Head and Face
Casualty officers and clinicians working in emergency care settings are often the ones who assess the head and face. In these settings, the assessment involves the bony aspects of the head and face as well as the soft tissues. The soft-tissue assessment involves primarily the sensory organs, such as the skin, eyes, nose, and ears, whereas the muscles are tested only as they relate to injury to these structures. Joints and their integrity are not the main objects of the assessment. Because the temporomandibular joints and cervical spine are discussed in Chapters 3 and 4, this chapter deals with only the head, the face, and their associated structures.
Applied Anatomy
The head and face are made up of the cranial vault and facial bones. The cranial vault, or skull, is composed of several bones: one frontal, two sphenoid, two parietal, two temporal, and one occipital (Figure 2-1). Of these, the strongest is the occipital bone, and the weakest are the temporal bones. The frontal bone forms the forehead, and the temporal and sphenoid bones form the anterolateral walls of the skull, or the temples of the head. The parietal bones form the top and posterolateral portions of the skull, and the occipital bones form the posterior portion of the skull. The cranial vault reaches 90% of its ultimate size by age 5.
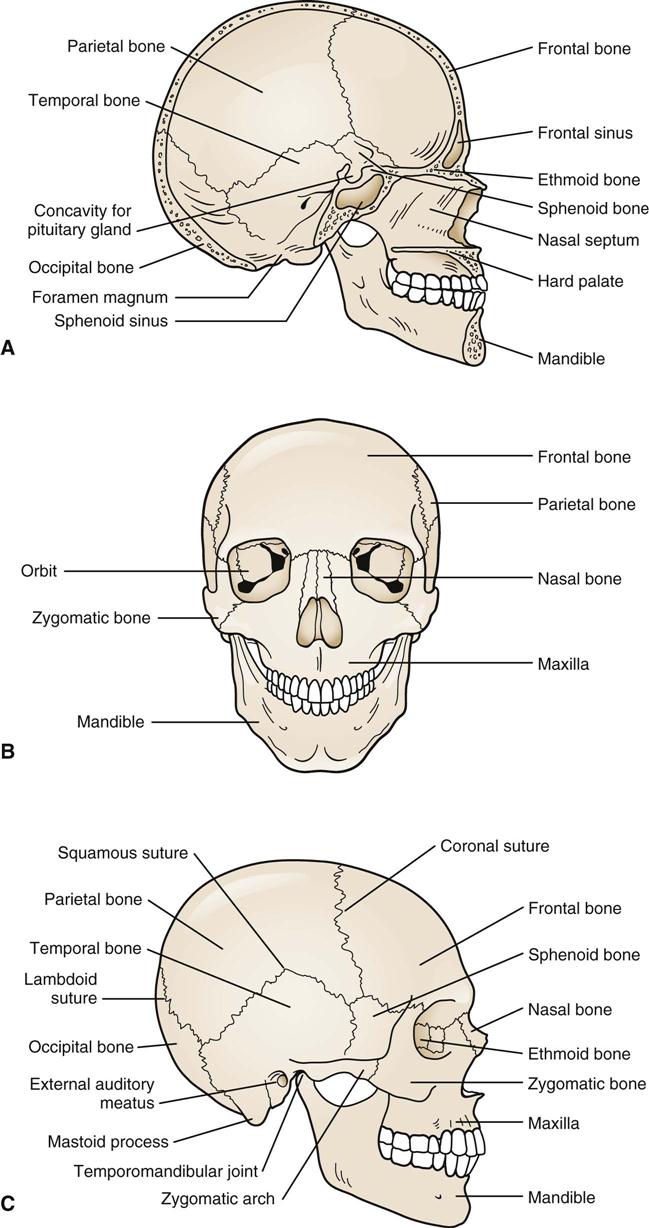
A, Interior view. B, Anterior view. C, Lateral view. (Redrawn from Jenkins DB: Hollinshead’s functional anatomy of the limbs and back, Philadelphia, 1991, WB Saunders, pp. 332–333.)
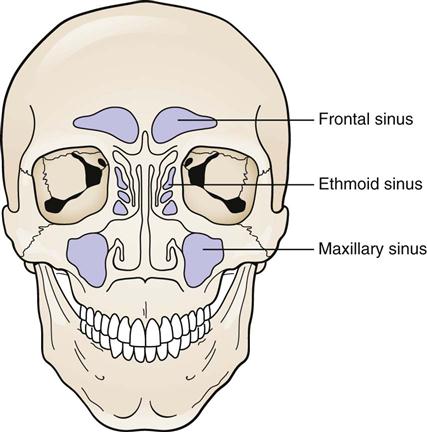
In addition to the cranial vault bones, there are 14 facial bones. These bones develop more slowly than the cranial bones, reaching only 60% of their ultimate size by age 6. The facial skeleton is composed of the mandible, which forms the lower jaw; the maxilla, which forms the upper jaw on each side; the nasal bones, which form the bridge of the nose; and the palatine, lacrimal, zygomatic, and ethmoid bones, which form the remainder of the face. It is the zygomatic bone that gives the cheek its prominence. The sphenoid bones also form part of the orbital cavity. The facial skull has several cavities for the eyes (orbital), nose (nasal), and mouth (oral), as well as spaces for nerves and blood vessels to penetrate the bony structure. Weight is saved in the skull area by the addition of sinus cavities (Figure 2-2).
The muscles of the head and face are controlled primarily by the 12 cranial nerves. The cranial nerves and their chief functions are shown in Table 2-1. The cranial nerves generally contain both sensory and motor fibers. However, some cranial nerves are strictly sensory (olfactory and optic), whereas others are strictly motor (oculomotor, trochlear, and hypoglossal).
TABLE 2-1
Cranial Nerves and Methods of Testing
| Nerve | Afferent (Sensory) | Efferent (Motor) | Test |
| I. Olfactory | Smell: Nose | — | Identify familiar odors (e.g., chocolate, coffee) |
| II. Optic | Sight: Eye | — | Test visual fields |
| III. Oculomotor | — | Voluntary motor: Levator of eyelid; superior, medial, and inferior recti; inferior oblique muscle of eyeball Autonomic: Smooth muscle of eyeball |
Upward, downward, and medial gaze Reaction to light |
| IV. Trochlear | Voluntary motor: Superior oblique muscle of eyeball | Downward and lateral gaze | |
| V. Trigeminal | Touch, pain: Skin of face, mucous membranes of nose, sinuses, mouth, anterior tongue | Voluntary motor: Muscles of mastication | Corneal reflex Face sensation Clench teeth; push down on chin to separate jaws |
| VI. Abducens | Voluntary motor: Lateral rectus muscle of eyeball | Lateral gaze | |
| VII. Facial | Taste: Anterior tongue | Voluntary motor: Facial muscles Autonomic: Lacrimal, submandibular, and sublingual glands |
Close eyes tight Smile and show teeth Whistle and puff cheeks Identify familiar tastes (e.g., sweet, sour) |
| VIII. Vestibulocochlear (acoustic nerve) | Hearing: Ear Balance: Ear |
— | Hear watch ticking Hearing tests Balance and coordination test |
| IX. Glossopharyngeal | Touch, pain: Posterior tongue, pharynx Taste: Posterior tongue |
Voluntary motor: Unimportant muscle of pharynx Autonomic: Parotid gland | Gag reflex Ability to swallow |
| X. Vagus | Touch, pain: Pharynx, larynx, bronchi Taste: Tongue, epiglottis |
Voluntary motor: Muscles of palate, pharynx, and larynx Autonomic: Thoracic and abdominal viscera |
Gag reflex Ability to swallow Say “Ah” |
| XI. Accessory | — | Voluntary motor: Sternocleidomastoid and trapezius muscle | Resisted shoulder shrug |
| XII. Hypoglossal | — | Voluntary motor: Muscles of tongue | Tongue protrusion (if injured, tongue deviates toward injured side) |
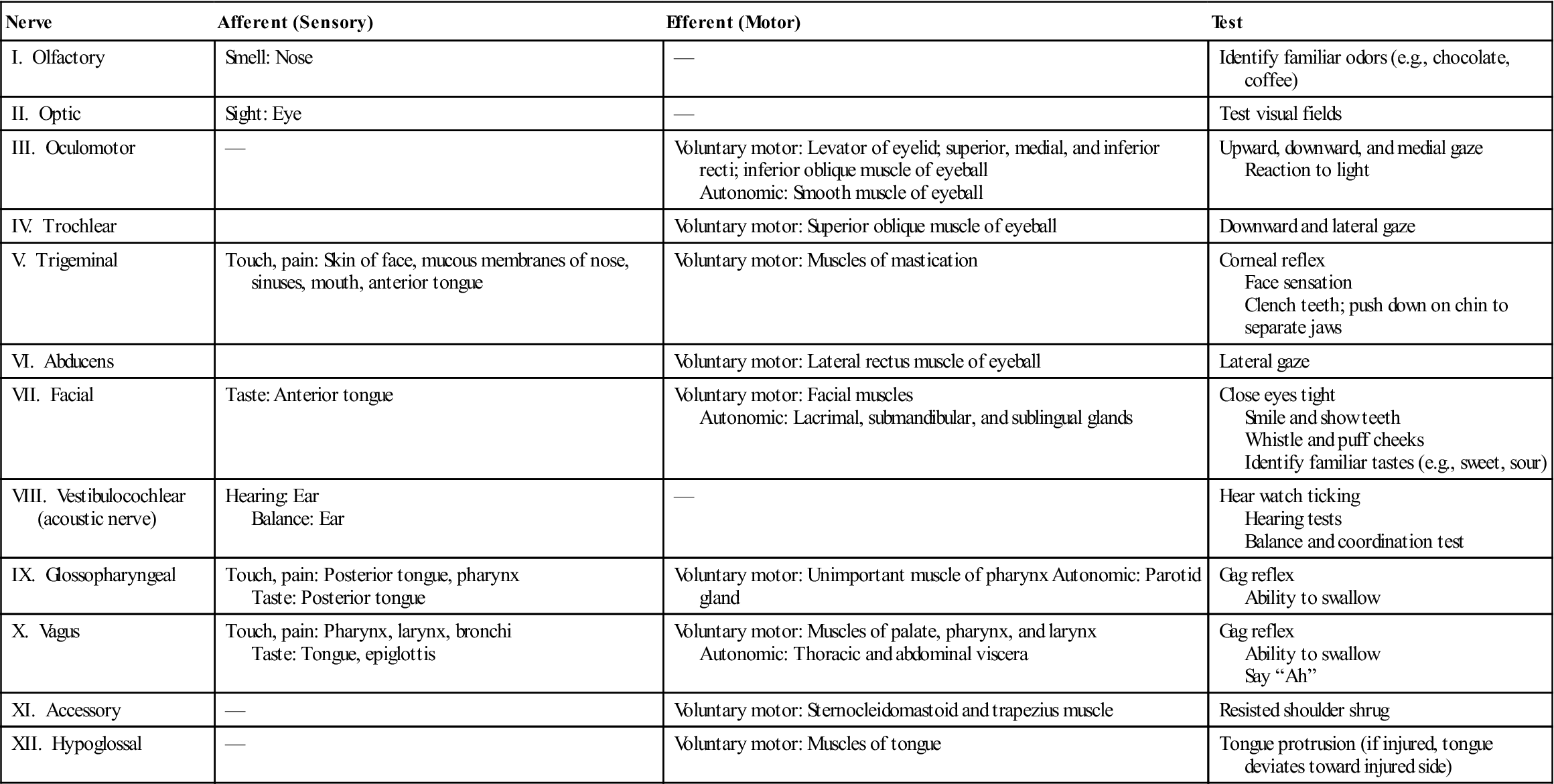
Adapted from Hollinshead WH, Jenkins DB: Functional anatomy of the limbs and back, Philadelphia, 1981, WB Saunders, p. 358; and Reid DC: Sports injury assessment and rehabilitation, New York, 1992, Churchill Livingstone, p. 860.
