54 Gout and hyperuricaemia
Epidemiology
Gout is one of the oldest recognised diseases and was identified by the Egyptians in 2460 BC. Hippocrates described it as ‘arthritis of the rich’ due to the association with certain foods and alcohol. Gout affects 1–2% of adults in developed countries, and in recent decades there has been a significant rise in its prevalence and incidence (Zhang et al., 2006). The USA has seen a doubling in the number of cases with the rate of gout increasing to 4.1% in older males. However, unlike the rest of the world, prevalence in the UK appears not to be rising and from 2000 to 2005 remained at 1.4% (Rider and Jordan, 2010). The increasing numbers in many developed countries have been attributed to trends in lifestyle leading to increased risk of gout, for example, obesity, metabolic syndrome, hypertension, alcohol consumption and increased age of the general population. Although the Maori population have a marked genetic predisposition to gout, prior to 1700 they did not experience this inflammatory joint disease. It was changes in diet and lifestyle following European settlement that led to the appearance and increasing prevalence in the country. New Zealand now has probably the highest prevalence in the World with one in eight men affected (Richette and Bardin, 2010). A similar pattern has also been seen in Eastern China, where gout was considered a very rare disease in the 1980s. Changes in diet and lifestyle due to Western influences have seen its prevalence rise to 1.1% in Eastern China in 2008.
In the UK, the presentation of gout in men before the age of 45 years is unusual, but in those over the age of 75 years prevalence is greater than 7% in men and 4% in women (Doherty, 2009; Jordan et al., 2007; Zhang et al., 2006). Gout is predominantly a disease of men with a male to female ratio of 3.6:1. In women, it tends to develop after menopause when levels of oestrogen, a known uricosuric, fall.
Although environmental factors are clearly implicated in the development of gout, studies have shown that inheritance also plays an important role. In recent years, research into the genetic background of gout has identified several renal urate transporters including URAT-1 and GLUT-9 and the genes that encode them, for example, SLC22A12 and SLC2A9, respectively. Polymorphisms in these genes are associated with increased hyperuricaemia and gout (Dalbeth and Merriman, 2009; Doherty, 2009).
Pathophysiology
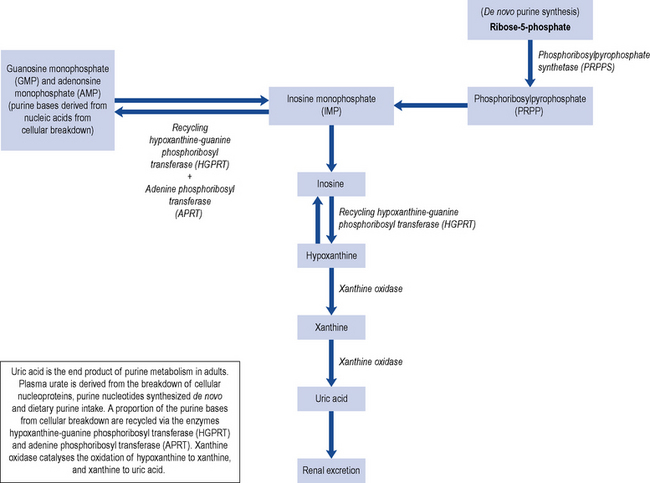
Uric acid is mainly a by-product from the breakdown of cellular nucleoproteins and purine nucleotides synthesised de novo with about a third coming from the breakdown of dietary purine intake (Fig. 54.1). Uric acid is a weak acid with a pKa of 5.75, and at the physiological pH of the extra-cellular compartment 98% of uric acid is in the ionised form of urate. This is mainly present as monosodium urate due to the high concentration of sodium in the extra-cellular compartment. Human beings and higher primates lack the enzyme uricase that degrades uric acid to the highly soluble allantoin resulting in higher concentrations of urate close to the level of solubility. Monosodium urate has a solubility limit of 380 µmol/L; when the concentration exceeds 380 µmol/L, there is a risk of precipitation and the formation of monosodium urate crystals.
