CHAPTER 71 HAND FRACTURES
The presence of an opposable thumb separates man from other primates. The hand serves many functions, ranging from precise prehension to power gripping. This requires finely coordinated interplay among the various components of the musculoskeletal architecture of the hand. A stable and well-aligned skeletal framework, stable joints, and balance between intrinsic and extrinsic muscles and tendinous systems are all necessary for good hand function.
Most hand fractures can be treated nonoperatively by means of closed manipulation, splinting, and protected motion. Certain fracture patterns, however, are best treated by operative intervention. The goals of treatment remain the same and include accurate reduction, stabilization, wound treatment, and early mobilization. Inability to achieve or maintain reduction in the so-called safe or functional position denotes that a fracture is unstable. The fracture pattern and integrity of the periosteal sleeve and surrounding soft tissues determine fracture stability. Unopposed pull of muscles can lead to instability. Fractures involving articular surfaces demand accurate reduction to achieve good motion. Severely comminuted fractures are often best treated closed, because open reduction can lead to devitalization of small bony fragments. These fractures are well suited for closed pinning. Open fractures with loss of bone, contamination, or poor soft tissue coverage are best treated with external fixation. This permits fixation and maintenance of length while allowing for soft tissue healing and dressing changes. Definitive procedures to achieve bony union and soft tissue coverage can be carried out in a delayed fashion. Indications for operative treatment are summarized in Table 1.
Table 1 Indications for Operative Treatment in Hand Fractures
INCIDENCE
The most common upper extremity fractures are those of the metacarpals and phalanges. In a series of 4303 patients presenting to the emergency room with fractures, 19% had hand fractures.1 The phalanges were most commonly fractured. Males between the ages of 15 and 35 were most commonly injured. Fractures of the little finger ray were most common.
Hove, in a series of 1000 consecutive patients, found that metacarpals, phalanges, and carpal bones accounted for 36%, 46%, and 18% of the fractures, respectively.2 Chung and Spilson analyzed data from the 1998 National Hospital Ambulatory Medical Care Survey and estimated that in 1998, there were more than 600,000 metacarpal and phalangeal fractures in the United States.3
Fractures in children follow different patterns in various age groups because of differing mechanisms of injury. In a review of 242 hand fractures, Mahabir et al. found that 75% of injuries were in males, the mean age being 11 years.4 The incidence of fractures was very low in the very young, rose sharply at age 9, and peaked at 12 years. Forty percent were epiphyseal fractures, predominantly Salter-Harris II. The fifth metacarpal was the most frequently fractured bone.
The incidence of hand injuries in polytrauma was studied by Schaller and Geldmacher.5 They noted a 20% incidence of associated hand injuries, 75% of which were closed fractures. Ninety-three percent were involved in motor vehicle accidents.
MECHANISM OF INJURY
Chung and Spilson described the cause of injury in hand and forearm fractures.3 Forty-seven percent of injuries were due to falls, while 15% were due to being struck by a person or object. Ten percent were due to vehicular accidents. Other causes included being caught between objects, accidents involving machines or tools, injury due to another person, and nontraffic motor vehicle accidents.
De Jonge et al. studied the incidence and etiology of 6857 phalangeal fractures.6 They found that falls were responsible for most injuries in patients 70 years or older, while sports were the main cause in the age group 10–29 years. The highest incidence was in males aged 40–70 years, and the cause was machinery. Over 45% of hand fractures in children occurred either during sports or in a fight.
DIAGNOSIS
Management of hand injuries requires a good understanding of hand anatomy and biomechanics. The individual needs of the patient need to be taken into account before devising a treatment plan. A detailed history needs to be obtained. Key points to be elicited are noted in Table 2.