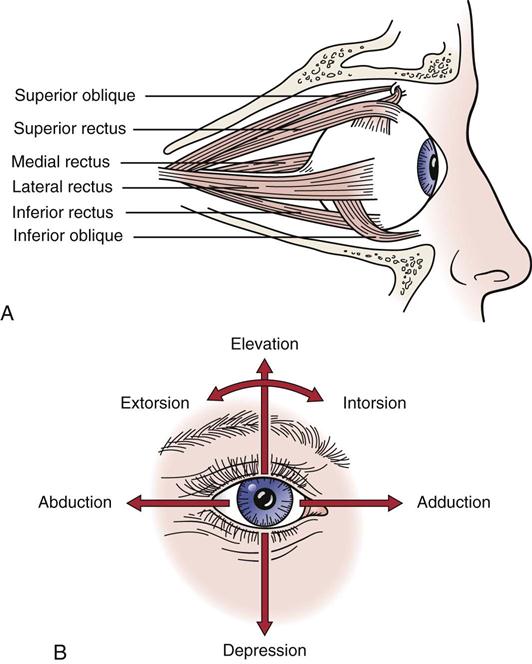
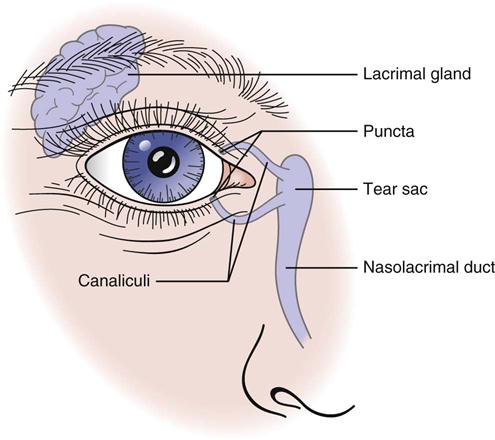
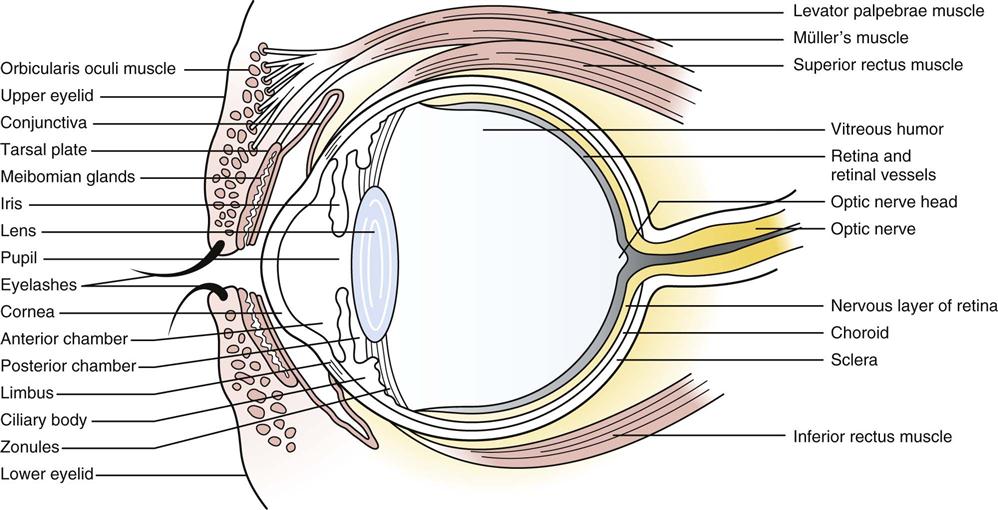
The external eye is composed of the eyelids (upper and lower), conjunctiva (a transparent membrane covering the cornea, iris, pupil, lens, and sclera), lacrimal gland, eye muscles, and bony skull orbit (Figure 2-3). Muscles of the eye, their actions, and their nerve supply are shown in Table 2-2. The muscles and movements of the eye are shown in Figure 2-4. To produce some of the actions, the various muscles of the eye must work in concert. The eyelids protect the eye from foreign bodies, distribute tears over the surface of the eye, and limit the amount of light entering the eye. The conjunctiva is a thin membrane covering the majority of the anterior surface of the eye. It helps to protect the eye from foreign bodies and desiccation (drying up). The lacrimal gland provides tears, which keep the eye moist (Figure 2-5). The eye itself is made up of the sclera, cornea, and iris as well as the lens and retina (Figure 2-6). The sclera is the dense white portion of the eye that physically supports the internal structures. The cornea is very sensitive to pain (e.g., the extreme pain that accompanies corneal abrasion) and separates the watery fluid of the anterior chamber of the eye from the external environment. It permits transmission of light through the lens to the retina. The iris is a circular, contractile muscular disc that controls the amount of light entering the eye and contains pigmented cells that give color to the eye. The lens is a crystalline structure located immediately behind the iris that permits images from varied distances to be focused on the retina. It is primarily the lens and its supporting ligaments that separate the eye into chambers: the anterior chamber (aqueous humor) and the posterior chamber (vitreous humor). Finally, the retina is the primary sensory structure of the eye that transforms light impulses into electrical impulses that are then transmitted by the optic nerve to the brain, which interprets the impulses as the objects seen.
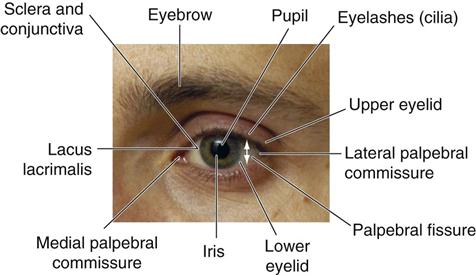
TABLE 2-2
Muscles of the Eye: Their Actions and Nerve Supply
| Action | Muscles Acting | Nerve Supply |
| Moves pupil upward | Superior rectus | Oculomotor (CN III) |
| Moves pupil downward | Inferior rectus | Oculomotor (CN III) |
| Moves pupil medially | Medial rectus | Oculomotor (CN III) |
| Moves pupil laterally | Lateral rectus | Abducens (CN VI) |
| Moves pupil downward and laterally | Superior oblique | Trochlear (CN IV) |
| Moves pupil upward and laterally | Inferior oblique | Oculomotor (CN III) |
| Elevates upper eyelid | Levator palpebrae superioris | Oculomotor (CN III) |
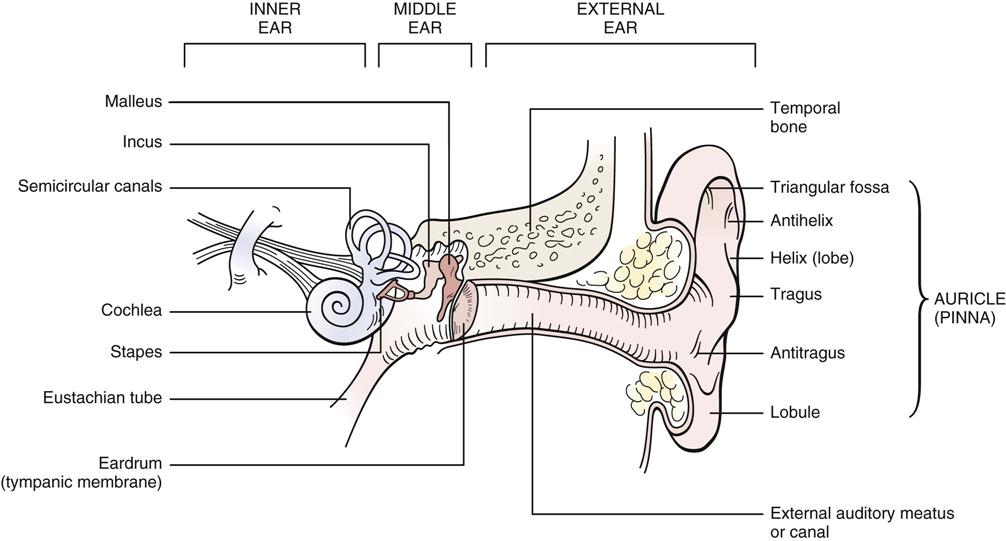
The external ear consists of cartilage covered with skin. Its primary purpose is to direct sound and to protect the external auditory meatus, through which sound is transmitted to the eardrum. The external ear, which is sometimes called the pinna, auricle, or trumpet, consists of the helix and lobule around the outside and the triangular fossa, antihelix, concha, tragus (a cartilaginous projection anterior to external auditory meatus), and antitragus on the inside (Figure 2-7). The middle ear structures consist of the tympanic membrane, or eardrum, which vibrates when sound hits it and sends vibrations through the ossicles—called the malleus (hammer), incus (anvil), and stapes (stirrup)—to the cochlea. The cochlea, which is part of the inner ear, transmits the sound waves to the vestibulocochlear nerve (cranial nerve VIII), which transmits electrical impulses to the brain for interpretation. The semicircular canals, the other part of the inner ear, play a significant role in maintaining balance.
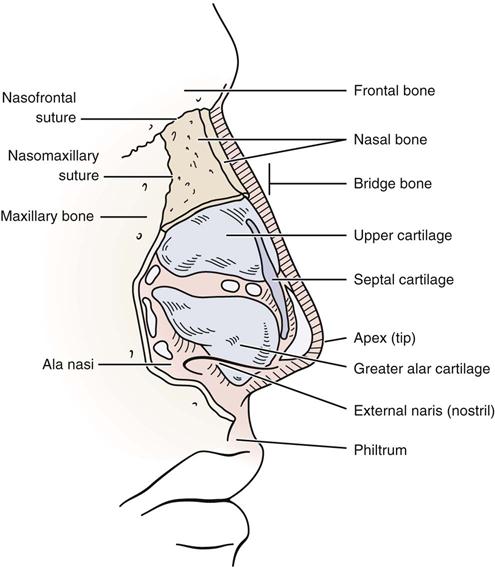
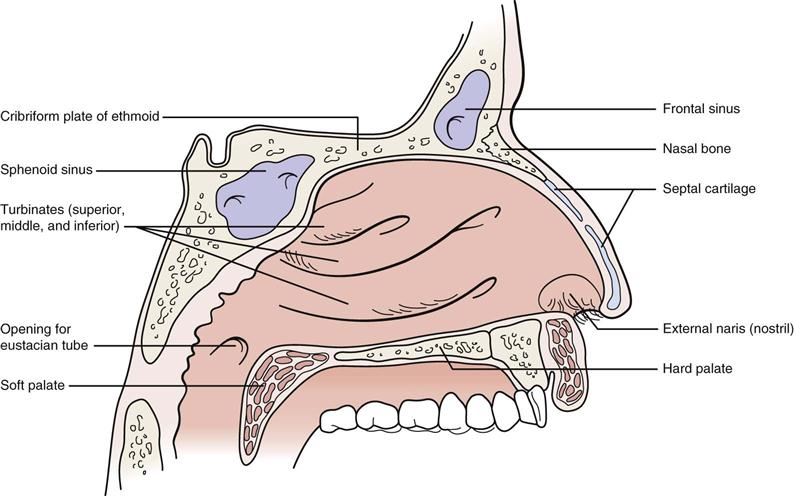
The external nose, like the external ear, consists primarily of cartilage covered with skin. However, its proximal portion contains bone covered with skin. Figure 2-8 shows the bone and cartilage makeup of the nose. The floor of the nose consists of the hard and soft palates and forms the roof of the mouth (Figure 2-9). Cartilage and the nasal, frontal, ethmoid, and sphenoid bones form the roof of the nose. The frontal and maxillary bones form the nasal bridge. Three bony structures called turbinates (superior, middle, and inferior) form the lateral aspects of the nose, which increase the surface area of the nose and thereby warm, humidify, and filter more of the inspired air. The nose is divided into two chambers (vestibules) by a septum. These chambers are lined with a mucous membrane containing hairs that collect debris and other foreign substances from the inspired air. The cribriform plate of the ethmoid bone contains the sensory fibers of the olfactory nerve (cranial nerve I) for smell.
Patient History
In addition to the questions listed under Patient History in Chapter 1, the examiner should obtain the following information from the patient who has sustained an injury to the head or the face:
1. What happened? This question determines the mechanism of injury and, potentially, the area of the brain or face injured (Table 2-3). A pathological classification for acute traumatic brain injuries is shown in the box on p. 89.1 A forceful blow to a resting, movable head usually produces maximum brain injury beneath the point of impact (Figure 2-10). This type of injury, called a coup injury, is usually caused by linear or translational acceleration.2 It often causes focal ischemic lesions, especially in the cerebellum, leading to alterations in smooth, coordinated movements, equilibrium, and posture. If the head is moving and strikes an unyielding object, such as the ground, maximum brain injury is usually sustained in an area opposite the site of impact.
