Chapter 76 Hardware Complications After Anterior Cruciate Ligament Reconstruction
Interference Screws
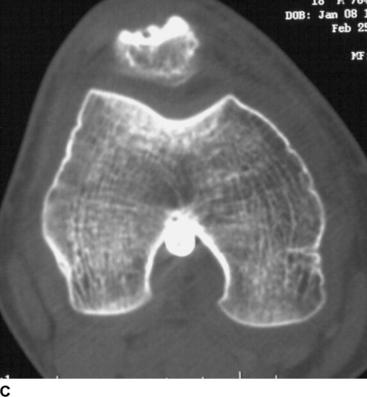
Intraoperative complications include intraarticular placement of the hardware, which ideally will be recognized during the procedure and adjusted accordingly (Fig. 76-1). During insertion of the screw, possible complications include laceration of the graft-passing suture,1 advancement of the graft within the bone tunnel,1 graft laceration1 and even rupture,2 fracture of the graft bone plug,3 and screw breakage.4–6 To minimize the risk of lacerating the passing suture, at least one suture can be passed through the tendon at the base of the bone plug.1 To minimize the risk of graft rupture, methylene blue can be used to mark the bone–tendon junction of the graft, the anterior portion of the bone tunnel can be notched to ease the initial engagement of the screw, the cancellous edge of the bone plug can be placed facing anterior flush with the intraarticular edge of the femoral tunnel, and a protective sheath or cannula can be used to protect the graft during screw placement.2 Another helpful technique to protect the graft is to insert the femoral screw over a guidewire drilled through a cannulated screwdriver.
If the graft ruptures during screw placement, a number of salvage options may be used. If a patellar tendon graft is cut at the bone–tendon junction, the graft can be reversed, placing the intact bone plug in the femoral tunnel and fixing the tendinous portion of the graft through the tibial tunnel with a post or button.2,7 If the remaining graft length is insufficient, an alternative autograft or allograft should be used. To minimize the chance of graft advancement, it is important to maintain constant tension on the passing sutures during screw insertion.1 Screw breakage during insertion has been reported with bioabsorbable screws in as many as 10% of cases.4,5 Steps to minimize such a complication include use of a dilator device to create a pilot hole for screw insertion, maintenance of continuous pressure on the screwdriver to keep it fully seated, and use of a screw 1 mm smaller than the diameter of the tunnel.6
Postoperative complications include intraarticular placement of hardware, which may not be recognized at the time of surgery and can present clinically after the index procedure. A second procedure may be necessary to reposition or remove the misplaced hardware. Late screw breakage8–12 and delayed intraarticular migration of interference screws13–16 have also been described in the literature. Late migration of interference screws is rare but should be considered in the case of sudden pain in the late postoperative period after ACL reconstruction and, in the case of a metallic screw, can easily be evaluated with plain films. If such a complication is encountered, removal is mandated to minimize mechanical problems and cartilage damage.9,14,17 An arthroscopic approach is preferred,17 even if the screw is in the notch or popliteal fossa, although an arthrotomy may be required.15
Endobutton
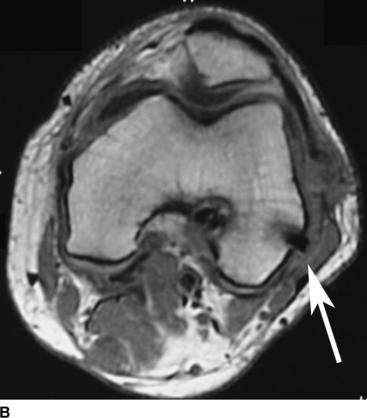
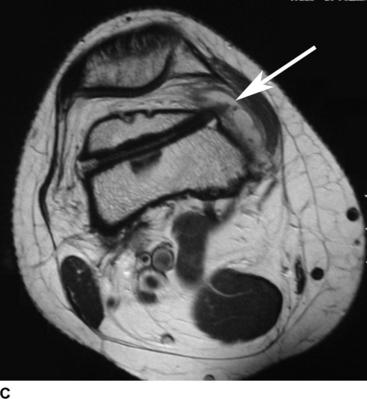
The Endobutton is another widely used fixation device that has been associated with specific complications. The Endobutton may remain in the femoral tunnel rather than flipping outside of the tunnel to rest on the lateral femoral cortex18 (Fig. 76-2). Conversely, the Endobutton may be pulled too far off the femoral cortex into the overlying soft tissue19 (Fig. 76-3). To ensure that the Endobutton has flipped and is in the correct position, the femoral tunnel length should be overdrilled by 6 mm and the graft should be marked at a location 6 mm distal to the desired insertion level.18 Once the Endobutton has flipped, the surgeon should feel for the button flipped on the lateral side of the femur against the cortex by pulling on the sutures. The surgeon can then pull back on the graft from below and pull both Endobutton sutures to make sure the button is not flipping with tension on the graft from the tibial side. If there is any doubt as to the position of the Endobutton, intraoperative fluoroscopy or x-rays should be used to confirm proper placement.19
