Chapter 38 SCROTAL MASSES
General Discussion
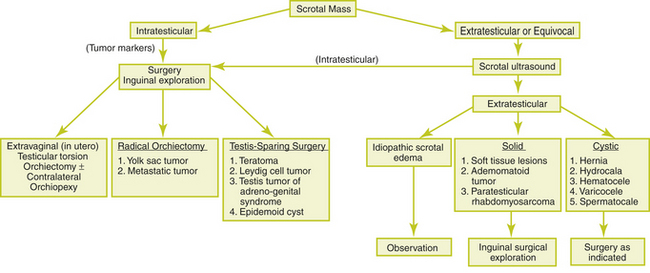
The most common painless scrotal masses in infants, children, and adolescents include indirect inguinal hernias, hydroceles, varicoceles, and spermatoceles. Testicular tumors, perinatal testicular torsion, acute idiopathic scrotal edema, and soft tissue tumors of the spermatic cord are less common causes. Figure 38-1 provides a clinical approach to the painless scrotal mass.
Painless Intratesticular Masses
Gonadoblastoma is a rare tumor that occurs in patients with intersex and dysgenetic gonads.
Causes of Scrotal Masses
Key Physical Findings
 Careful palpation and identification of the intrascrotal contents
Careful palpation and identification of the intrascrotal contents
 Testicular examination for volume, masses, or tenderness
Testicular examination for volume, masses, or tenderness
 Evaluation of the contralateral testis for bilateral testicular lesions
Evaluation of the contralateral testis for bilateral testicular lesions
 Transillumination of the testicular mass
Transillumination of the testicular mass
 Assessment of the spermatic cord
Assessment of the spermatic cord
 Examination of the inguinal canals for a hernia or cord tenderness
Examination of the inguinal canals for a hernia or cord tenderness
 Valsalva maneuver to evaluate for hernia or varicocele
Valsalva maneuver to evaluate for hernia or varicocele
 Abdominal examination for masses
Abdominal examination for masses
Suggested Work-Up
| Scrotal ultrasound | To help define suspected lesions and differentiate between intratesticular and extratesticular lesions |
Additional Work-Up
| Serum | Elevated in more than 80% of patients with yolk sac testicular tumors. It is not elevated in pediatric patients with testicular teratomas. Normal serum levels of AFP remain elevated for the first 8 months after birth. |
| Serial follow-up and serum AFP | If testicular microlithiasis is seen in association with testicular enlargement |
| Chest radiography and CT scan of the abdomen and chest | Indicated if the diagnosis of a yolk sac tumor is made |
| Serum human chorionic gonadotropin (hCG) | Little or no value in pediatric patients |
1. Haynes J.H. Inguinal and scrotal disorders. Surg Clin North Am. 2006;86:371–381.
2. Jayanthi V.R. Adolescent urology. Adolesc Med Clin. 2004;15:521–534.
3. Junnila J., Lassen P. Testicular masses. Am Fam Physician. 1998;57:685–692.
4. Skoog S.J. Benign and malignant pediatric scrotal masses. Pediatr Clin of North Am. 1997;44:1229–1250.