cm ulcer of the ankle in a diabetic person
c. myocardial infarction of the lateral wall of the left ventricle
d. lobar pneumonia with consolidation of the left lower lobe
e. a 3cm diameter chronic abscess of the liver
3. Endothelial precursor cells are mainly produced in the:
a. bone marrow
b. liver
c. lung
d. skin
e. thymus
4. A patient has skin damage due to trauma that heals by fibrosis. Which of the following is mainly responsible for contraction of the wound?
a. endothelial cells
b. fibroblasts
c. macrophages
d. myofibroblasts
e. smooth muscle cells
5. A mature scar differs from granulation tissue in that it has more:
a. blood vessels
b. crossed-linked collagen
c. fibroblasts
d. inflammatory cells
e. type III collagen
True-false questions
1. A deficiency of the following is known to impair wound healing:
a. vitamin C
b. lead
c. vitamin B12
d. zinc
e. corticosteroids
2. The following are characteristic of healing by primary union (healing by first intention) in the skin:
a. large amounts of granulation tissue
b. close apposition of skin edges
c. relatively inconspicuous scarring
d. production of type I and type III collagen
e. proliferation of epidermal cells
Case history questions
Case history 1
A 37-year-old fireman suffers full-thickness burns to the skin of his hands, face and neck during the course of his duties.
1. What is a full-thickness skin burn and how might it heal?
Two weeks later, one of the burns is inflamed and exuding pus. A wound swab grows Staphylococcus aureus.
2. Will the presence of Staph. aureus have any effect on healing? Explain your answer.
Six months after this episode, he develops pain in his neck at the site of the burn scar. The scar and skin around it appear twisted and distorted.
3. What complication has occurred?
Case history 2
An 89-year-old woman falls in the street and suffers a compound fracture of her lower right forearm. She takes tolbutamide for diabetes and prednisolone for temporal arteritis. She is otherwise in good general health, although she takes vitamin C supplements she buys from the supermarket.
1. Identify local and systemic factors in the above vignette that might inhibit healing of the fracture.
The woman is treated with antibiotics and the fracture is surgically immobilised with the bone ends in close apposition.
2. Describe the stages of healing in fractures of this type.
Self-assessment: answers
One best answer
2. d. Lobar pneumonia typically resolves, unless there are complications that damage the alveolar walls. The burn, ankle ulcer and chronic abscess will be associated with severe tissue destruction, precluding healing by resolution. The myocardial infarct (no matter what its size) will not resolve either, because adult heart muscle cells do not regenerate. These conditions will heal by granulation tissue formation and fibrosis.
3. a. EPCs are produced in the bone marrow and circulate to sites of injury where they participate in angiogenesis.
4. d. Myofibroblasts have contractile filaments in their cytoplasm and are an important component of granulation tissue.
5. b. A mature scar is characterised by a predominance of type I collagen that shows increasing cross-linking as it remodels. The numbers of cells and blood vessels diminish as granulation tissue turns into a scar.
True-false answers
1.
a. True. Vitamin C is required as a co-factor in collagen synthesis. A deficiency of this vitamin leads to scurvy.
b. False. Lead is poisonous and even in small amounts is detrimental to humans.
c. False. Vitamin B12 deficiency causes a macrocytic megaloblastic anaemia.
d. True. Zinc, like vitamin C, is required for normal collagen synthesis. Zinc supplements can improve wound healing in zinc-deficient patients.
e. False. It is an excess of corticosteroids that hinders wound healing. This is a side effect of steroid therapy, and is also seen in Cushing’s syndrome.
2.
a. False. Primary union involves minimal granulation tissue.
b. True. Unless the skin edges are brought together, primary union cannot occur.
c. True. In contrast, secondary union produces relatively large amounts of scar tissue.
d. True. All healing by repair involves collagen production – type III predominates early in the process, type I later.
e. True. Epidermal cells multiply and spread over the top of the defect. In primary union, this only takes a few days, whereas in secondary union it may take weeks or months, depending on the size of the defect and whether factors inhibiting healing are present.
Case history answers
Case history 1
1. A full-thickness burn extends deeper than the dermis, i.e. it involves subcutaneous tissue. Granulation tissue will form in the exposed subcutaneous tissue. Because the epithelial cells of the skin have all been destroyed, re-epithelialisation of the surface will take place from the edges of the burn where viable skin remains; this process may take a long time (hence, skin grafts are often used to treat burns of this sort).
2. The presence of infection in this case may delay healing, because infection inhibits the healing process. In addition, there may be larger amounts of granulation tissue production as a result of continuing tissue damage, so the final scar may be larger.
3. The scar has contracted (largely as a result of the contractile properties of myofibroblasts) causing the distortion. This phenomenon of distorted contraction of a scar is known as cicatrisation or contracture formation, and is particularly common in large, full-thickness burns.
Case history 2
1. Local and systemic factors in the above vignette that might inhibit healing of the fracture are:
• Age – as an elderly person, her immune and healing responses may be diminished.
• Compound fracture (i.e. there is a breach in the overlying skin) – may allow infection or foreign bodies into the fracture site.
• Diabetes – inhibits the immune response. It also causes atherosclerosis and microangiopathy (see chapter on diabetes) that could cause poor blood supply, although this is more commonly a problem in the lower limbs.
• Steroid therapy – inhibits healing through its effects on macrophage function and endothelial cell regeneration.
2. In the few hours after the fracture, blood forms a haematoma at the fracture site. Within 1–2days, neutrophils and macrophages begin to digest the haematoma. At around day 3, granulation tissue forms and begins to organise the haematoma. This granulation tissue also contains chondroblasts and osteoblasts that produce cartilage and woven bone. In 1–2weeks this modified granulation tissue becomes hard as the cartilage and bone are calcified, producing callus that seals the bone ends. The bone is remodelled over the subsequent weeks, until eventually the fractured fragments are linked by lamellar bone. Remodelling continues for several months: the strength of the bone increases, the cortex reappears and the contour of the bone approaches normal.