This contrecoup injury is the result of impact deceleration. The injury occurs on the side of the head opposite to that receiving the blow, because the head is accelerating before impact, which squeezes the cerebrospinal fluid away from the trailing edge (the side away from the impact). The fluid moves toward the impact side, thereby thickening the cerebrospinal fluid and offering a cushioning effect at the point of impact. Because of the lack of cushioning on the trailing edge, greater injury is likely to occur to the brain on the side opposite the impact. The brain may also experience a “shaking” caused by repeated reverberation within the brain after the head has been struck. This type of injury often results in the signs and symptoms of a concussion with the degree of the concussion depending on the severity of the injury (Table 2-4). Concussion severity is only determined after signs and symptoms have disappeared and any neurological and cognitive testing is normal.3 If the cervical spine is taken beyond its normal range of motion, especially into rotation or side flexion, there may be a twisting of the cerebral hemisphere, brain stem, carotid artery, or carotid sinus that can result in injury to these structures or ischemia to the brain. Those areas of the brain that are most susceptible to damage include the temporal lobes, anterior frontal lobe, posterior occipital lobe, and upper portion of the midbrain.4
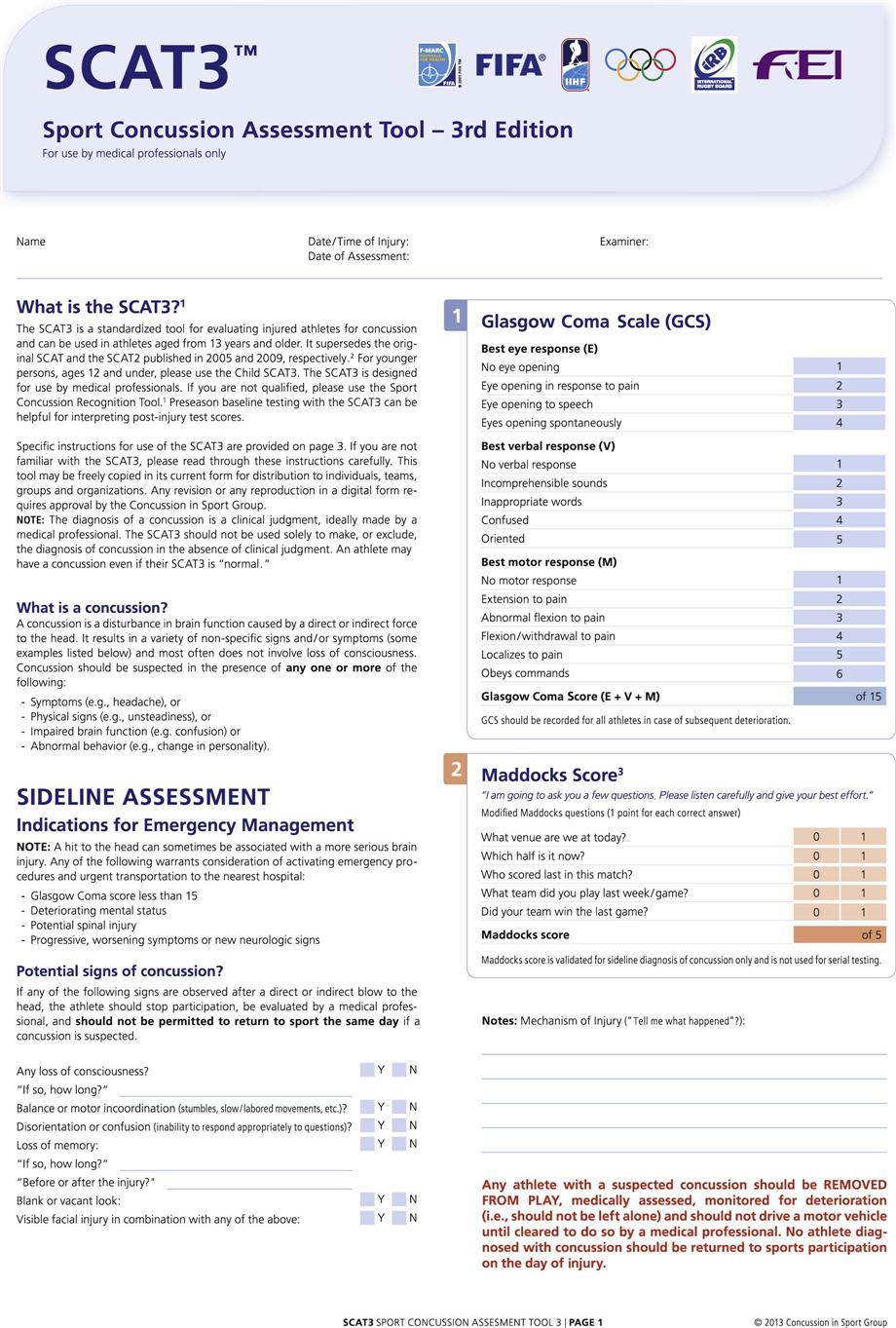
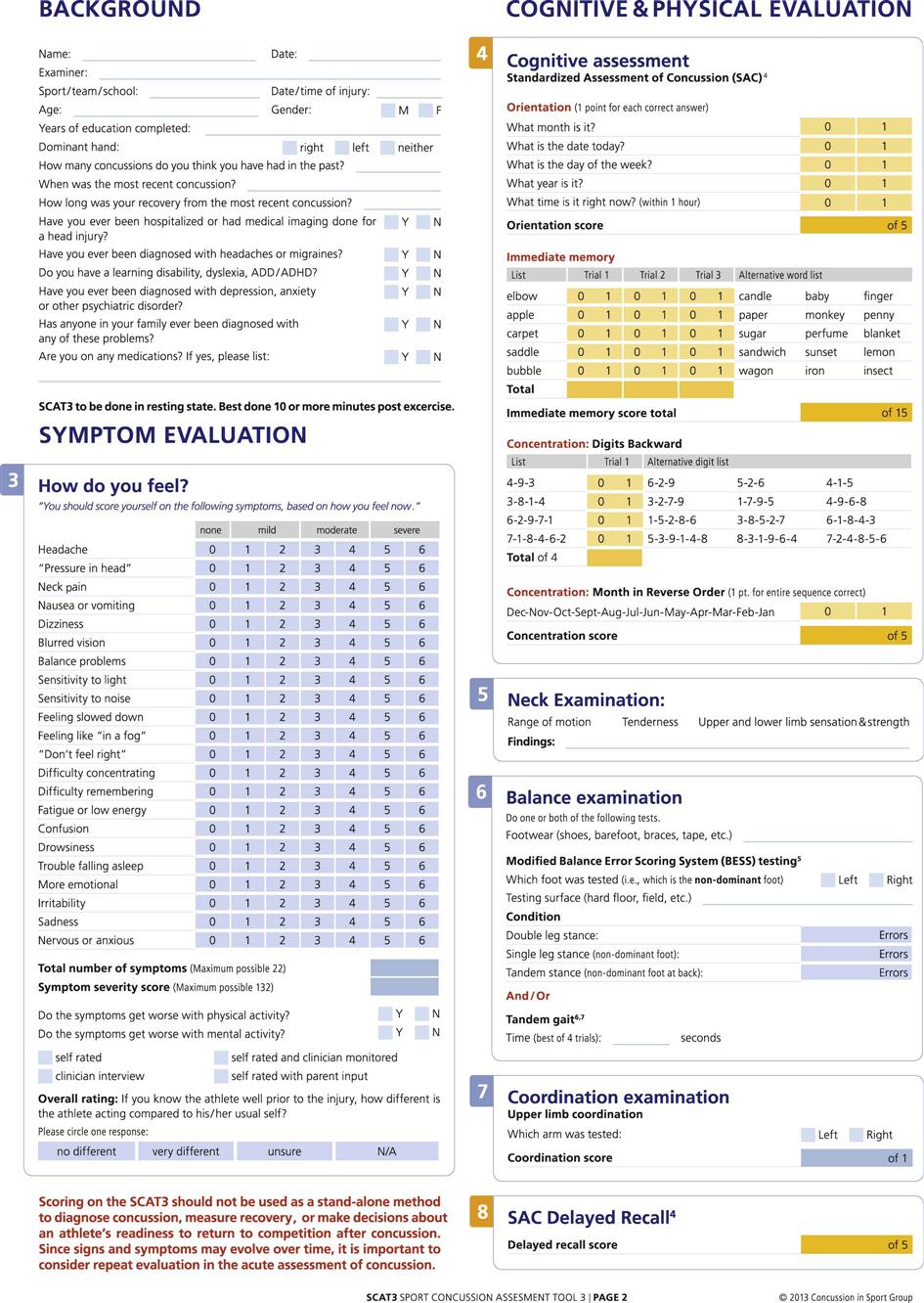
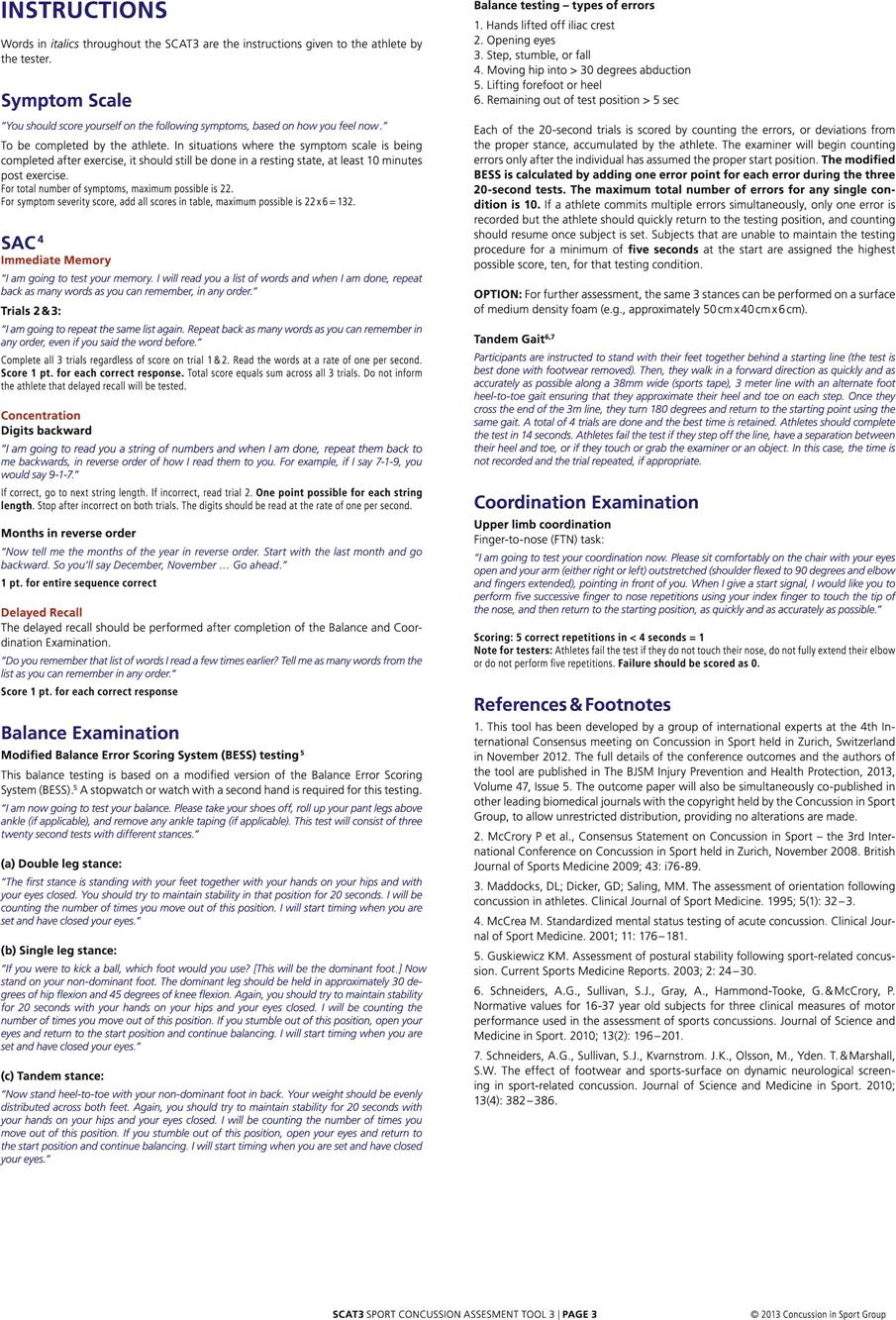
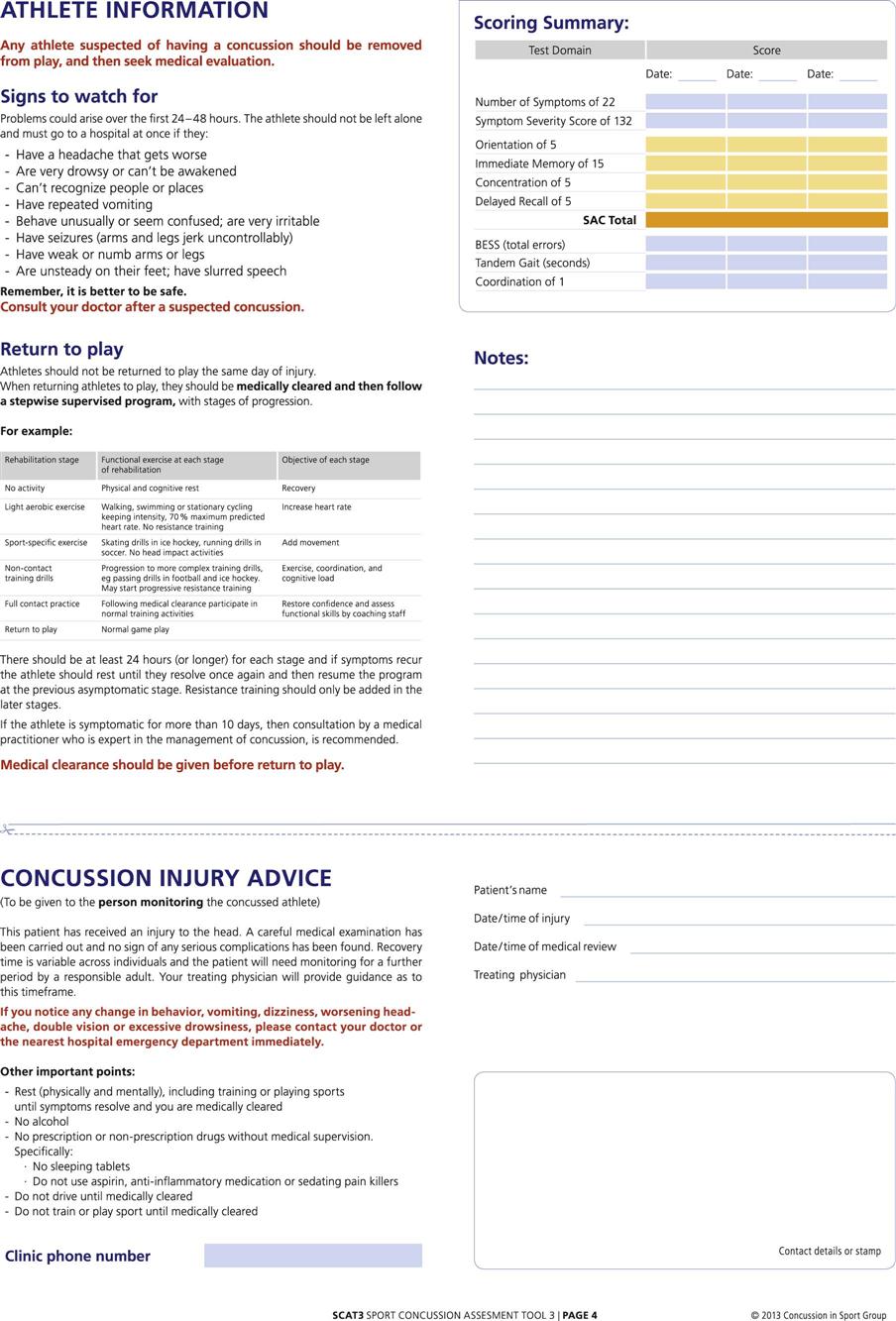
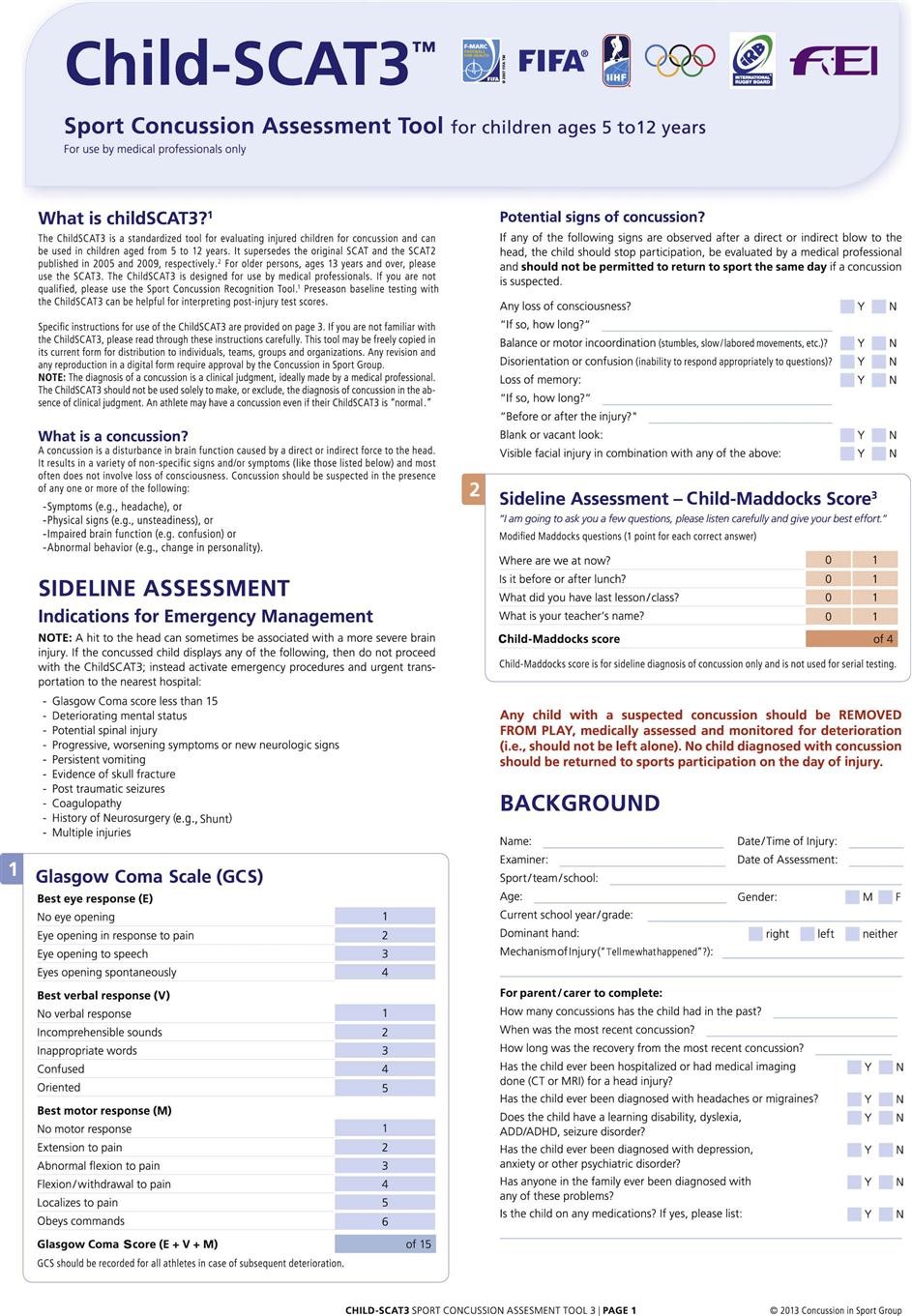
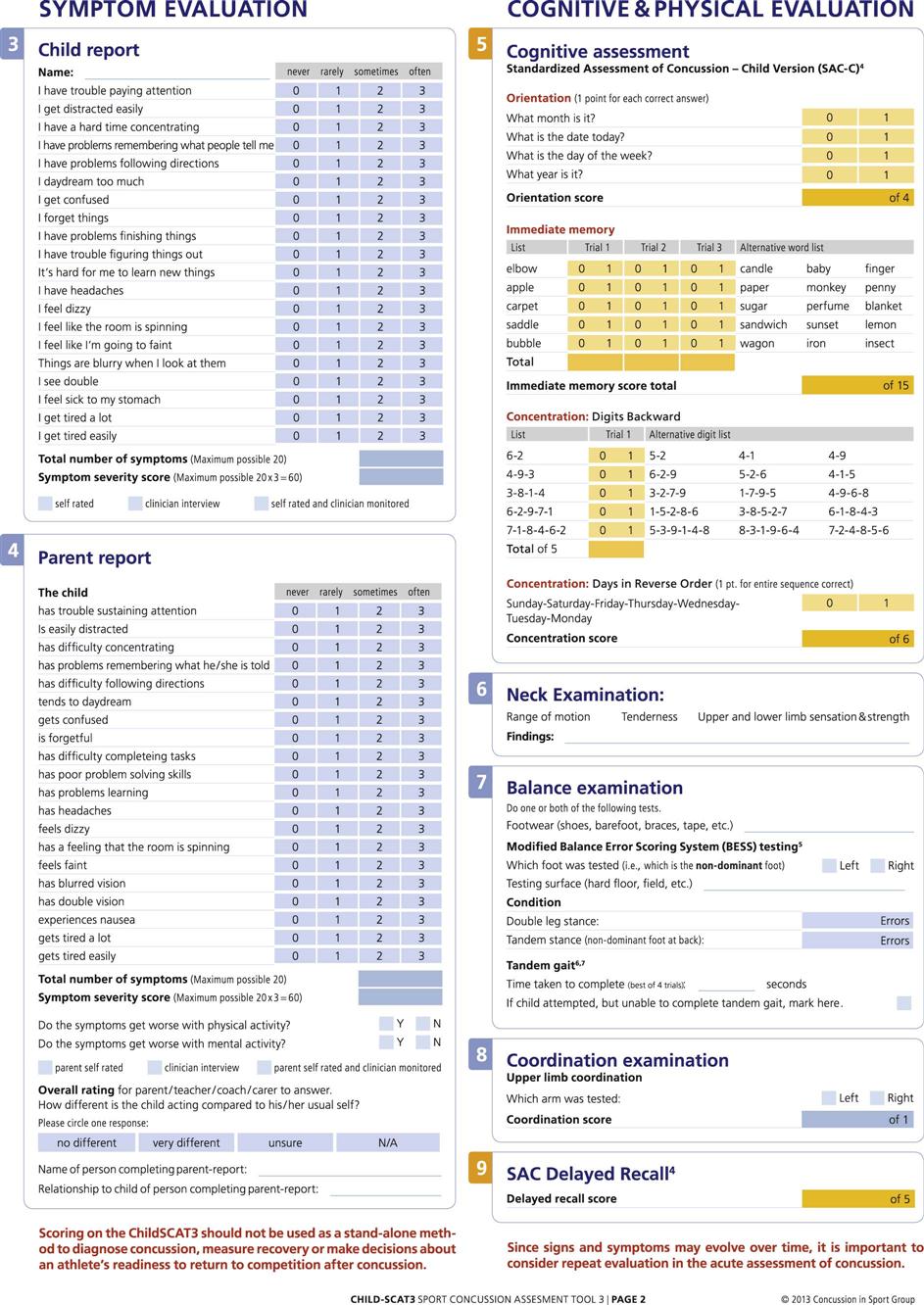
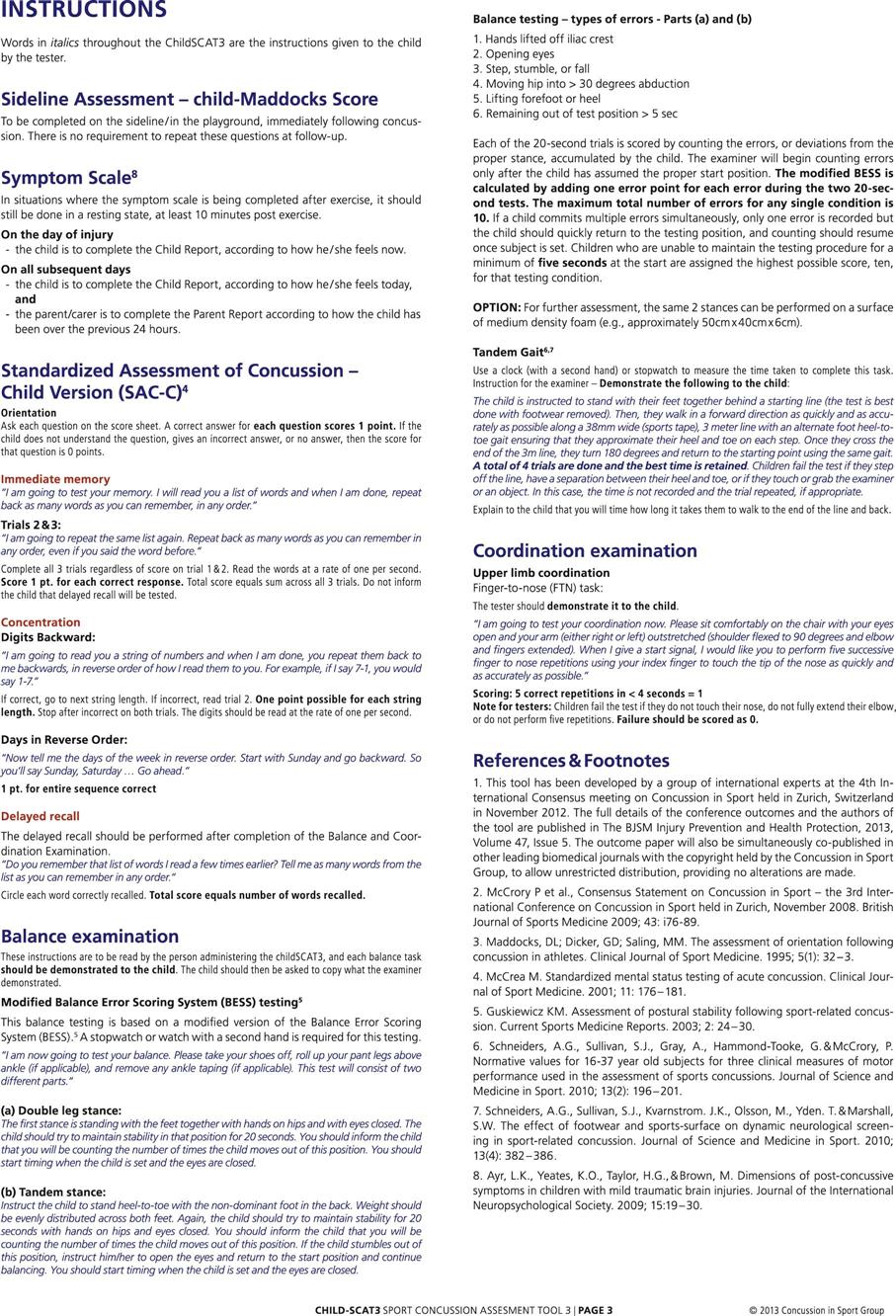
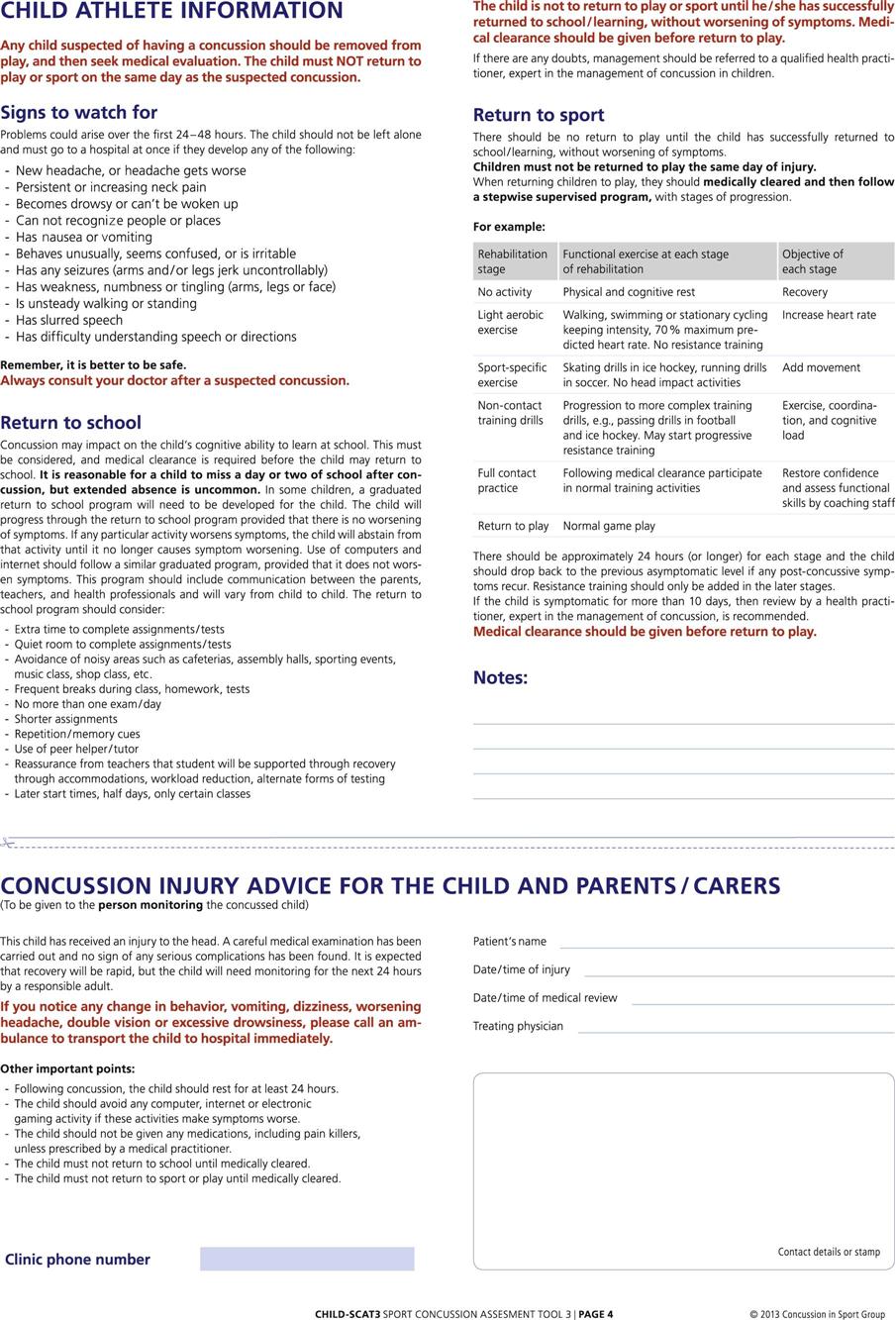
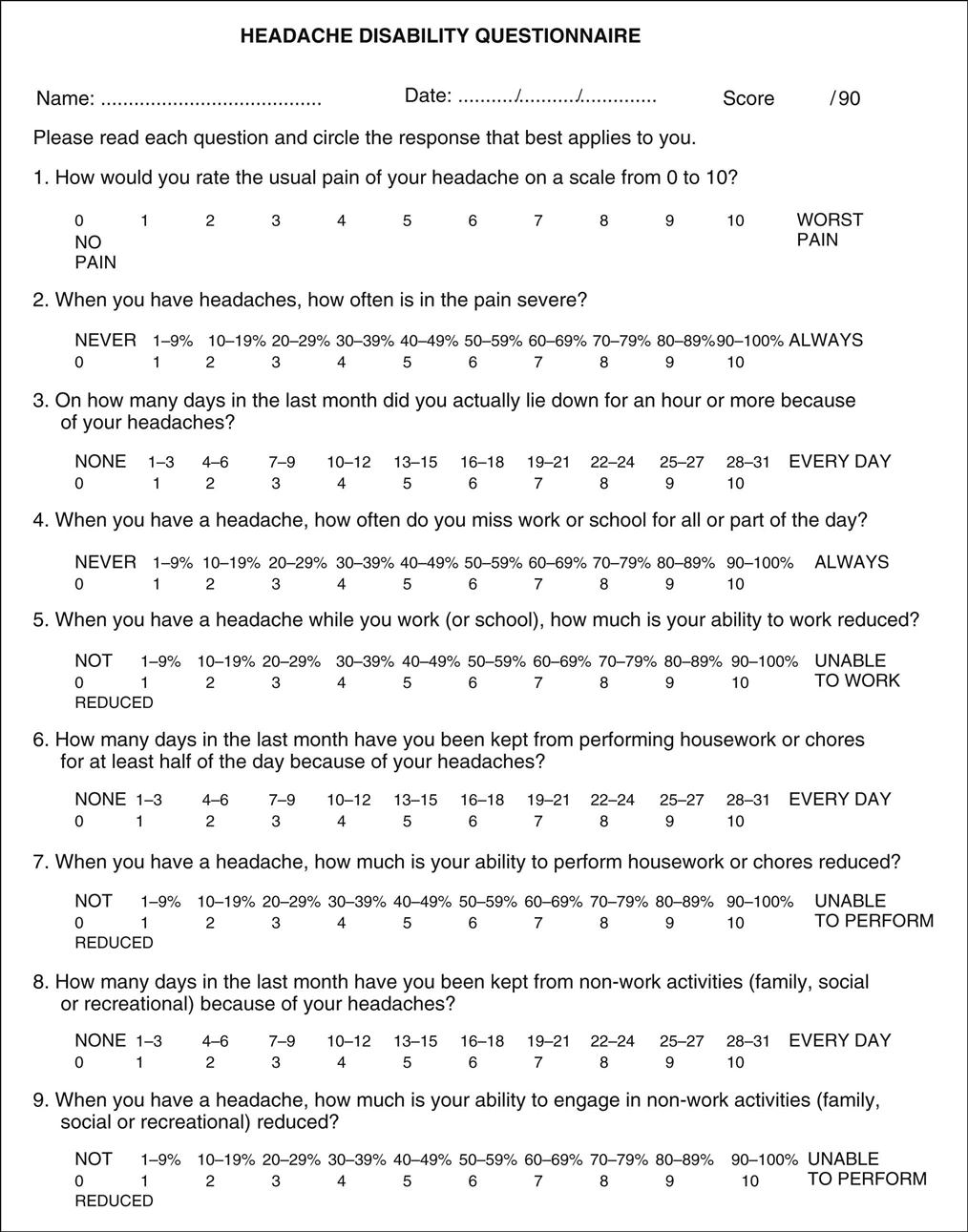
2. Did the patient lose consciousness? If so, how long was the patient unconscious? Has the patient suffered a concussion before? These questions are often difficult for the patient to answer or the examiner to know, because the patient may have been momentarily stunned and the time may have been so short that the patient believed there was no loss of consciousness. In other words, loss of consciousness may have been only momentary or, more traditionally, it may have lasted seconds to minutes. If the examiner is working with a sports team, accurate records are essential to record the severity (see later discussion) and the number of concussions suffered by the athlete and to ensure that proper care is instituted so that the athlete is not allowed to return to competition too soon. A concussion (a subset of mild traumatic brain injury) is a pathophysiological process that affects the brain and is caused by direct or indirect biomechanical forces. At present, there is no known threshold for a consussion.5–8 Risk factors are shown in Table 2-5,9 and stages of concussion are shown in Table 2-6.10 Signs and symptoms of concussions are shown in Table 2-7.11–13 Women appear to be more susceptible to concussions than men,14 and traumatic brain injury is different in children than adults.9,15,16 Concussions can result from a blow to the head or jaw or a fall on the buttocks from a height and can result in an inability to process information. Their effect is cumulative, and the risk of having another concussion following an initial concussion is four to six times greater than someone who has not had a concussion.12,17 Concussions can lead to continued and severe problems (e.g., post-concussion syndrome, second-impact syndrome).10,12,17–20 To be maximally effective, athletes should have done baseline tests in their pre-participation evaluation and have an extensive concussion history taken covering somatic, neurobehavioral, and cognitive symptoms (Table 2-8).3,12,21–26 In 2012, the International Conference on Concussion in Sport updated a Sideline Concussion Assessment Tool—3rd edition (SCAT3) (Figure 2-11) and added the Sport Concussion Assessment Tool for children ages 5 to 12 years (Child-SCAT3)8 (Figure 2-12). Kelly and Rosenberg12,13 have developed a Standardized Assessment of Concussion (SAC) (Figure 2-13),27,28 which provides a concise evaluation method for concussion by including measures of orientation, immediate memory, concentration, delayed recall, and other parameters. Lovell and Burke have developed a similar form for ice hockey.29