METACARPAL FRACTURES
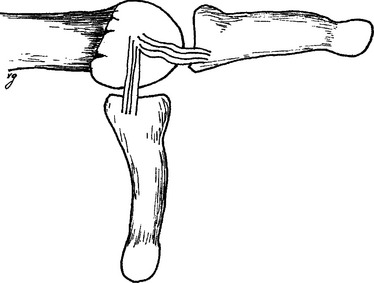
The metacarpals are structurally divided into the head, neck, shaft, and base. The metacarpal head articulates with the base of the proximal phalanx. The collateral ligaments between the metacarpal and phalanx arise in an eccentric position. Hence, these ligaments are stretched in flexion and lax in extension, and the joint is stable in flexion (Figure 1). The thumb metacarpal and fourth and fifth metacarpals are mobile. Because of its unique anatomy, thumb fractures are dealt with separately. Common metacarpal fracture patterns are illustrated in Figure 2.
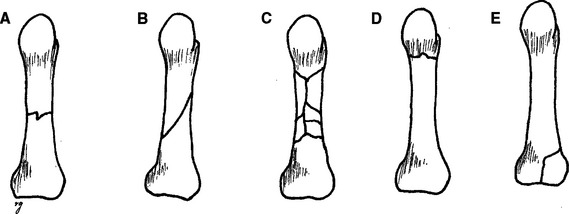
Figure 2 Common fracture patterns. (A) Transverse. (B) Spiral. (C) Comminuted. (D) Neck. (E) Intra-articular.
Metacarpal Shaft Fractures
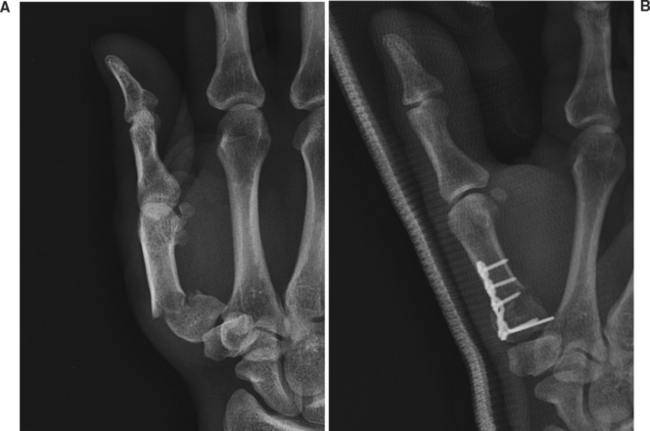
Open reduction is indicated when the fracture is malaligned or unstable. Open fractures and those with associated soft tissue injuries are also best treated by open reduction. This permits earlier mobilization to prevent stiffness. With multiple metacarpal fractures, the stabilizing influence of the adjacent metacarpals is lost, and such fractures may need open reduction and internal fixation. Various techniques are available to stabilize fractures. Spiral or long oblique fractures can be stabilized by lag screws (Figure 3). The length of the fracture line should be at least twice the diameter of the bone. The proximal hole is overdrilled to a diameter wider than the thread of the screw. As the screw is tightened and the threads grip the distal fragment, interfragmentary compression is achieved.

Figure 3 (A) Metacarpal shaft fracture sustained in a fist fight. (B) Fixation with three lag screws.
Kirschner wires can be used to stabilize shaft fractures. Percutaneous insertion involves minimal soft tissue dissection; however, the stabilization is not rigid, and patients need to be splinted. Rarely, pin tract infections can complicate treatment. Multiple wires are usually placed to avoid rotation of fragments (Figure 4).
Metacarpal Neck Fractures
Metacarpal neck fractures angulate dorsally because of the pull of the intrinsic muscles. The fourth and fifth metacarpals have more mobility at the carpometacarpal joints, and hence angulation in the ulnar metacarpals is better tolerated from the functional standpoint. Patients may complain about the resultant deformity—a loss of prominence of the knuckle—and also about feeling a mass in the clenched fist.