Primary gout is not a consequence of an acquired disorder, but is associated with rare inborn errors of metabolism and isolated renal tubular defects in the fractional clearance of uric acid. A rare group of enzyme defects result in an increased de novo purine synthesis such as hypoxanthine-guanine phosphoribosyl transferase deficiency (Lesch-Nyhan syndrome), phosphoribosyl pyrophosphate synthetase super activity, glucose-6 phosphatase deficiency and myogenic hyperuricaemia (Table 54.1).
| Primary gout | Secondary gout |
|---|---|
| Idiopathic Rare enzyme deficiencies Hypoxanthine-guanine phosphoribosyl transferase deficiency (HPRT) Phosphoribosyl pyrophosphate synthetase super-activity Ribose-5-phosphate AMP-deaminase deficiency |
Increased uric acid production Lymphoproliferative/Myeloproliferative Chronic haemolytic anaemias Secondary polycythemia Severe exfoliative psoriasis Gaucher’s disease Cytotoxic drugs Glucose-6 phosphate deficiency High purine diet overproduction Reduced uric acid secretion Renal failure Hypertension Drugs (diuretics, aspirin, ciclosporin) Lead nephropathy Alcohol Down’s Syndrome Myxoedema Beryllium poisoning |
Secondary gout is the consequence of the use of specific drugs or develops as a consequence of other disorders. Certain diseases are associated with enhanced nucleic acid turnover, for example, myeloproliferative and lymphoproliferative disorders, psoriasis and haemolytic anaemia, and can lead to hyperuricaemia. Renal mechanisms are responsible for the majority of hyperuricaemia in individuals with over production representing less than 10% of patients with gout. The kidney excretes about two-thirds of the uric acid produced daily with the remainder being eliminated via the biliary tract with subsequent conversion to soluble allantoin by colonic bacterial uricase. Approximately 90% of the daily load of urate filtered by the kidneys is re-absorbed. This re-absorption process is mediated by specific anion transporters such as URAT-1 which is located on the apical side of the renal proximal tubular cells and is an important determinant of urate re-absorption (Richette and Bardin, 2010). The URAT-1 transporter is targeted by a number of drugs including benzbromarone, probenecid, losartan and sulphinpyrazone.
Risk factors
Hyperuricaemia is one of the main risk factors for gout and occurs in about 15–20% of the population (Doherty, 2009). Fortunately, only a minority of individuals with increased serum uric acid levels develop gout suggesting the importance of other contributing factors (Box 54.1).
Box 54.1 Risk factors for gout
Co-morbidities, for example, obesity, dyslipidaemia, glucose intolerance, hypertension
Genetics
Common primary gout in men often shows a strong familial predisposition, although the genetic basis for this is not fully understood. A polymorphism of the SLC22A12 gene which encodes for URAT-1 has been associated with under excretion of uric acid and hyperuricaemia in German Caucasians (Graessler et al., 2006). While in a Japanese cohort, another mutation of the SLC22A12 gene has been shown to be protective for the development of gout (Taniguchi et al., 2005).
The recently identified glucose and fructose transporter (GLU9) also acts as a high-capacity urate transporter in the proximal renal tubules (Dalbeth and Merriman, 2009). Polymorphism in the gene which encodes for this transporter (SLC2A9) has been reported to influence serum uric acid levels, and a significant association with self-reported gout has been described (Dalbeth and Merriman, 2009).
Renal disease
Gout is frequently associated with kidney disease, each being a risk factor for the other. Hyperuricaemia is associated with primary kidney disease, but kidney damage may arise secondary to gout as a consequence of the deposition of urate crystals in the interstitium and tubules of the kidney. Historically, gout was associated with significant renal impairment; however, progressive renal failure directly due to gout is now rare and mainly limited to inadequately treated patients with primary purine overproduction associated with purine enzyme defects, rare forms of inherited renal disease, chronic lead intoxication and renal disease as a consequence of uncontrolled disease states associated with gout e.g. hypertension, type 2 diabetes and congestive cardiac failure. Men with gout have a two-fold higher risk of kidney stones than patients without gout (Jordan et al., 2007). The likelihood of stones increases with serum urate concentration, extent of urinary acid secretion and low urine pH.
