Chapter 505 Glomerulonephritis Associated with Infections
505.1 Acute Poststreptococcal Glomerulonephritis
Pathology
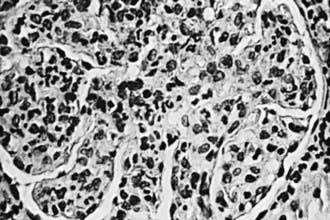
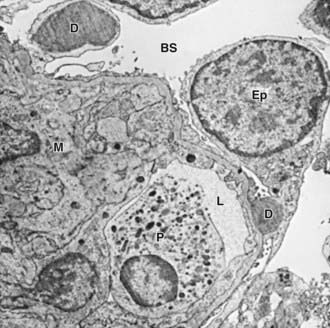
The kidneys appear symmetrically enlarged. Glomeruli appear enlarged and relatively bloodless and show diffuse mesangial cell proliferation, with an increase in mesangial matrix (Fig. 505-1). Polymorphonuclear leukocyte infiltration is common in glomeruli during the early stage of the disease. Crescents and interstitial inflammation may be seen in severe cases, but these changes are not specific for poststreptococcal GN. Immunofluorescence microscopy reveals a pattern of “lumpy-bumpy” deposits of immunoglobulin and complement on the glomerular basement membrane (GBM) and in the mesangium. On electron microscopy, electron-dense deposits, or “humps,” are observed on the epithelial side of the GBM (Fig. 505-2).
Diagnosis
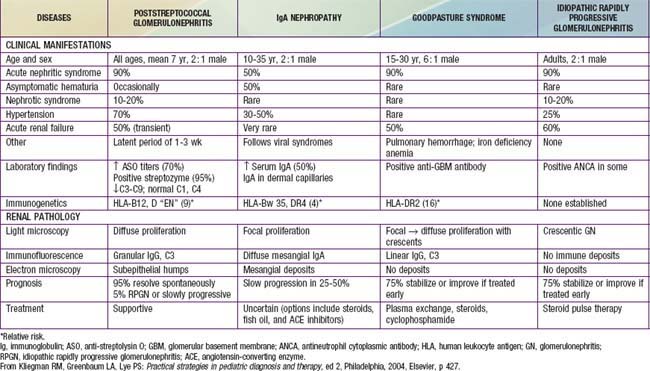
The differential diagnosis of poststreptococcal GN includes many of the causes of hematuria listed in Tables 503-2 and 505-1 and an algorithm to help with diagnosis is presented in Figure 505-3. Acute postinfectious GN can also follow other infections with coagulase-positive and coagulase-negative staphylococci, Streptococcus pneumoniae, and gram-negative bacteria. Bacterial endocarditis can produce a hypocomplementemic GN with renal failure. Acute GN can occur after certain fungal, rickettsial, and viral diseases, particularly influenza.
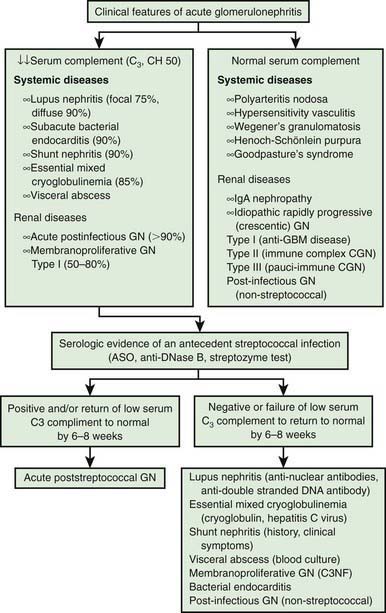
Figure 505-3 Differential diagnosis of acute glomerulonephritis (GN). ASO, anti-streptolysin O; GBM, glomerular basement membrane.
(Adapted from Sulyok E: Acute proliferative glomerulonephritis. In Avner ED, Harmon WE, Niaudet P, editors: Pediatric nephrology, ed 5, Philadelphia, 2004, Lippincott Williams & Wilkins, pp 601–613.)
Treatment
Management is directed at treating the acute effects of renal insufficiency and hypertension (Chapter 529.1). Although a 10-day course of systemic antibiotic therapy with penicillin is recommended to limit the spread of the nephritogenic organisms, antibiotic therapy does not affect the natural history of GN. Sodium restriction, diuresis usually with intravenous furosemide, and pharmacotherapy with calcium channel antagonists, vasodilators, or angiotensin-converting enzyme inhibitors are standard therapies used to treat hypertension.
Ahn SY, Ingulli E. Acute poststreptococcal glomerulonephritis: an update. Curr Opin Pediatr. 2008;20:157-162.
Clark G, White RHR, Glasgow EF, et al. Poststreptococcal glomerulonephritis in children: clinicopathological correlations and long-term prognosis. Pediatr Nephrol. 1988;2:381-388.
Pais PJ, Kump T, Greenbaum LA. Delay in diagnosis in poststreptococcal glomerulonephritis. J Pediatr. 2008;153:560-564.
Rodriquez-Iturbe B, Mezzano S. Acute postinfectious glomerulonephritis. In: Avner ED, Harmon WE, Niaudet P, et al, editors. Pediatric nephrology. ed 6. Heidelburg, Germany: Springer-Verlag; 2009:743-756.
White AV, Hoy WE, McCredie DA. Childhood post-streptococcal glomerulonephritis as a risk factor for chronic renal disease in later life. Med J Aust. 2001;10:492-496.
505.2 Other Chronic Infections
Chesney RW, O’Regan S, Guyda HJ, et al. Candida endocrinopathy syndrome with membranoproliferative glomerulonephritis: demonstration of glomerular Candida antigen. Clin Nephrol. 1976;5:232-238.
Connor FL, Rosenberg AR, Kennedy SE, et al. HBV associated nephrotic syndrome: resolution with oral lamivudine. Arch Dis Child. 2003;88:446-449.
Hendrickse RG, Adeniyi A. Quartan malarial nephrotic syndrome in children. Kidney Int. 1979;16:64-74.
Hunte W, Al-Ghraoui F, Cohen RJ. Secondary syphilis and the nephrotic syndrome. J Am Soc Nephrol. 1993;3:1351-1355.
Meyers CM, Seeff LB, Stehman-Breen CO, et al. Hepatitis C and renal disease: an update. Am J Kidney Dis. 2003;42:631-657.
Naicker S, Fabian J, Naidoo S, et al. Infection and glomerulonephritis. Semin Immunopathol. 2007;29:397-414.
Nasr SH, Markowitz GS, Stokes MB, et al. Acute postinfectious glomerulonephritis in the modern era. Medicine. 2008;87:21-32.
Neugarten J, Baldwin DS. Glomerulonephritis in bacterial endocarditis. Am J Med. 1984;77:297-304.
Ozdamar SO, Gucer S, Tinaztepe K. Hepatitis-B virus associated nephropathies: a clinicopathological study in 14 children. Pediatr Nephrol. 2003;181:23-28.
Ray PE, Xu L, Rakusan T, et al. A 20-year history of childhood HIV-associated nephropathy. Pediatr Nephrol. 2004;10:1075-1092.
Vella J, Carmody M, Campbell E, et al. Glomerulonephritis after ventriculo-atrial shunt. Q J Med. 1995;88:911-918.