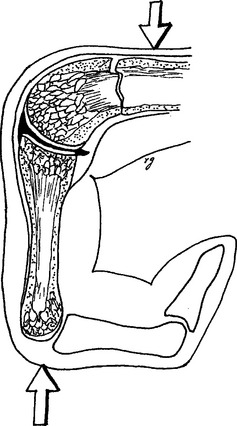
Closed reduction of metacarpal neck fractures is achieved by the Jahss maneuver8 (Figure 5). Local anesthesia with a hematoma block is administered. Traction is applied and the fracture is disimpacted. The metacarpophalangeal and interphalangeal joints are flexed to 90 degrees. This relaxes the intrinsics and tightens the collateral ligaments. An upward push on the proximal phalanx transmits force to the distal fragment to achieve reduction. Reduction is confirmed by radiology. The hand is immobilized in an ulnar gutter splint. If the fracture is more than 7–10 days old, closed reduction is usually not possible.
Persistent dorsal angulation of more than 30–40 degrees of the ring and little finger metacarpals, more than 10–15 degrees in the index and long finger metacarpals, and any rotational malalignment require operative intervention. Percutaneous insertion of Kirschner pins usually suffices. On occasion, open reduction and pinning, or plate application is necessary.6
Metacarpal Head Fractures
Metacarpal head fractures are unusual and are usually intra-articular. Index metacarpal head fractures are the most common. These fractures usually result from direct trauma or axial loading. In addition to the standard three views, special views, such as the Brewerton view or skyline metacarpal view, are useful. Significant joint incongruity requires operative management.6
Thumb Metacarpal Fractures
Thumb metacarpal head, neck, and shaft fractures are treated as outlined previously (Figure 6). Fractures of the metacarpal base are important because loss of the carpometacarpal joint integrity can severely compromise hand function. Two patterns of injury are notable: Bennett’s fracture and Rolando fracture.6
Bennett’s Fracture
Bennett’s fracture is an intra-articular fracture of the base of the thumb metacarpal (Figure 7). The smaller ulnar fragment remains attached to the trapezium by the volar oblique ligament, and the shaft is displaced by the pull of the adductor pollicis and abductor pollicis muscles. It is difficult to maintain reduction in a cast, so these fractures require operative intervention. Once reduced, the reduction is maintained by passing a Kirschner wire through the metacarpal shaft into the trapezium or the second metacarpal. It is not necessary to include the small fragment. If reduction is not possible by the closed technique, open reduction is necessary.
PHALANGEAL FRACTURES
Proximal and Middle Phalangeal Fractures
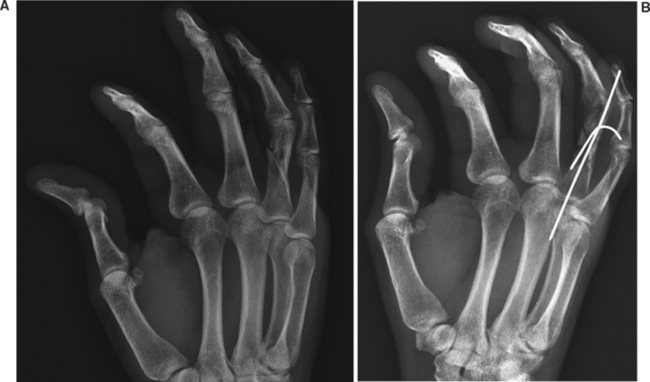
Stable nondisplaced shaft fractures and those that are stable after reduction are immobilized with malleable aluminum splints and a short arm splint in the safe position. The finger can be “Buddy taped” to an adjacent noninjured finger to prevent rotational malalignment. Mobilization should be initiated early to prevent stiffness. Immobilization for more than 3 weeks is seldom necessary. Unstable fractures require pinning (Figure 8). Plate and screw application in the fingers can potentially compromise tendon function and soft tissue coverage.