Co-morbidities
Metabolic syndrome is a multiplex risk factor for atherosclerotic cardiovascular disease that consists of atherogenic dyslipidaemia, raised blood pressure, increased blood glucose, and both prothrombotic and pro-inflammatory states. In the USA, metabolic syndrome is present in 63% of those with gout compared to 25% of those without gout (Choi et al., 2007). Other studies have shown obesity, weight gain and hypertension all to be independent risk factors for the development of gout (Choi et al., 2005).
Diet
Gout has often been associated with a rich lifestyle and excesses in diet. In particular, gout is higher in people who consume large quantities of red meat. There is also an increased risk associated with seafood consumption, but to a lesser extent than with red meat. In contrast, a diet high in purine-rich vegetables does not increase the risk, and the consumption of low-fat dairy products reduces the relative risk of gout with each additional dairy serving. The consumption of soft drinks sweetened with sugar (not diet drinks) has also been linked to an increase in the number of gout cases particularly in USA (Choi and Curham, 2008). The mechanism of action is thought to be an increase in uric acid levels caused by an increase in adenine nucleotide degradation. Vitamin C (ascorbic acid) has been shown to have a modest uricosuric effect (Huang et al., 2005). The consumption of cherries, but no other fruits, has also been shown to decrease uric acid levels.
Alcohol
Increased daily consumption of alcohol is associated with a higher risk of gout. Beer carries the greatest risk, probably due to its high purine content, followed by spirits. However, a moderate consumption of wine is not associated with an increased risk of developing gout (Jordan et al., 2007). The mechanism of action involved is thought to be the metabolism of ethanol to acetyl coenzyme A leading to adenine nucleotide degradation, with resultant increased formation of adenosine monophosphate, a precursor of uric acid. Alcohol also raises lactic acid levels in blood, which inhibits uric acid excretion.
Medication
A number of drugs are associated with increased uric acid levels (Box 54.2). The use of both loop and thiazide diuretics is the most common modifiable risk factor for secondary gout, especially in the elderly. It is thought loop and thiazide diuretics may precipitate an attack via volume depletion and reduced renal tubular secretion of uric acid. Aspirin has a bimodal effect; low doses inhibit uric acid excretion and increase urate levels, while doses greater than 3 g/day are uricosuric.
The prescribing of ciclosporin in organ transplant patients is an independent risk factor for new-onset gout in this group. The proposed mechanism of action is the interaction of ciclosporin with the hOAT10 transporter that mediates urate/glutathione exchange in the kidney (Bahn et al., 2008). Radiotherapy and chemotherapy in patients with neoplastic disorders can cause hyperuricaemia because of increased cell breakdown; to overcome this, prophylactic treatment may be given with allopurinol, commencing 3 days before therapy.
Presentation and diagnosis
The shed crystals are phagocytosed by monocytes and macrophages, activating the NACHT–LRR–PYD-containing protein-3 (NALP3) inflammasome and triggering the release of interleukin-1β (IL-1β) and other cytokines, a subsequent infiltration of neutrophils and the symptoms of an acute attack (Dalbeth and Haskard, 2005). The NALP3 inflammasome (cryopyrin) is a complex of intracellular proteins that is activated on exposure to microbial elements, such as bacterial RNA and toxins. Activation of NALP3 leads to the release of caspase-1, which is required for cleavage of pro-IL-1β to active IL-1β (Richette and Bardin, 2009). IL-1β has been shown to be critically associated with the inflammatory response induced by monosodium urate crystals (Rider and Jordan, 2010).
A third of patients will have normal uric acid concentrations during an acute attack of gout due to increased urinary urate excretion. The most appropriate time to measure serum urate for monitoring purposes is when the attack has completely resolved. The gold standard for the diagnosis of gout is the demonstration of urate crystals in synovial fluid or in a tophus by polarised light microscopy (Zhang et al., 2006). Crystals may be found in fluid aspirated from non-inflamed joints, even in those joints which have not previously experienced an attack. The crystals are large (10–20 μm) and needle shaped with a strong, intense, characteristic light pattern under polarised light. In contrast, the calcium pyrophosphate dehydrate crystals associated with pseudo-gout are small rhomboid crystals of low intensity. Gout and septic arthritis may co-exist and in order to exclude septic arthritis synovial fluid is sent for Gram staining and culture.