Postoperatively, Muneta et al20 described late detachment and intraarticular migration of an Endobutton that had been fixed in the suprapatellar pouch, most likely due to impingement between the patella and femoral groove. To avoid this impingement and possible inflammatory reaction, it is preferable not to affix the Endobutton in the joint, particularly near the patellofemoral joint.20
Cross-Pin Fixation
A number of postoperative complications associated with cross-pin fixation have recently been described in the literature. Incorrect placement, including leaving the pin proud on the lateral side of the femur as well as advancing the pin too far to penetrate the medial cortex of the femur, should be avoided as it may require reoperation for hardware removal21 (Fig. 76-4). The pin can break even after graft incorporation.22 The case of late breakage reported by Han et al22 using the Rigidfix system (Mitek Products, Norwood, MA) was attributed to an improper femoral tunnel with posterior wall blowout and posterior direction of the cross-pins, potentially leading to abnormally high stress on the pins. Iliotibial band syndrome has also been described, either from direct irritation23 or in association with breakage of the femoral bioabsorbable cross-pin, specifically BioTransfix (Arthrex, Naples, FL).24
Tibia Fixation
A number of options can be used for cortical fixation in the tibia, including interference screws and staples. Although early studies indicated a high incidence of hardware removal from the tibia due to pain when using interference screws,23,25,26 low-profile interference screws are usually well tolerated.27 Another option for tibial fixation when using hamstring grafts or Achilles allografts is a cortical screw with a spiked washer. Although one series using a higher-profile, round-headed screw reported a 70% incidence of hardware removal due to pain,28 other studies reviewing lower-profile screws suggest a very low, almost negligible, rate of hardware removal with this type of fixation.27,29 Staples are another method of fixation, used for supplementary fixation more often than primary fixation. The major concern with staples is their high profile and the resulting incidence (as high as 29%) of kneeling pain leading to hardware removal.30
Skeletally Immature Patients
Graft fixation in skeletally immature patients has its own potential for complication regardless of the type of fixation device used. The primary concern is disruption of the growth plates, which can manifest itself in a number of different ways including limb length discrepancy,31,32 tibial recurvatum,33 and valgus deformity of the distal femur.33,34 Specific recommendations with regard to fixation include avoidance of fixation hardware across the lateral distal femoral epiphysis and tibial tubercle apophysis.33 Although this complication reflects the surgical approach and technique as much as the type of graft fixation, it is important to attempt to avoid or at least minimize disruption of the growth plate(s) whenever possible.
Conclusion
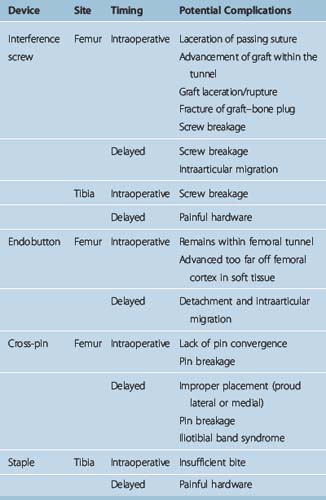
In summary, each method of graft fixation presents its own potential complications both at the time of surgery and in the short- and long-term postoperative period (Table 76-1). Surgeons should be aware of the potential complications with the methods of fixation they use, how to avoid them, and how to treat them if they occur. Special considerations should be made in skeletally immature patients to minimize disruption of the growth place, with graft harvest, tunnel placement and drilling, and graft fixation.
1 Matthews LS, Soffer SR. Pitfalls in the use of interference screws for anterior cruciate ligament reconstruction: brief report. Arthroscopy. 1989;5:225-226.
2 Arciero RA. Endoscopic anterior cruciate ligament reconstruction: complication of graft rupture and a method of salvage. Am J Knee Surg. 1996;9:27-31.
3 Malek MM, Kunkle KL, Knable KR. Intraoperative complications of arthroscopically assisted ACL reconstruction using patellar tendon autograft. Instr Course Lect. 1996;45:297-302.
4 McGuire DA, Barber FA, Elrod BF, et al. Bioabsorbable interference screws for graft fixation in anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:463-473.
5 Pena F, Grontveldt T, Brown GA, et al. Comparison of failure strength between metallic and absorbable interference screws. Influence of insertion torque, tunnel-bone block gap, bone mineral density, and interference. Am J Sports Med. 1996;24:329-334.