These tests are often combined with computerized neurocognitive testing to try to predict how long recovery will take.30,31 Ideally, this neurocognitive testing should be done individually at preseason evaluations to establish a baseline and should be updated every 2 years.32,33 If pre-injury values are not available, normative data may be used.34 An example of such a computerized post-concussion assessment is the ImPACT test; ImPACT stands for Immediate Post-Concussion Assessment and Cognitive Testing.31,32,35–37
There are several different grading systems for concussions (Table 2-9). It should be pointed out, however, that the International Conference on Concussion in Sport3 recommended that grade scales be abandoned, because concussion severity can only be determined retrospectively after all signs and symptoms have cleared, the neurological examination is normal, and cognitive function has returned to normal.38 The conference group felt concussions should be grouped as simple or complex. Simple concussion implies that the injury resolves over 7 to 10 days without complications. Neurophysiological screening does not play a role, but mental status screening is part of the assessment. Complex concussions are those in which persistent symptoms and specific sequelae (i.e., convulsions, loss of consciousness for longer than 1 minute, prolonged cognitive impairment) occur.3 This includes people with more than one concussion. In this case, neurophysiological testing does play a role.13,39–42 Table 2-10 shows some neurophysiological tests that could be used for post-concussion assessment.
Grades of concussion, such as those advocated by Torg (see later discussion and Table 2-4), can play a role in the acute phase but should be used with caution if making return to activity decisions.43 With each grade, the signs and symptoms worsen, and the sequelae are more evident. No signs and symptoms under exertion (i.e., simulating the activity the person will return to) should be evident, even with simple concussions.
With a grade I concussion, the patient is slightly confused and may have a dazed look. The patient is completely lucid within 5 to 15 minutes; has no amnesia, sequelae, or residual symptoms; and has had no loss of consciousness. Some people refer to the grade I concussion as the patient’s having his or her “bell rung.”
With a grade II concussion, there is slight confusion, and posttraumatic amnesia becomes evident. Posttraumatic (anterograde) amnesia is the loss of memory for events occurring immediately after wakening or from the moment of injury. Posttraumatic amnesia is considered to be the length of time from injury until conscious memory returns. In the acute state, it may take time for posttraumatic amnesia to become obvious. Sometimes, the patient will remember what happened immediately after the injury, but as time goes on (up to 1 to 2 hours after the injury), posttraumatic amnesia becomes evident. This is one of the reasons it is advisable to reassess acute head injuries every 15 to 30 minutes. Manzi and Weaver reported that a patient who had sustained a period of posttraumatic amnesia of less than 60 minutes was considered to have sustained a mild head injury.44 If the period of posttraumatic amnesia lasted from 1 to 24 hours, moderate head injury was considered to have occurred. If the posttraumatic amnesia lasted for more than 1 week, the patient was considered to have sustained a serious head injury. If the duration of the posttraumatic amnesia was more than 7 days, full return to neurological function was highly unlikely.44 With a grade II concussion, the patient may experience mild tinnitus (ringing in the ears), mild dizziness, and a dull headache with some disorientation. Dizziness at the time of injury has been reported to be a sign of risk for protracted recovery.45 The patient who experienced a grade II concussion may also develop a post-concussion syndrome (i.e., have continual neurological problems after the concussion), which is observed in about 10% of concussion cases. The signs and symptoms of this syndrome include persistent headaches, especially with exertion; inability to concentrate; and irritability. The symptoms may last from several weeks to several years.