Course of disease
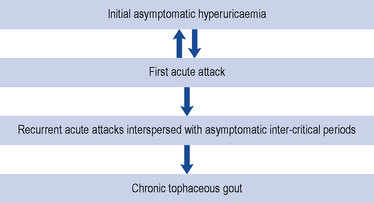
The course of gout follows a number of stages; initially, the patient may be asymptomatic with a raised serum uric acid level (Fig. 54.2). Some patients may only ever experience one attack, but often a second attack occurs within 6–12 months. Subsequent attacks tend to be of longer duration, affect more than one joint and may spread to the upper limbs. Untreated disease can result in chronic tophaceous gout, with persistent low-grade inflammation in a number of joints resulting in joint damage and deformity. The disease is characterised by the presence of tophi (Fig. 54.3), monosodium urate crystals surrounded by chronic mononuclear and giant-cell reactions. Tophi deposition can occur anywhere in the body, but they are commonly seen on the helix of the ear, within and around the toe or finger joints, on the elbow, around the knees or on the Achilles tendons. The skin overlying the tophi may ulcerate and extrude white, chalky material composed of monosodium urate crystals.
Treatment
The management of gout can be split into the rapid resolution of the initial acute attack and long-term measures to prevent future episodes (see Box 54.3).
Box 54.3 Treatment aims in gout
Rapid alleviation of the acute attack
Lower serum uric acid levels to below saturation point
Reduce risk of co-morbidities, for example, cardiovascular disease
Management of an acute attack
Drugs used in the management of an acute attack include NSAIDs, colchicine and corticosteroids. NSAIDs are the recommended first-line agents, but in a number of patients their use is contraindicated and a second-line agent is indicated (Box 54.4). Where the pain is not adequately controlled by treatment, paracetamol and weak opiate analgesics, for example, codeine or dihydrocodeine may be added to the regimen to provide additional relief. Treatment should be continued until the attack is terminated, usually between 1 and 2 weeks. The affected joints should also be rested for 1–2 days and initially treated with ice which has a significant analgesic effect during an acute attack.
A complete medication review should be performed, and ideally medication which is likely to have contributed to the attack discontinued. Where loop and thiazide diuretics are being used for the management of hypertension alone, an alternative anti-hypertensive agent should be considered according to national guidance. Losartan, an angiotensin receptor blocker effective in hypertension, has been shown to have uricosuric properties and is a suitable agent in hypertensive patients with gout (Sica and Schoolwerth, 2002; Takahashi et al., 2003). In patients with heart failure, diuretics are often essential and cannot be discontinued. Certain NSAIDs may be preferable in patients on diuretics with both indometacin and azapropazone (no longer licensed in the UK) demonstrating an increase uric acid secretion. Moreover, the diuretic effect of furosemide appears unaffected by azapropazone and azapropazone’s ability to promote uric acid secretion is sustained (Williamson et al., 1984).
Non-steroidal anti-inflammatory drugs
Although the NSAIDs differ in chemical structure, they all have similar pharmacological properties in terms of anti-inflammatory and analgesic action, and have similar drug interactions. For a number of years, indometacin was considered the NSAID of choice in gout largely because it was one of the first NSAIDs shown to be effective in the management of gout. However, it has not been shown to be of superior efficacy or safety when compared to other NSAIDs used in the management of acute gout (Jordan et al., 2007).
In an effort to reduce the side effects of NSAIDs, and particularly the gastro-intestinal side effects, agents were developed to selectively block COX-2 and have minimal effect on COX-1. COX-2 selective agents are recommended for use in patients who are at high risk of developing gastro-intestinal side effects, but they are not recommended for routine use. It should be noted that the selective benefit of COX-2 inhibitors is lost in patients taking low dose aspirin. The selective COX-2 inhibitor etoricoxib in a daily dose of 120 mg has been shown to give comparable rapid relief of pain in acute gout to indometacin 50 mg three times daily but with fewer side effects (Schumacher et al., 2002). However, a systematic review and meta-analysis of studies involving etoricoxib have demonstrated an increased risk of cardiovascular thromboembolic events (Aldington et al., 2005). Although there are currently no data directly comparing the cardiovascular risk associated with selective and non-selective NSAIDs, it is recommended that the use of COX-2 inhibitors is avoided in patients with established heart disease, cerebrovascular disease or peripheral vascular disease.