6 Smith CA, Tennent TD, Pearson SE, et al. Fracture of Bilok interference screws on insertion during anterior cruciate ligament reconstruction. Arthroscopy. 19, 2003. E4–6
7 Cain ELJr, Gillogly SD, Andrews JR. Management of intraoperative complications associated with autogenous patellar tendon graft anterior cruciate ligament reconstruction. Instr Course Lect. 2003;52:359-367.
8 Bottoni CR, Deberardino TM, Fester EW, et al. An intra-articular bioabsorbable interference screw mimicking an acute meniscal tear 8 months after an anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:395-398.
9 Lembeck B, Wulker N. Severe cartilage damage by broken poly-L-lactic acid (PLLA) interference screw after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:283-286.
10 Macdonald P, Arneja S. Biodegradable screw presents as a loose intra-articular body after anterior cruciate ligament reconstruction. Arthroscopy. 19, 2003. E22–24
11 Shafer BL, Simonian PT. Broken poly-L-lactic acid interference screw after ligament reconstruction. Arthroscopy. 2002;18:E35.
12 Werner A, Wild A, Ilg A, et al. Secondary intra-articular dislocation of a broken bioabsorbable interference screw after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2002;10:30-32.
13 Bush-Joseph CA, Bach BRJr. Migration of femoral interference screw after anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11:32-34.
14 Hallet A, Mohammed A. Displaced femoral interference screw causing locked knee. Injury. 2003;34:797-798.
15 Karlakki SL, Downes ME. Intra-articular migration of a femoral interference screw: open or arthroscopic removal. Arthroscopy. 2003;19:E19.
16 Sidhu DS, Wroble RR. Intra-articular migration of a femoral interference fit screw. A complication of an anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:269-271.
17 Resinger C, Vecsei V, Heinz T, et al. The removal of a dislocated femoral interference screw through a posteromedial portal. Arthroscopy. 2005;21:1398.
18 Karaoglu S, Halici M, Baktir A. An unidentified pitfall of Endobutton use: case report. Knee Surg Sports Traumatol Arthrosc. 2002;10:247-249.
19 Simonian PT, Behr CT, Stechschulte DJJr, et al. Potential pitfall of the EndoButton. Arthroscopy. 1998;14:66-69.
20 Muneta T, Yagishita K, Kurihara Y, et al. Intra-articular detachment of the Endobutton more than 18 months after anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:775-778.
21 Marx RG, Spock CR. Complications following hamstring anterior cruciate ligament reconstruction with femoral cross-pin fixation. Arthroscopy. 2005;21:762.
22 Han I, Kim YH, Yoo JH, et al. Broken bioabsorbable femoral cross-pin after anterior cruciate ligament reconstruction with hamstring tendon graft: a case report. Am J Sports Med. 2005;33:1742-1745.
23 Clark R, Olsen RE, Larson BJ, et al. Cross-pin femoral fixation: a new technique for hamstring anterior cruciate ligament reconstruction of the knee. Arthroscopy. 1998;14:258-267.
24 Pelfort X, Monllau JC, Puig L. Iliotibial band friction syndrome after anterior cruciate ligament reconstruction using the transfix device: report of two cases and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2006;14:586-589.
25 Howell SM, Deutsch ML. Comparison of endoscopic and two-incision techniques for reconstructing a torn anterior cruciate ligament using hamstring tendons. Arthroscopy. 1999;15:594-606.
26 Siegel MG, Barber-Westin SD. Arthroscopic-assisted outpatient anterior cruciate ligament reconstruction using the semitendinosus and gracilis tendons. Arthroscopy. 1998;14:268-277.
27 Prodromos CC, Han YS, Keller BL, et al. Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy. 2005;21:138-146.
28 Jansson KA, Linko E, Sandelin J, et al. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:12-18.
29 Prodromos CC, Joyce BT, Shi K, et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21:1202.
30 Hill PF, Russell VJ, Salmon LJ, et al. The influence of supplementary tibial fixation on laxity measurements after anterior cruciate ligament reconstruction with hamstring tendons in female patients. Am J Sports Med. 2005;33:94-101.
31 Andrews M, Noyes FR, Barber-Westin SD. Anterior cruciate ligament allograft reconstruction in the skeletally immature athlete. Am J Sports Med. 1994;22:48-54.
32 Lipscomb AB, Anderson AF. Tears of the anterior cruciate ligament in adolescents. J Bone Joint Surg. 1986;68A:19-28.
33 Kocher MS, Saxon HS, Hovis WD, et al. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop. 2002;22:452-457.
34 Koman JD, Sanders JO. Valgus deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. A case report. J Bone Joint Surg. 1999;81A:711-715.