A patient with a grade III concussion has the same symptoms as someone with a grade II concussion and also experiences retrograde amnesia. Retrograde amnesia is loss of memory of events that occurred before the injury. It may take 5 to 10 minutes for retrograde amnesia to develop after the concussion, and amnesia may involve only a few minutes before the injury. For this reason, the patient should be questioned frequently about what happened before the injury occurred and how it occurred, to see if there is any change in the patient’s memory pattern. There is always some degree of permanent retrograde amnesia with these patients.
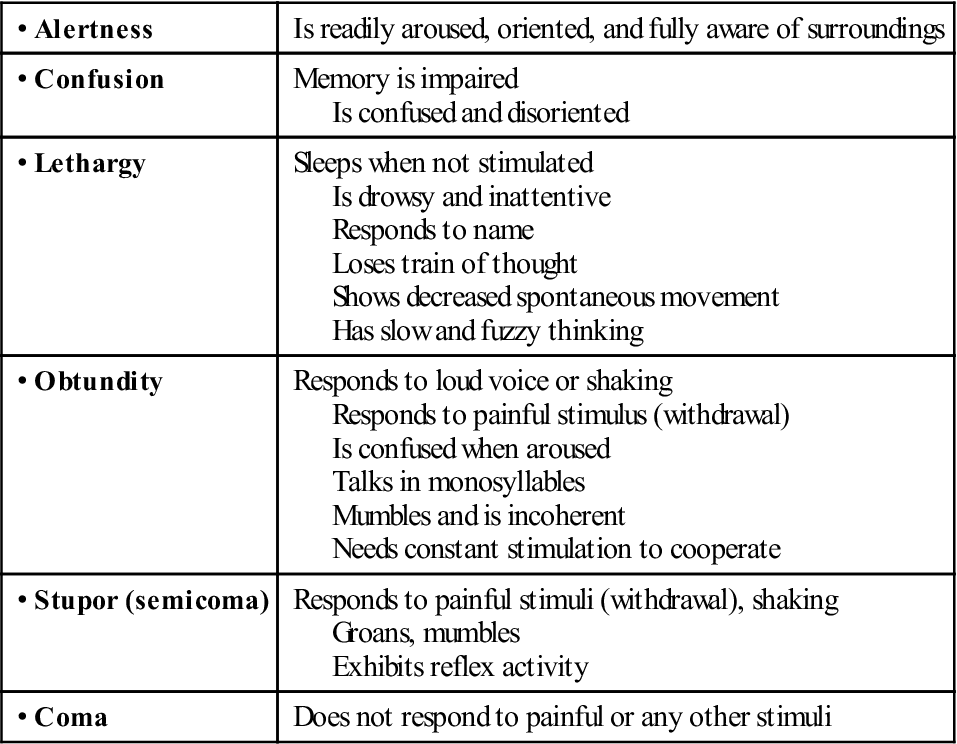
With a grade IV concussion, the patient loses consciousness for 5 minutes or less. The level of consciousness may vary; the patient may be comatose, stuporous, obtunded, lethargic, confused, or fully alert. The patient goes through the following stages of recovery: unconsciousness (also called paralytic coma), stupor, obtundity, lethargy, confusion (with or without delirium), near lucidity with automatism, and finally full alertness. Stupor implies that the patient is only partially conscious and has reduced responsiveness. Obtundity implies the patient has reduced sensitivity to painful or unpleasant stimuli. Lethargy implies a state of sluggishness, dullness, or serious drowsiness. Confusion implies that the patient is disoriented in terms of time, place, or person. Delirium means that the patient may experience illusions, hallucinations, restlessness, or incoherence. Lucidity with automatism implies that the patient appears to be alert and fully recovered but acts only mechanically and is not really aware of what he or she is doing. With a grade IV concussion, there may be subtle changes in the patient’s personality and memory function. Both retrograde and posttraumatic amnesia are evident, and the patient demonstrates mental confusion and complains of tinnitus and dizziness to a greater degree than is seen with a grade III concussion. The patient also has residual headaches and is unsteady for 5 to 10 minutes after regaining consciousness. The literature has reported that loss of consciousness, by itself, is not a good predictor of the degree of neurophysiological loss or damage with a head injury.46 The severity of the head injury is best determined by the administration of different neurophysiological tests (e.g., GOAT test,47 Hopkins Verbal Learning Test,48 Trail Making Test, Wisconsin Card Sorting Test, Digit Symbol Substitution Test [DSST],49 and measures of decision time49) as well as considering all signs and symptoms the patient demonstrates.6,8,15,50–53 To ensure adequate data, however, these tests must also have been administered before the injury (e.g., in a pre-participation evaluation in sports).6,35
With a grade V concussion, the patient has experienced a paralytic coma or unconsciousness for 5 minutes or longer. This grade of concussion involves bruising of the brain, and there is prolonged retrograde amnesia as well as posttraumatic amnesia. The patient complains of severe tinnitus, unsteadiness for longer than 10 minutes, blurred vision, poor light accommodation, and a headache that feels “different” from most headaches. Both the autonomic and the peripheral nervous systems can be affected through their control by the brain. These patients may also experience nausea, vomiting, and sometimes convulsions. The recovery after a grade V concussion may be one of two types. In type A, the patient goes from a paralytic coma through stupor, confusion, lucidity, and full alertness, which is similar to a grade IV concussion but more severe. The individual with a type B grade V concussion experiences a paralytic coma that is associated with secondary cardiorespiratory collapse and is of much greater concern to the examiner, especially during the initial assessment, when the body’s essential functions must be maintained.