Colchicine
Although the mode of action of colchicine in gout is not fully understood, it is thought to arrest microtubule assembly in neutrophils and inhibit many cellular functions. It suppresses monosodium urate crystal-induced NALP3 inflammasome-driven caspase-1 activation, IL-1β processing and release, and L-selectin expression on neutrophils. Colchicine also blocks the release of a crystal-derived chemotactic factor from neutrophil lysosomes, blocks neutrophil adhesion to endothelium by modulating the distribution of adhesion molecules on the endothelial cells and inhibits monosodium urate crystal-induced production of superoxide anions from neutrophils (Nuki, 2008).
Although widely used, there are few studies that demonstrate the efficacy of colchicine. A single, randomised, controlled trial has compared the benefits of colchicine to placebo in acute gouty flare (Ahern et al., 1987). Patients were given 1 mg of colchicine followed by 500 μcg every 2 h until the attack stopped or they felt too ill to continue taking colchicine. Colchicine was found to be superior to placebo with an absolute reduction of 34% for pain and a 30% reduction in clinical symptoms such as palpation, swelling, redness and pain. The number needed to treat (NNT) with colchicine to reduce pain was 3 and the NNT to reduce clinical symptoms was 2. All participants given colchicine experienced gastro-intestinal side effects such as diarrhoea and/or vomiting. There are no studies comparing colchicine to either NSAIDs or corticosteroids in an acute flare of gout.
The current dose of colchicine licensed for the management of an acute attack of gout is 1 mg initially, followed by 500 μcg every 2–3 h until relief of pain is obtained or vomiting or diarrhoea occurs. A maximum of 6 mg should be given per course and treatment should not be repeated within 3 days. This dosage regimen frequently causes diarrhoea and other toxic side effects, particularly in elderly patients (Morris et al., 2003; Terkeltaub et al., 2008). It is therefore recommended that a dose of 500 μcg given twice or four times a day should be used to reduce toxicity. Intravenous colchicine is no longer licensed in the UK because use has been associated with a number of fatalities (2% mortality rate).
Corticosteroids
Intramuscular triamcinolone acetonide 60 mg has been shown to be as safe and effective as indometacin 50 mg three times daily in treating an acute attack of gout with earlier resolution of symptoms in the steroid group (Alloway et al., 1993). Common doses of intra-articular steroids are 80 mg of methylprednisolone acetate for a large joint such as a knee; 40 mg of methylprednisolone acetate or 40 mg of triamcinolone acetonide for a smaller joint such as a wrist or elbow. Oral prednisolone 30 mg daily for 5 days has also been shown to be equally efficacious to indometacin 50 mg three times a day for 2 days or 25 mg three times a day for 3 days plus paracetamol and has fewer adverse events (Man et al., 2007). Oral steroid regimens used in practice include prednisolone 30 mg daily for 1–3 days with subsequent dose tapering over 1–2 weeks. Intramuscular steroid injections (methylprednisolone acetate 80–120 mg) may sometimes be used to prevent the precipitation of a flare on initiation of prophylactic treatment for gout. Corticosteroids may have fewer adverse events than other acute treatments when used short term, particularly in the elderly.
Interleukin-1 inhibitors
IL-1β is critically associated with the inflammatory response induced by monosodium urate crystals (Rider and Jordan, 2010). Anakinra, an IL-1 receptor antagonist, has been shown to reduce the pain of gout and bring about complete resolution by day 3 in the majority of patients after a course of three 100-mg subcutaneous injections (McGonagle et al., 2007; So et al. 2007). Other IL-1 inhibitors, such as rilonacept, are under development.
