Chapter 19 GYNECOMASTIA
Causes of Gynecomastia
Key Physical Findings
 Differentiate pseudogynecomastia (fatty tissue) from true gynecomastia
Differentiate pseudogynecomastia (fatty tissue) from true gynecomastia
 Evidence of systemic disease, such as thyrotoxicosis, liver disease, or adrenal disease
Evidence of systemic disease, such as thyrotoxicosis, liver disease, or adrenal disease
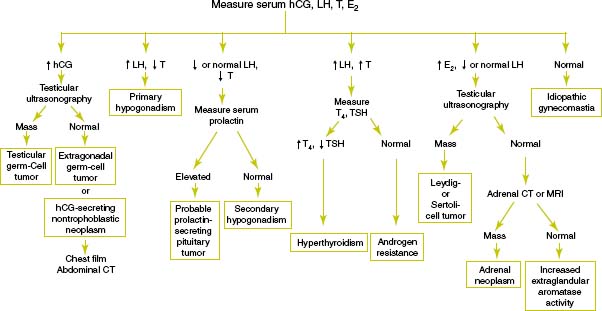
Suggested Work-up
| Thyroid-stimulating hormone (TSH) | To evaluate for hyperthyroidism |
| Luteinizing hormone | See Figure 19-1 |
| Testosterone level | See Figure 19-1 |
| Estradiol level | To evaluate for testicular Leydig-cell tumor or feminizing adrenocortical neoplasm |
| Human chorionic gonadotropin (hCG) level | To evaluate for testicular germ cell tumor, extragonadal germ cell tumor, or hCG-secreting nontrophoblastic neoplasm |
| See Figure 19-1 | |
| Serum electrolytes | To evaluate for adrenal disease |
| Blood urea nitrogen (BUN) and creatinine | To evaluate for renal disease |
| Liver function tests | To evaluate for liver disease |
Additional Work-up
| Prolactin level | If gynecomastia is associated with galactorrhea to evaluate for prolactinoma |
| HIV test | If HIV infection is suspected or the patient has risk factors for infection |
| Testicular ultrasonongraphy | If testicular examination is abnormal or if estradiol is increased with a decreased or normal luteinizing hormone |
| Adrenal computed tomography (CT) or magnetic resonance imaging (MRI) | If adrenal neoplasm is suspected |
1. Braunstein G.D. Gynecomastia. N Engl J Med. 1993;328:490–495.
2. Einav-Bachar R., Phillip M., Aurbach-Klipper Y., Lazar L. Prepubertal gynaecomastia: aetiology, course, and outcome. Clin Endocrinol (Oxf). 2004;61:55–60.
3. Henley D.V., Lipson N., Korach K.S., Bloch C.A. Prepubertal gynecomastia linked to lavender and tea tree oils. N Engl J Med. 2007;356:479–485.
4. Rapaport R. Gynecomastia. In Behrman R.E., Kliegman R.M., Jenson H.B., editors: Nelson Textbook of Pediatrics, 17th ed., Philadelphia: WB Saunders, 2004.
5. Wilson J.D. Endocrine disorders of the breast. In: Isselbacher K.J., Braunwald E., Wilson J.D., editors. Harrisons’s Textbook of Internal Medicine. 13th ed. New York: McGraw-Hill; 1994:2037–2039.
6. Wise G.J., Roorda A.K., Kalter R. Male breast disease. J Am Coll Surg. 2005;200:255–269.