More severe diffuse brain injuries are associated with more severe neurological dysfunction. With these injuries, loss of consciousness lasts for more than 24 hours, and recovery is never complete, leading to deficits in intelligence, reasoning, and memory and to changes in personality. Shearing brain injuries tend to be more severe than diffuse brain injuries and lead to abnormal brain stem signs, such as decerebrate rigidity.43
5. What type of pain is the patient experiencing? The type of pain indicates the type of structure injured (see Table 1-3).
7. What activities aggravate the particular problem?
8. What activities ease the particular problem?
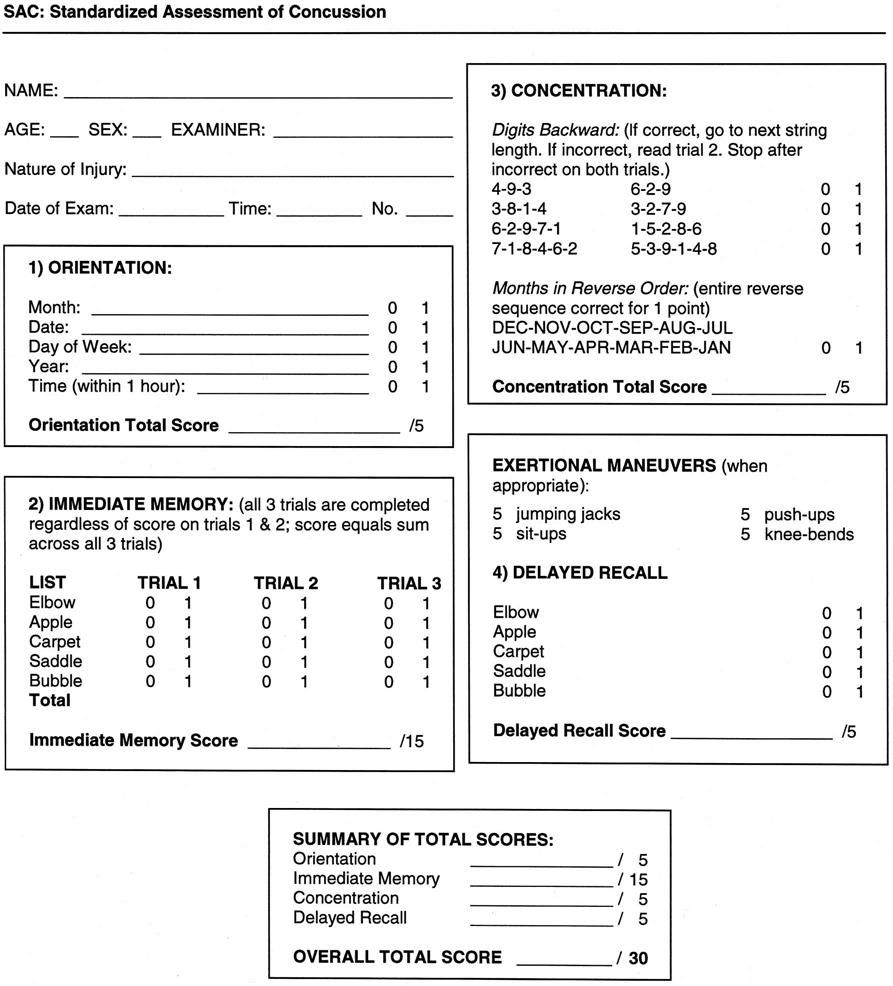
9. Does the patient have a headache, and, if so, where (Tables 2-11 and 2-12)? Is the headache tolerable? What type of headache is it? Is it a throbbing, pounding, boring, shocklike, dull, nagging, or constant-pressure type of headache? Is the pain of the headache aggravated by movement or by rest? What is the exact location of the headache? Is the headache affected by position or time of day (Table 2-13)? Does it cover the entire head, the sinus region, or behind the eyes? Does it present a “hat band” distribution, or does it affect the neck or the occiput area? It is important for the examiner to record the location, character, duration, and frequency of the headache, as well as any factors that appear to either aggravate or relieve the pain so that a diagnosis can be made and any changes can be noted (Table 2-14). Figure 2-14 shows a headache disability questionnaire that may be used to determine the severity of headache and its effect on everyday activity.54
13. Does the patient have any memory of past events or what occurred before or after the injury? This type of question tests for retrograde amnesia, posttraumatic amnesia, and injury severity, which can be determined by asking the patient straightforward questions about events in the patient’s own past, such as birth date or year of graduation from high school or university. The examiner may also ask questions about the injury, preceding events, and posttraumatic events. Questions such as “What day is it?” “Who is the opposition?” “Who is winning?” and “What is your telephone number and address?” test the patient’s static memory ability. The examiner must ensure that he or she or someone present at the time of the examination knows the answer to these questions. Although it is common to ask these orientation questions (e.g., time, place), it has been shown that these questions can be unreliable in sporting situations when compared with memory assessment.55,56 The examiner can assess recent memory by asking the patient to remember the names for two to five persons or common objects, such as the color “red,” the number “five,” the name “Mr. Smith,” and the word “pride,” and then asking the patient to name them 5 or 10 minutes later. The patient may be asked to repeat the words two or three times when the examiner initially says them to test immediate recall or to ensure that the patient can say and recall the words. Immediate recall, another form of memory, is best tested by asking the patient to repeat a series of single digits. Normally, a person can repeat at least six digits, and many people can repeat eight or nine. The examiner may also ask the patient to repeat the months of the year backward in a similar type of test. Memory is generally thought to be formed and stored in certain regions of the temporal lobes. The parietal lobe of the brain is thought to enable one to appreciate the environment, to interpret visual stimuli, and to communicate.
14. Can the patient solve simple problems? Because concussions reduce one’s ability to process information, it is important to determine the patient’s reasoning and processing ability. For example, does the patient know his or her home telephone number? Is the patient able to do the “minus 7” or “serial 7” test (i.e., count backward from 100 by sevens)? This test gives the examiner some idea of the patient’s calculating ability and concentration skills. Mathematic ability (the ability to add, subtract, multiply, and divide) can also be evaluated to test processing ability. In addition, the examiner can ask the patient to name several important people from the present in reverse chronological order (e.g., the last three presidents of the United States) or to give the names of some familiar capital cities. Finally, the patient should be tested on his or her ability to comprehend abstract relations. For example, the examiner may quote a common proverb, such as “A bird in the hand is worth two in the bush,” and then ask the patient to explain what the expression means. Patients with organic mental impairment and certain patients with schizophrenia may give a concrete answer, failing to recognize the abstract principle involved.44 The ability to conceptualize, abstract, plan ahead, and formulate rational judgments of problems or events is largely a function of the frontal lobes.
17. Is the patient having any problems with the eyes? Monocular diplopia (blurred vision when looking with one eye) may result from hyphema, a detached lens, or other trauma to the globe of the eye.57 Binocular diplopia (blurred vision when looking through both eyes) occurs in 10% to 40% of patients with a zygoma fracture. It may be caused by soft-tissue entrapment, neuromuscular injury (intraorbital or intramuscular), hemorrhage, or edema. It disappears when one eye is closed. Double vision, which occurs when the good eye is closed, indicates that some structure of the eye is injured. If it occurs with both eyes open, something is affecting the free movement of the eyes (Tables 2-15 and 2-16).
21. If the examiner is concerned about the mouth and teeth or the temporomandibular joints, questions related to these areas can be found in Chapter 4. It is important, however, to ensure that the patient’s dental occlusion and biting alignment have not been altered. Are all the teeth present, and are they symmetrical? Is there any swelling or bleeding around the teeth? Are the teeth mobile, or is part of a tooth missing? Is the pulp exposed? Each of these questions helps determine whether the teeth have been injured. Teeth that have been avulsed, if intact, should be reimplanted as quickly as possible. If reimplanted after cleansing (rinsed in saline solution or water) within less than 30 minutes, the tooth has a 90% chance of being retained. If it is not possible to reimplant the tooth, it should be kept moist in saline, or the patient should keep it between the gum and cheek while dental care is sought.
22. Questions concerning the neck and cervical spine can be found in Chapter 3.
TABLE 2-3
Areas of the Brain and Their Function
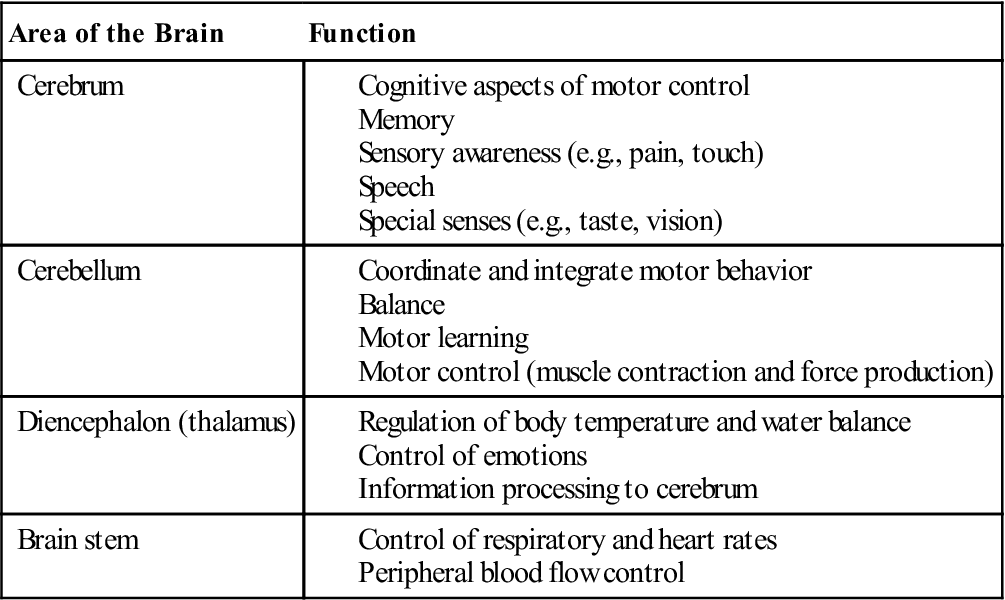
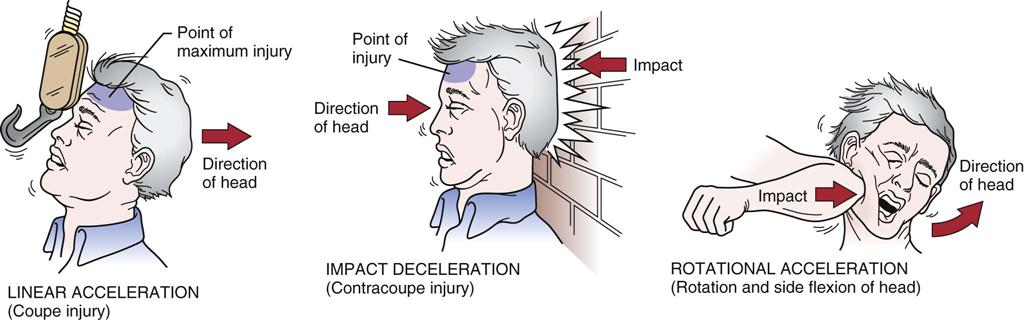
TABLE 2-4
Signs and Symptoms* of Concussion (Torg Classification)
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | |
| Confusion | None or momentary | Slight | Moderate | Severe | Severe |
| Amnesia | No | Posttraumatic amnesia <30 min | Posttraumatic amnesia <30 min Retrograde amnesia |
Posttraumatic amnesia >30 min Retrograde amnesia |
Posttraumatic amnesia >24 hours Retrograde anmesia |
| Residual symptoms | No | Perhaps | Sometimes | Yes | Yes |
| Loss of consciousness | No | No | No | Yes (<5 min) | Yes (>5 min) |
| Tinnitus | No | Mild | Moderate | Severe | Often severe |
| Dizziness | No | Mild | Moderate | Severe | Usually severe |
| Headache | No | May be present (dull) | Often | Often | Often |
| Disorientation and unsteadiness | None or minimal | Some | Moderate | Severe (5 to 10 min) | Often severe (>10 min) |
| Blurred vision | No | No | No | Not usually | Possible |
| Post-concussion syndrome | No | Possible | Possible | Possible | Possible |
| Personality changes | No | No | No | Possible | Possible |
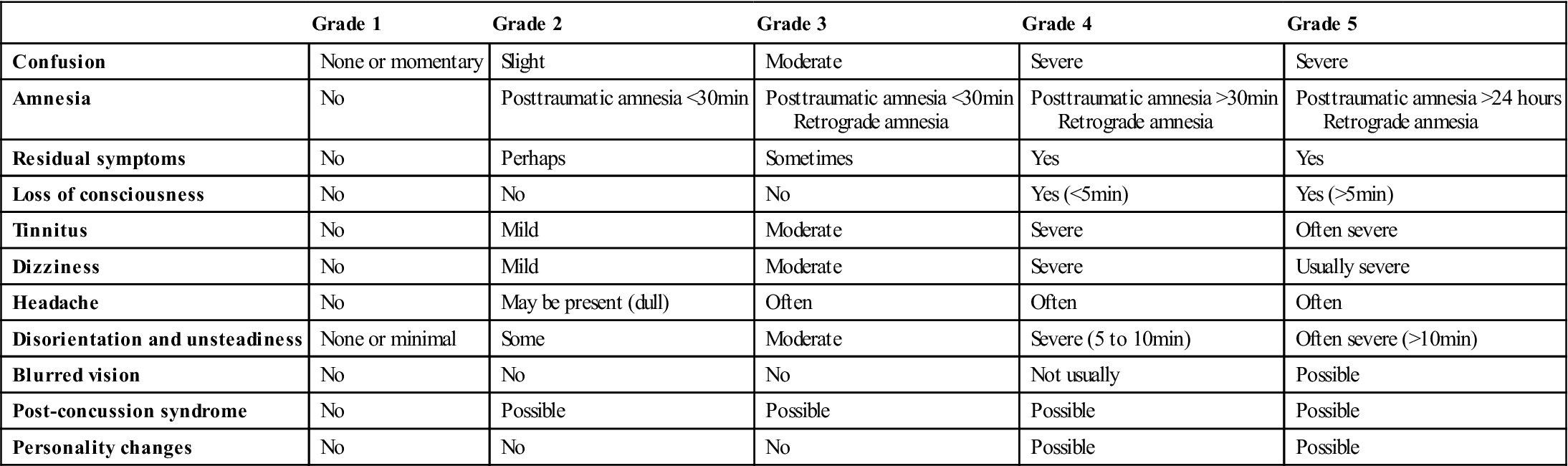
*These signs and symptoms should only be used as a guide in acute situations.