Management of chronic gout
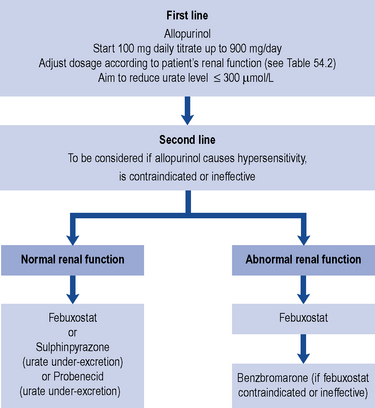
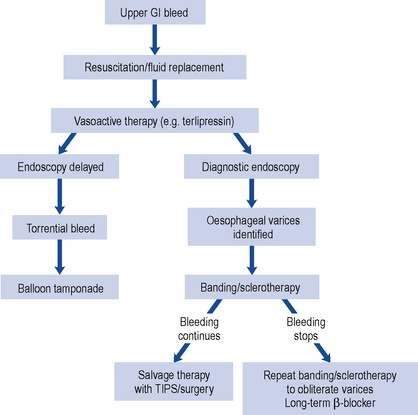
The presence of hyperuricaemia is not an indication to commence prophylactic therapy. Some patients may only experience a single episode and a change in lifestyle, diet or concurrent medication may be sufficient to prevent further attacks. Patients who suffer one or more acute attacks within 12 months of the first attack should normally be prescribed prophylactic urate-lowering therapy (see Fig. 54.4). There are, however, some groups of patients where prophylactic therapy should be instigated after a single attack. These include individuals with uric acid stones, the presence of tophi at first presentation and young patients with a family history of renal or cardiac disease. The criteria for starting prophylactic therapy for gout is detailed in Box 54.5.
Box 54.5 Criteria for starting prophylactic therapy for gout
One or more acute attacks within 12 months of the first attack
Tophi present at the first presentation of an acute attack
Need to continue medication associated with raised uric acid levels, for example diuretics
Young patients with a family history of renal or cardiac disease
Drugs that lower serum uric acid can be classified into three groups according to their pharmacological mode of action (Box 54.6).
Box 54.6 Classification of prophylactic agents used to lower serum urate
Uricostatic agents: allopurinol, febuxostat
Uricosuric agents: benzbromarone, probenecid, sulphinpyrazone
Uricostatic agents
Uricostatic agents act on the enzyme xanthine oxidase. Xanthine oxidase catalyses the oxidation of hypoxanthine to xanthine and subsequently xanthine to uric acid (Fig. 54.1). Hypoxanthine comes from the catabolism of cellular nucleoproteins and purine nucleotides. Blocking the action of this enzyme reduces the production of uric acid. Agents in this group include allopurinol and febuxostat.
Allopurinol
Allopurinol is the prophylactic agent of choice in the management of recurrent gout. In order to become pharmacologically active, allopurinol must be metabolised by the liver to oxypurinol. Oxypurinol has a much longer half-life than allopurinol, 14–16 h compared to 2 h. Both allopurinol and oxypurinol are renally excreted, with oxypurinol undergoing re-absorption from the renal tubule. In patients with reduced renal function, the half-life of oxypurinol is increased with the risk of accumulation and toxicity. It is, therefore, essential that a patient’s renal function is checked prior to the prescribing of allopurinol and the dose adjusted accordingly (Table 54.2).
Table 54.2 Recommended dose of allopurinol in patients with diminished renal function
| Creatinine clearance (mL/min) | Dose |
|---|---|
| 0 | 100 mg three times a week |
| 10 | 100 mg alternate days |
| 20 | 100 mg daily |
| 40 | 150 mg daily |
| 60 | 200 mg daily |
| >100 | 300 mg daily |
Febuxostat
Febuxostat is a more selective and potent inhibitor of xanthine oxidase than allopurinol and has no effect on other enzymes involved in purine or pyrimidine metabolism (Lawrence Edwards, 2009). It is licensed for the treatment of chronic hyperuricaemia in conditions where urate deposition has already occurred including a history, or presence of, tophus and/or gouty arthritis. It is recommended as a second-line agent in patients who are intolerant of allopurinol or for whom allopurinol is contraindicated.
Febuxostat is more effective than fixed-dose allopurinol 300 mg in lowering uric acid concentrations in trials of up to 40 months’ duration (Schumacher et al., 2008, 2009). However, a reduction in the incidence of episodes of acute gout has not been demonstrated.