DISLOCATIONS
Proximal Interphalangeal Joint Dislocation
Dislocation of the proximal interphalangeal (PIP) joint is the most common ligamentous injury in the hand. These can be dorsal, volar, or lateral (Figure 9).
METACARPOPHALANGEAL JOINTS
These are usually dorsal dislocations caused by hyperextension of the joint. They are divided into simple subluxations and complex dislocations. In simple subluxations, the volar plate is draped over the metacarpal head, and the proximal phalanx is in hyperextension over the metacarpal head. Simple dislocations are reduced by flexing the wrist while applying traction and flexing the MP joint. Following reduction, a dorsal extension block splint is applied (Figure 10).
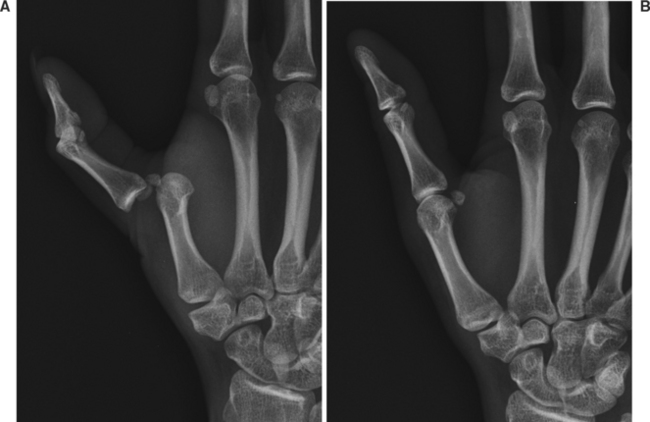
Figure 10 (A) Simple metacarpophalangeal joint dislocation following a fist fight. (B) Post reduction.
In complex dislocations, the metacarpal head protrudes volarly between the lumbrical and flexor tendon. The volar plate is folded and entrapped between the two articular surfaces. Hyperextension of a simple subluxation can pull the volar plate further into the joint, entrapping it and converting it into a complex dislocation. Complex dislocations present with the MP joint in slight extension, palpable metacarpal head in the palm, and dimpling of the skin from pull on the periosteal dermal attachments. X-rays, especially of the first metacarpophalangeal joint, may show the sesamoid bones in the joint space, indicating volar plate entrapment. Complex dislocations require open reduction.
COMPLICATIONS
Both undertreatment and overtreatment of hand fractures and dislocations can lead to complications. The most common complication is stiffness, and its prevention is of paramount importance in the restoration of hand function. Joint contractures can result from prolonged immobilization. The safe position must be utilized, whenever feasible. Scarring can result in tendon adhesions and entrapment of nerves, resulting in poor function. Stabilization of fractures and early protected motion are essential. Clinical healing precedes radiologic union. On the other hand, inadequate immobilization can lead to malunion, or nonunion. Malunion and nonunion may require operative intervention to correct. Corrective osteotomies and internal fixation are utilized to treat malunion. Nonunions may require bone grafting (Figure 11). Infection can be seen in open fractures and are more likely in human bite injuries. These injuries require antibiotic prophylaxis after adequate debridement.
1 van Onselen EB, et al. Prevalence and distribution of hand fractures. J Hand Surg [Br]. 2003;28(5):491-495.
2 Hove LM. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27(4):317-319.
3 Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg [Am]. 2001;26(5):908-915.
4 Mahabir RC, et al. Pediatric hand fractures: a review. Pediatr Emerg Care. 2001;17(3):153-156.
5 Schaller P, Geldmacher J. Hand injury in polytrauma. A retrospective study of 782 cases. Handchir Mikrochir Plast Chir. 1994;26(6):307-312.
6 De Jonge JJ, et al. Phalangeal fractures of the hand: an analysis of gender and age-related incidence and aetiology. J Hand Surg. 1994;19(2):168-170.
7 Jahss SA. Fractures of the metacarpals: a new method of reduction and immobilization. J Bone Joint Surg. 1938;20:178-186.