Data from Vegso JJ, Torg JS: Field evaluation and management of intracranial injuries. In Torg JS, editor: Athletic injuries to the head, neck and face, St Louis, 1991, Mosby, pp. 226–227.
TABLE 2-5
Risk Factors That May Prolong or Complicate Recovery from Concussion
| Factors | Modifier |
| Symptoms | |
| Signs | |
| Sequelae | |
| Temporal | |
| Threshold | |
| Age | |
| Co- and pre-morbidities | |
| Medication | |
| Behavior | |
| Sport |
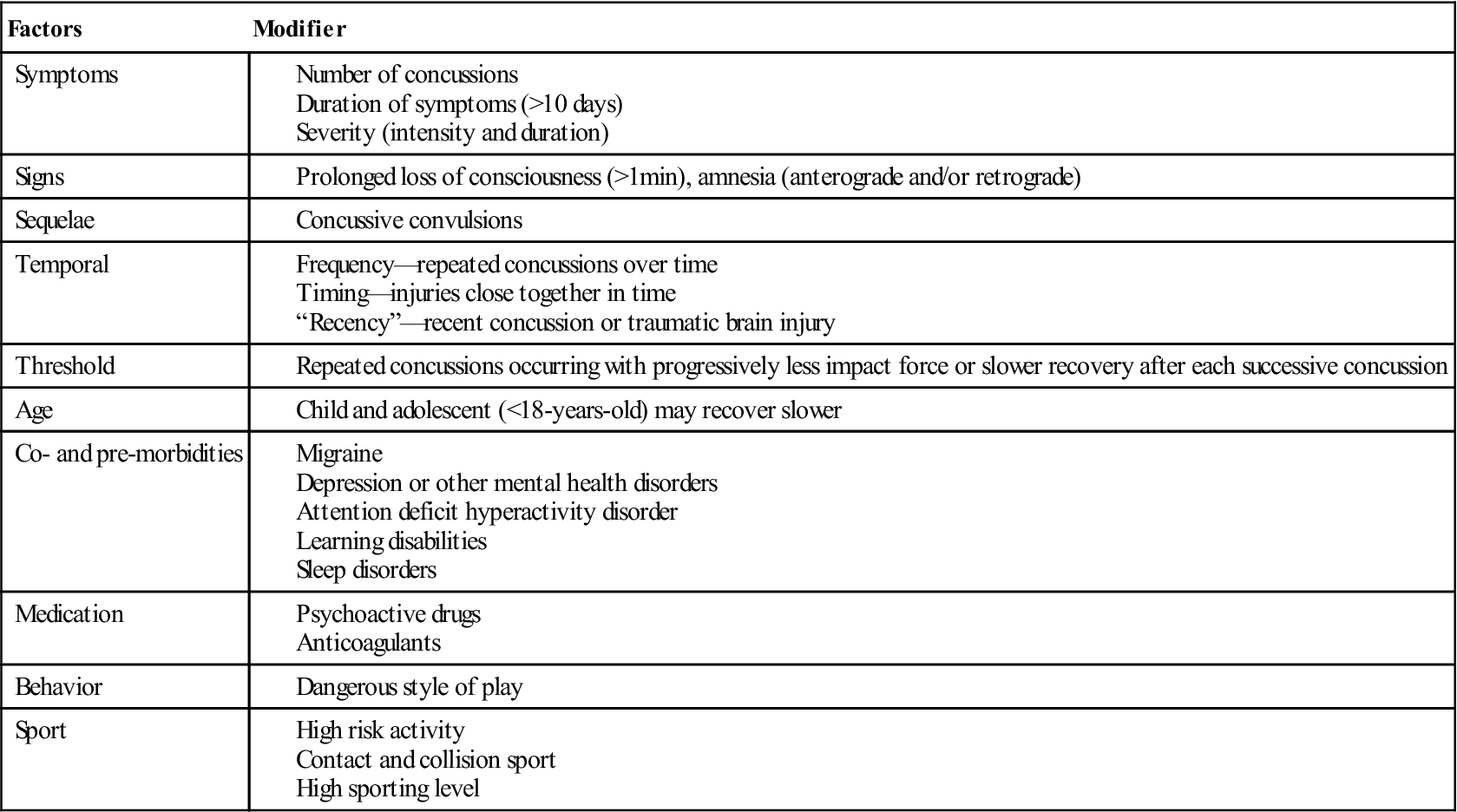
Modified from McCrory P, Meeuwisse W, Johnston K, et al: Consensus statement on concussion in sport—The 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med 19(3):189, 2009.
TABLE 2-6
Severity Stages of Concussive Injury
| Acute Concussion | Post-Concussion Syndrome | Prolonged Post-Concussion Syndrome | Chronic Traumatic Encephalopathy |
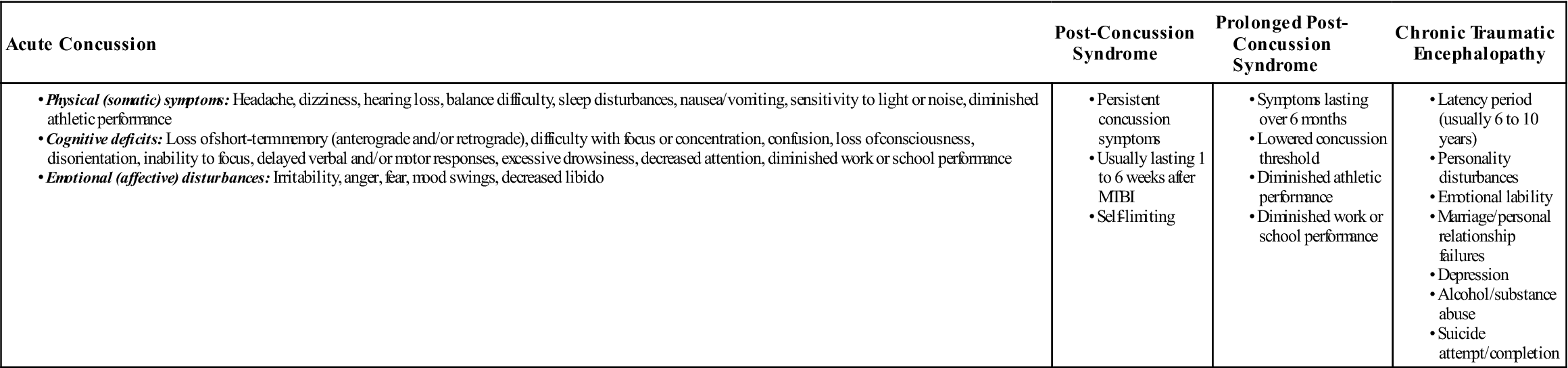
MTBI, Mild traumatic brain injury.
Modified from Sedney CL, Orphanos J, Bailes JE: When to consider retiring an athlete after sports-related concussion. Clin Sports Med 30(1):189–200, 2011.
TABLE 2-7
Signs and Symptoms of Concussions
| Acute | Late (Delayed) |
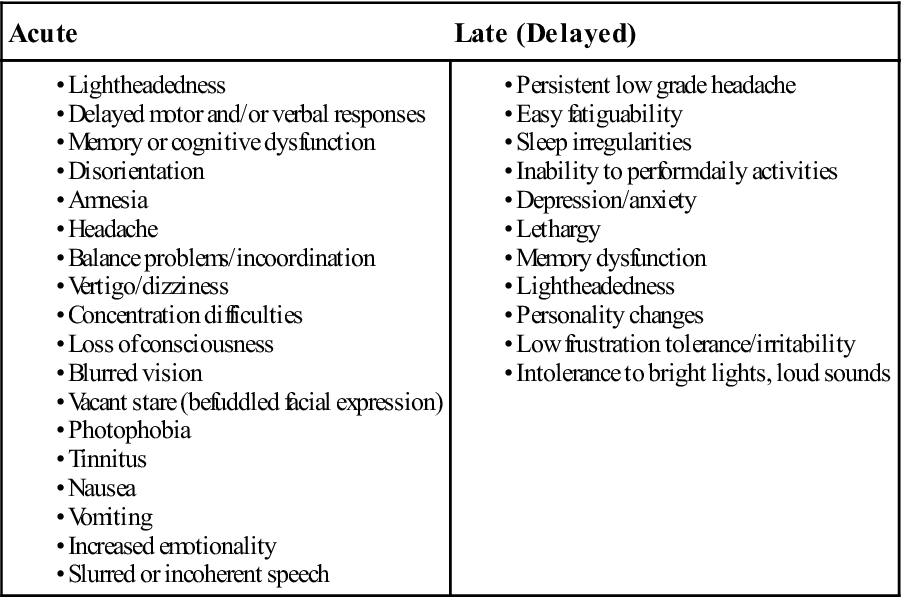
TABLE 2-8
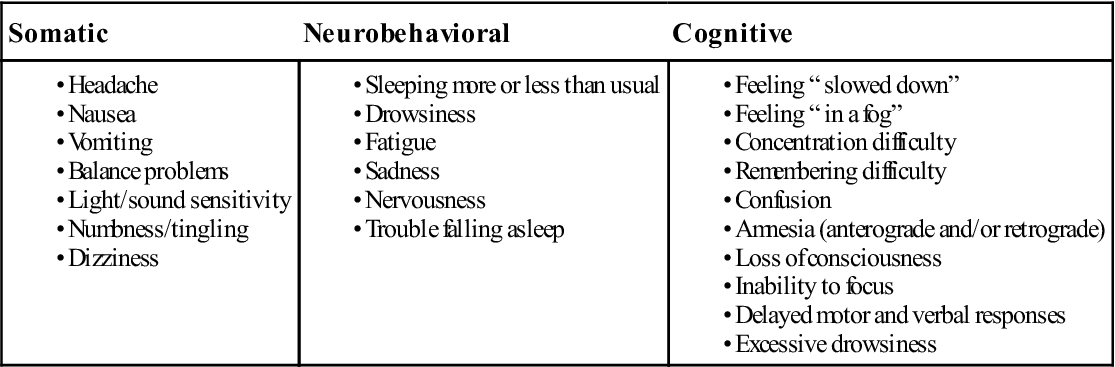
Data from Piland SG, Motl RW, Guskiewicz KM, et al: Structural validity of a self-report concussion-related symptoms scale, Med Sci Sports Exerc 38(1):27–32, 2006; Herring SA, Cantu RC, Guskiewicz KM, et al: Concussion (mild traumatic brain injury) and the team physician: a consensus statement—2011 update. Med Sci Sports Exerc 43(12):2414, 2011.
TABLE 2-9
Classification Systems for Concussions
| System | Grade I (Mild) | Grade Ia | Grade II (Moderate) | Grade III (Severe) | Grade IV |
| Cantu | No LOC or PTA < 30 min | N/A | LOC < 5 min, PTA 30 min to 24 hrs | LOC > 5 min, PTA > 24 hrs | N/A |
| Torg | (Grade I to II) No LOC or amnesia (except PTA) | (Grade III–IV) LOC < few minutes, PTA or retrograde amnesia |
(Grade V–VI) LOC/coma, confusion, amnesia |
||
| Colorado Consortium | Confusion without amnesia, no LOC | N/A | Confusion and amnesia, no LOC | LOC | N/A |
| Virginia Neurological Institute | Short LOC, PTA < 1 hr, GCS score = 15 |
Short LOC, PTA 1 to 24 hrs, GCS score = 15 | LOC < 5 min, PTA ≥ 24 h, GCS score > 15 for < 5 min | LOC < 5 min, PTA N/A, GCS score < 15 for < 1 hr | LOC 5 to 60 min, PTA N/A, GCS score < 12 for > 5 min or < 15 for > 1 hr |
| American Academy of Neurology | No LOC, Symptoms < 15 min |
N/A | No LOC, Symptoms > 15 min |
Any LOC | N/A |
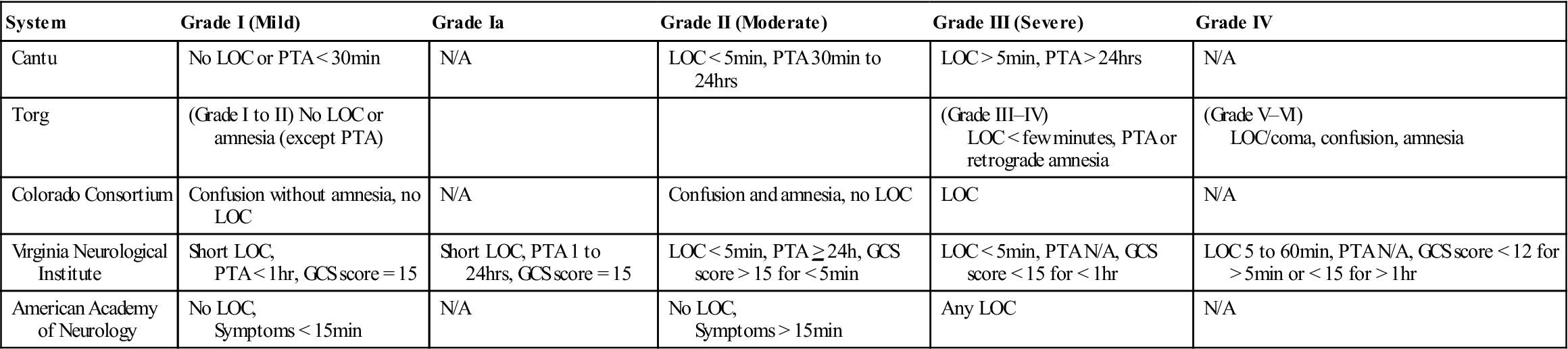
GCS, Glasgow Coma Scale; LOC, loss of consciousness; PTA, posttraumatic amnesia.