Uricosuric agents
Benzbromarone
Benzbromarone has been shown to be effective in lowering serum urate levels and reducing the time to resolution of tophi (Kumar et al., 2005; Reinders et al. 2009). However, its use was associated with hepatoxicity and it was withdrawn from the UK. It is still possible to obtain benzbromarone on a named patient basis. The risk of hepatotoxicity has been estimated to be 1:17,000 patients. For those who are prescribed benzbromarone, regular liver function tests must be performed during the first 6 months of therapy, and the hepatotoxic risk associated with the medicine should be clearly explained to the patient at the outset.
The dose ranges from 50 to 200 mg daily. It remains active in mild to moderate renal impairment and is indicated where there is a contraindication to other agents used in the management of gout such as allopurinol and febuxostat (see Fig. 54.4). Diarrhoea may be troublesome in approximately 10% of patients.
Patient care
It is important to inform patients about the disease, its curable nature, the aims of drug therapy and how to prevent and handle flares. The need for dietary and lifestyle changes should also be stressed. The UK Gout Society website can assist in providing patients with information about the condition and how it should be managed (http://www.ukgoutsociety.org/). In over-weight patients, gradual weight loss should be encouraged, very rapid weight loss should be avoided as it can cause ketosis and result in raised uric acid levels with the likelihood of precipitating an attack. Low purine diets are difficult to adhere to; a calorie-restricted diet with low carbohydrate (40% of energy), high protein (30% of energy) and unsaturated fat (30% of energy) should be recommended. The importance of avoiding or reducing alcohol consumption should also be emphasised.
Answers
As previously discussed, Mr TH should also moderate his alcohol consumption.
Answers
Answers
Ahern M.J., Reid C., Gordon T.P., et al. Does colchicine work? The results of the first controlled study in acute gout. Aust. N. Z. J. Med.. 1987;17:301-304.
Aldington S., Shirtcliffe P., Weatherall M., et al. Systematic review and meta-analysis of the risk of major cardiovascular events with etoricoxib therapy. N. Z. Med. J.. 2005;118(1223):U1684.
Alloway J.A., Moriarty M.J., Hoogland Y.T., et al. Comparison of traimcinolone acetonide with indomethacin in the treatment of acute gouty arthritis. J. Rheumatol.. 1993;20:111-113.
Bahn A., Hagos Y., Reuter S., et al. Identification of a new urate and high affinity nicotinate transporter, hOAT10 (SLC22A13). J. Biol. Chem.. 2008;283:16332-16341.
Choi H.K., Curham G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. Br. J. Med.. 2008;336:309-312.
Choi H.K., Atkinson K., Karlson E.W., et al. Purine rich foods, dairy and protein intake, and the risk of gout in men. N. Engl. J. Med.. 2004;350:1093-1103.
Choi H.K., Atkinson K., Karlson E.W., et al. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Arch. Int. Med.. 2005;165:742-748.
Choi H.K., Ford E.S., Li C., et al. Prevalence of metabolic syndrome in patients with gout: the Third National Health and Nutrition Examination Survey. Arthritis Rheum.. 2007;57:109-115.
Dalbeth N., Haskard D.O. Mechanisms of inflammation in gout. Rheumatology. 2005;44:1090-1096.
Dalbeth N., Merriman T. Crystal ball gazing: new therapeutic targets for hyperuricaemia and gout. Rheumatology. 2009;48:222-226.
Doherty H. New insights into the epidemiology of gout. Rheumatology. 2009;49:613-614.
Lawrence Edwards N. Febuxostat: a new treatment for hyperuricaemia in gout. Rheumatology. 2009;48(Suppl. 2):ii15-ii19.
Graessler J., Graessler A., Unger S., et al. Association of the human urate transporter 1 with reduced renal uric acid excretion in a German Caucasian population. Arthritis Rheum.. 2006;54:292-300.
Huang H.Y., Appel L.J., Choi M.J., et al. The effects of vitamin C supplementation on serum concentrations of uric acid: results of a randomized controlled trial. Arthritis Rheum.. 2005;52:1843-1847.
Jordan K.M., Cameron S., Snaith M., on behalf of the British Society for Rheumatology and British Health Professionals in Rheumatology Standards, Guidelines and Adult Working Group (SGAWG). British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of gout. Rheumatology. 2007. doi:10.1093/rheumatology/kem056b
Kumar S., Ng J., Gow P. Benzbromarone therapy in management of refractory gout. N. Z. Med. J.. 2005;118(1217):U1528.
Man C.Y., Cheung I., Cameron I., et al. Comparison of oral prednisolone/paracetamol and oral indomethacin/paracetamol combination therapy in the treatment of acute gout like arthritis: a double blind randomized, controlled trial. Ann. Emerg. Med.. 2007;49:670-677.
McGonagle D., Tan A.L., Shankaranarayana S., et al. Management of treatment resistant inflammation of acute or chronic tophaceous gout with anakinra. Ann. Rheum. Dis.. 2007;66:1683-1684.
Morris I., Varughese G., Mattingly P. Lesson of the week – colchicine in acute gout. Br. Med. J.. 2003;327:1275-1276.
Nuki G. Colchicine: its mechanism of action and efficacy in crystal-induced inflammation. Curr. Rheumatol. Rep.. 2008;10:218-227.
Reinders M.K., Haagsma C., Jansen T.L., et al. A randomised controlled trial on the efficacy and tolerability with dose escalation of allopurinol 300–600mg/day versus benzbromarone 100–200mg/day in patients with gout. Ann. Rheum. Dis.. 2009;68:892-897.
Richette P., Bardin T. Gout. Lancet. 2010;375:318-328.
Rider T.G., Jordan K.M. The modern management of gout. Rheumatology. 2010;49:5-14.
Schumacher H.R., Boice J.A., Daikh D.I., et al. Randomised double blind trial of etoricoxib and indometacin in treatment of acute gouty arthritis. Br. Med. J.. 2002;324:488-492.
Schumacher H.R., Becker M.A., Wortmann R.L., et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricaemia and gout: a 28-week, phase III, randomized, double blind, parallel-group trial. Arthritis Rheum.. 2008;59:1540-1548.
Schumacher H.R., Becker M.A., Lloyd E., et al. Febuxostat in the treatment of gout; 5-yr findings of the FOCUS efficacy and safety study. Rheumatology. 2009;48:188-194.
Sica A.D., Schoolwerth A.C. Part 1. Uric acid and losartan. Curr. Opin. Nephrol. Hypertens. 2002;11:475-482.
So A., De Smedt T., Revas S., et al. A pilot study of IL-1 inhibition by anakinra in acute gout. Arthritis Res. Ther.. 2007;9:R28.
Takahashi S., Moriwaki Y., Yamamoto T., et al. Effects of combination treatment using anti-hyperuriaemic agents with fenofibrate and/or losartan on uric acid metabolism. Arthritis Res. Ther.. 2003;72:671-674.
Taniguchi A., Urano W., Yamanaka M., et al. A common mutation in an organic anion transporter gene SLC22A12, is a suppressing factor for the development of gout. Arthritis Rheum.. 2005;52:2576-2577.
Terkeltaub R., Furst D.E., Bennett K., et al. Low dose (1.8 mg) vs high dose (4.8 mg) oral colchicine regimens in patients with acute gout flare in a large, multicentre, randomized, double-blind, placebo controlled, parallel group study. Arthritis Rheum.. 2008;58(Suppl. 9):1944.
Williamson P.J., Ene M.D., Roberts C.J. A study of the potential interactions between azapropazone and frusemide in man. Br. J. Clin. Pharmacol.. 1984;18:619-623.
Zhang W., Doherty M., Pascual E., et al. EULAR evidence based recommendations for gout. Part I: diagnosis. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann. Rheum. Dis.. 2006;65:1301-1311. doi 10.1136/ard.2006.055251
Choi H.K., Mount D.B., Reginato A.M. Pathogenesis of gout. Ann. Int. Med.. 2005;143:499-516.
National Institute for Health and Clinical Excellence. Febuxostat for the management of hyperuricaemia in people with gout, Technology Appraisal No. 164. London: NICE. 2008. Available from http://www.nice.org.uk/nicemedia/live/12101/42738/42738.pdf
Zhang W., Doherty M., Bardin T., et al. EULAR evidence based recommendations for gout. Part II: management. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann. Rheum. Dis.. 2006;65:1312-1324. doi 10.1136/ard.2006.055269