From Durand P, Adamson GJ: On-the-field management of athletic head injuries, J Am Acad Orthop Surg 12:194, 2004. Adapted with permission from Macciocchi SN, Barth JT, Littlefield LM: Outcome after mild head injury. Clin Sports Med 17:27–36, 1998.
TABLE 2-10
Examples of Neurophysiological Tests
| Test | Ability Evaluated |
| Continuous Performance Test | Sustained attention, reaction time |
| Controlled Oral Word Association Test | Word fluency, word retrieval |
| Delayed Recall (from Hopkins Verbal Learning Test) | Delayed learning from previously learned word list |
| Digit Span (from Wechsler Memory Scale—revised) | Attention span |
| Grooved-Pegboard Test | Motor speed and coordination |
| Hopkins Verbal Learning Test | Verbal memory (memory for words) |
| Immediate Measurement of Performance and Cognitive Testing (IMPACT) | Attention span, sustained and selective attention, reaction time, memory |
| Number/Symbol Matching | Processing speed, visual motor speed |
| Orientation Questionnaire | Orientation, post traumatic amnesia |
| Sequential Digit Tracking | Sustained attention, reaction time |
| Stroop Test | Mental flexibility, attention |
| Symbol Digit Modalities | Visual scanning, attention |
| Symbol Memory | Immediate visual memory |
| Trail-Making Test | Visual scanning, mental flexibility |
| Verbal Working Memory | Word memory, working memory |
| Visual Span | Visual attention, immediate memory |
| Visual Symbol Search | Visual scanning, reaction time |
| Word/Colour Tracking | Focused attention, response inhibition |
Data from Maroon JC, Lovell MR, Norwig J, et al: Cerebral concussion in athletes: evaluation and neurophysiological testing. Neurosurg 47:659–672, 2000.
TABLE 2-11
Type of Headache Pain and Usual Causes
| Type of Pain | Usual Causes |
| Acute | Trauma, acute infection, impending cerebrovascular accident, subarachnoid hemorrhage |
| Chronic, recurrent | Migraine (definite pattern of irregular interval); eyestrain; noise; excessive eating, drinking, or smoking; inadequate ventilation |
| Continuous, recurrent | Trauma |
| Severe, intense | Meningitis, aneurysm (ruptured), migraine, brain tumor |
| Intense, transient, shocklike | Neuralgia |
| Throbbing, pulsating (vascular) | Migraine, fever, hypertension, aortic insufficiency, neuralgia |
| Constant, tight (bandlike), bilateral | Muscle contraction |
TABLE 2-12
Location of Headache and Usual Causes
| Location | Usual Causes |
| Forehead | Sinusitis, eye or nose disorder, muscle spasm of occipital or suboccipital region |
| Side of head | Migraine, eye or ear disorder, auriculotemporal neuralgia |
| Occipital | Myofascial problems, herniated disc, eyestrain, hypertension, occipital neuralgia |
| Parietal | Hysteria (viselike), meningitis, constipation, tumor |
| Face | Maxillary sinusitis, trigeminal neuralgia, dental problems, tumor |
TABLE 2-13
Effect of Position or Time of Day on Headache
| Position or Time of Day When Headache Is Worst | Usual Causes |
| Morning | Sinusitis, migraine, hypertension, alcoholism, sleeping position |
| Afternoon | Eyestrain, muscle tension |
| Night | Intracranial disease, osteomyelitis, nephritis |
| Bending | Sinusitis |
| Lying horizontal | Migraine |
TABLE 2-14
Headaches: A Differential Diagnosis
| Disorder | Sex/Age Predominance | Nature of Pain | Frequency | Location | Duration | Prodromal Events | Precipitating Factors | Cause | Familial Predisposition | Other Possible Symptoms |
| Migraine | Female/20 to 40 years | Builds to throbbing and intense | Usually not more than twice a week; may be noctural | Usually unilateral | Several hours to days | Visual disturbances can occur contralateral to pain site | Unknown, may be physical, emotional, hormonal, dietary | Vasomotor | Yes | Nausea, vomiting, pallor, photophobia, mood disturbances, fluid retention |
| Cluster (histamine) headache | Male/40 to 60 years | Excruciating, stabbing, burning, pulsating | 1 to 4 episodes per 24 hours; nocturnal manifestation | Unilateral, eye, temple, forehead | Minutes to hours | Sleep disturbances or personality changes can occur | Unknown, may be serotonin, histamine, hormonal blood flow | Vasomotor | Minor | Ipsilateral sweating of face, lacrimation, nasal congestion or discharge |
| Hypertension headache | None | Dull, throbbing, nonlocalized | Variable | Entire cranium, especially occipital region | Variable | None | Activity that increases blood pressure | High blood pressure; diastolic >120 mm Hg | Only as related to hypertension | |
| Trigeminal neuralgia (tic douloureux) | Female/40 to 60 years | Excruciating, spontaneous, lancinating, lightning | Can occur many (12 or more) times per day | Unilateral along trigeminal nerve area | 30 seconds to 1 minute | Disagreeable tingling | Touch (cold) to affected area | Neurological | None | Reddened conjunctiva, lacrimation |
| Glossopharyngeal neuralgia | Male/40 to 60 years | Excruciating, spontaneous, lancinating, lightning | Can occur many (12 or more) times per day | Unilateral retrolingual area to ear | 30 seconds to 1 minute | None | Movement or contact of the pharynx | Neurological | None | |
| Cervical neuralgia | None | Dull pain or pressure in head | Bilateral, occipital, frontal, or facial | Variable | None | Posture or head movement | Neurological, pressure on roots of spinal nerves | None | Dizziness, auditory disturbances | |
| Eye disorders | None | Generalized discomfort in or around the eyes | Intensify with sustained visual effort | Entire cranium | During and after visual effort | None | Impairment of eye function | Cornea, iris, or intraocular pain | Possible | Diminished vision, sensitivity to light |
| Sinus, ear, and nasal disorders | None | Dull, persistent | Variable | Frontal, temporal, ear, nose, occipital | Variable | None | Infection, allergy, chemical, bending, straining | Blockage, inflammation, infection | None |
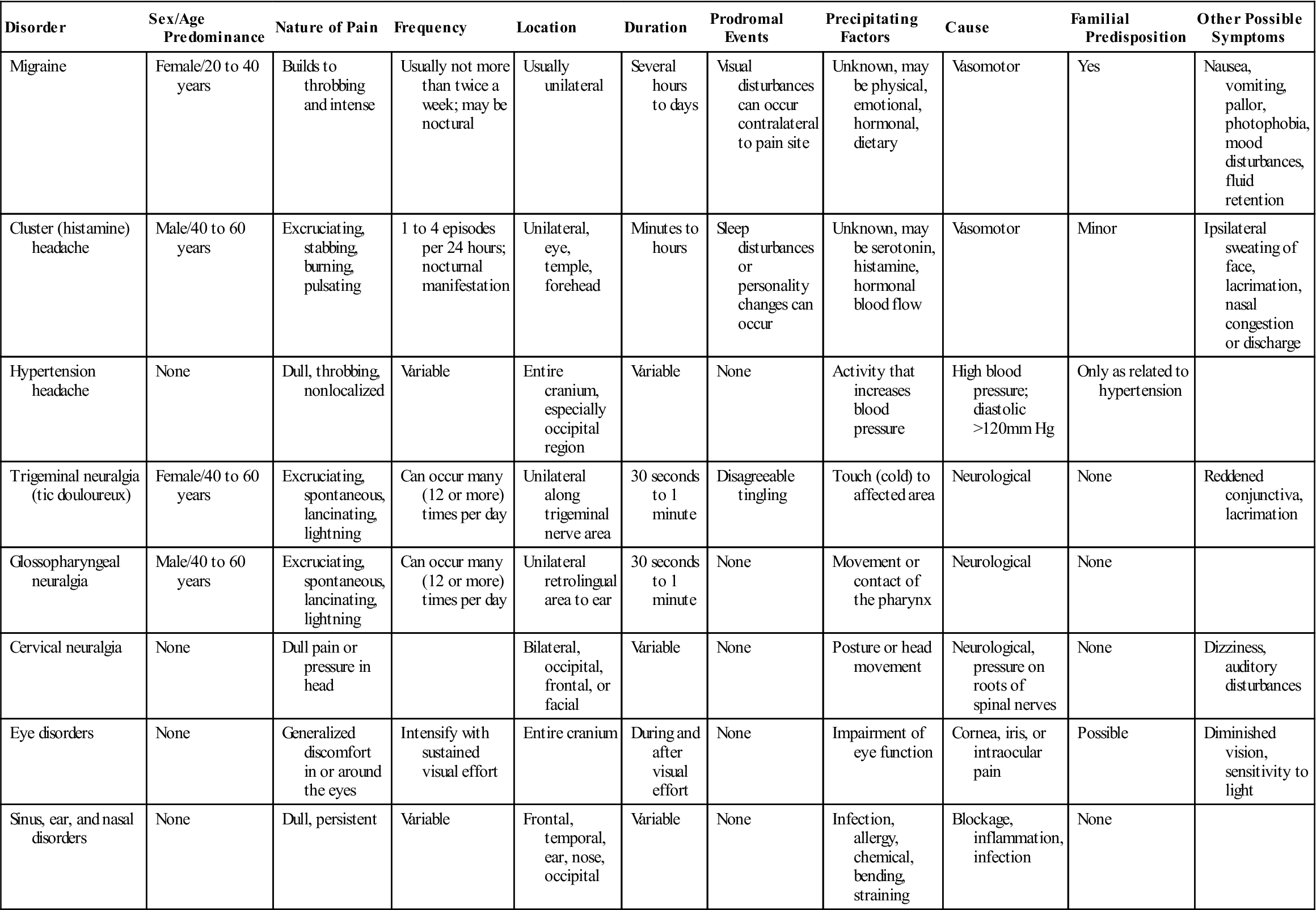
Modified from Esposito CJ, Grim GA, Binkley TK: Headaches: a differential diagnosis. J Craniomand Pract 4:320–321, 1986.
TABLE 2-15
Common Visual Eye Symptoms and Disease States
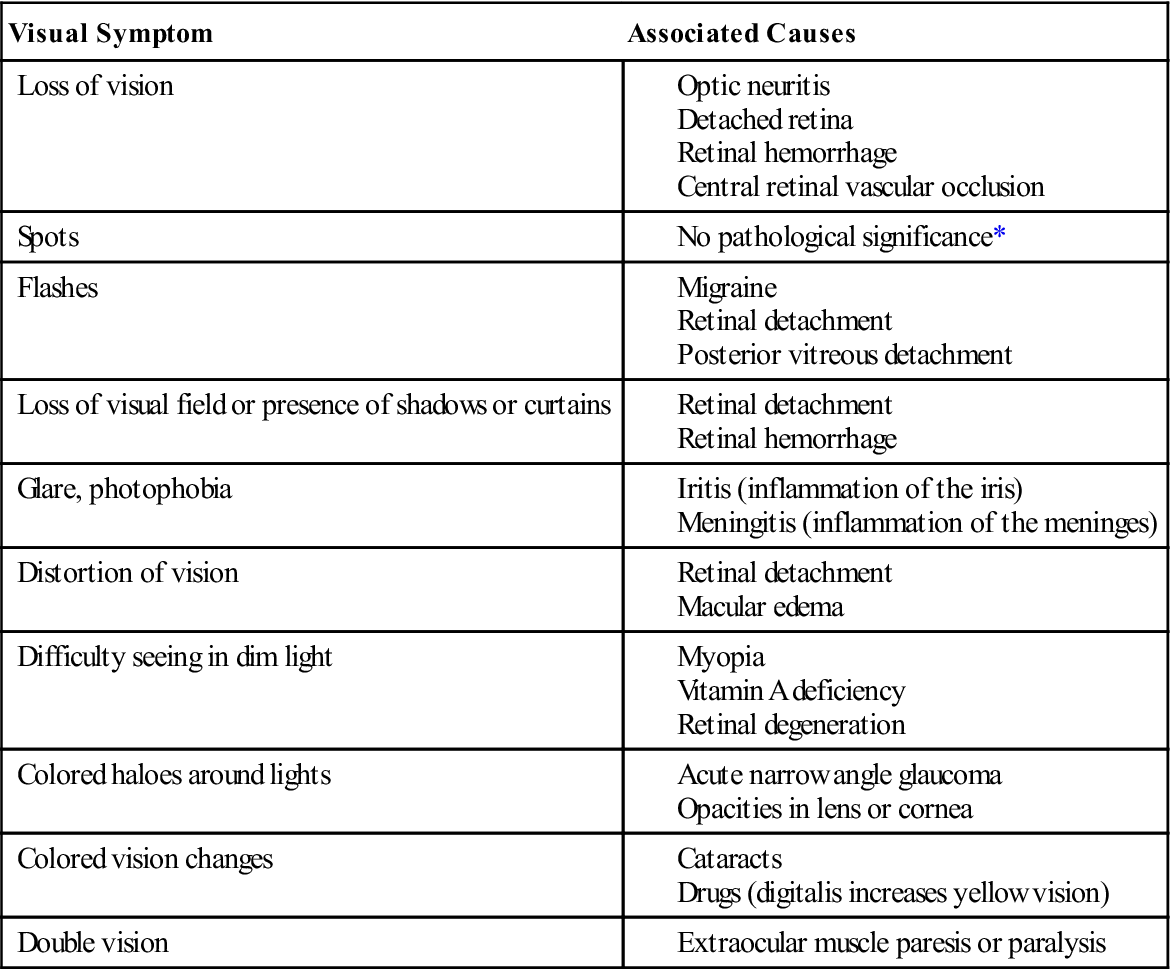
*May precede a retinal detachment or be associated with fertility drugs.
From Swartz MH: Textbook of physical diagnosis, Philadelphia, 1989, WB Saunders, p. 132.
TABLE 2-16