12 Gastrointestinal system
Symptoms of gastrointestinal disease
The common symptoms of GI and abdominal disease are listed in Box 12.1 and are discussed individually below.
Abdominal pain
Abdominal pain is a common symptom which often accompanies serious diagnoses but frequently has no definable cause. As with any pain, it is important to characterize its site, intensity, character, areas of radiation, duration and frequency, together with aggravating and relieving factors and associated features. The particular clinical problem of acute abdmominal pain is discussed on page 237-238. The particular characteristics of pain from certain frequent and important causes are given in Box 12.2. Pain that comes in waves is described as being colicky. These waves are more frequent in pain from the gut, but vary over a longer time period when pain is from the biliary or renal tract. Abdominal pain may be due to causes that are not specifically in the abdomen such as metabolic disorders (porphyria or lead poisoning) or depression.
Box 12.2 Particular characteristics of pain from frequent and important causes (the regions of the abdomen are shown in Fig. 12.5 – the loin is lateral and posterior to the lumbar area)
 Peptic ulcer: epigastric, burning or gnawing, radiates through to back, meal related, wakes the patient, relieved by antacid
Peptic ulcer: epigastric, burning or gnawing, radiates through to back, meal related, wakes the patient, relieved by antacid
 Gastric cancer: epigastric, severe, partly meal related, not relieved by antacid
Gastric cancer: epigastric, severe, partly meal related, not relieved by antacid
 Pancreatic: high epigastric, severe, felt front-to-back, immediately after eating, relieved by sitting forward
Pancreatic: high epigastric, severe, felt front-to-back, immediately after eating, relieved by sitting forward
 Midgut: periumbilical, colicky, some relation to meals
Midgut: periumbilical, colicky, some relation to meals
 Lower gut: periumbilical or suprapubic, colicky, some relief from bowel action
Lower gut: periumbilical or suprapubic, colicky, some relief from bowel action
 Biliary: right upper quadrant, severe, colicky (but over a long time period), radiates to right shoulder, accompanied by nausea
Biliary: right upper quadrant, severe, colicky (but over a long time period), radiates to right shoulder, accompanied by nausea
 Renal colic: loin-to-groin, colicky, very severe, accompanied by nausea
Renal colic: loin-to-groin, colicky, very severe, accompanied by nausea
 Functional: anywhere in the abdomen, colicky, accompanied by bloating, relieved by bowel action
Functional: anywhere in the abdomen, colicky, accompanied by bloating, relieved by bowel action
Nutritional assessment
A full examination will include most signs of general and nutrient-specific malnutrition. Some detail of the latter is given in Table 12.1. Body weight is a key part of general examination as is height. These two can be related together and to a standard range by calculating the body mass index (BMI or Quetelet index). This is defined by the body weight (in kilograms), divided by the height (in metres) squared. The World Health Organization (WHO) classification of this index is given in Table 12.2. In the UK, the range 20-25 is often regarded as desirable, but the lower level of 18.5 is more applicable internationally. Patients with an index of more than 30 should undergo weight loss. In malnourished children, retardation of height lags behind that of weight and the relation between weight and height should always be compared with age using appropriate charts.
Table 12.1 Principal symptoms and signs due to vitamin and mineral deficiencies
| Nutrients | Deficiency syndrome | Principal symptoms/signs |
|---|---|---|
| Vitamin A, retinol (carotenoids) | Night blindness, keratomalacia | |
| Vitamin B1, thiamine | Wernicke/Korsakoff, beriberi | Nystagmus, sixth cranial nerve palsy, ataxia, acidosis, dementia, paraesthesiae, neuropathy and cardiac failure |
| Vitamin B2, riboflavin | Ariboflavinosis | Angular stomatitis, glossitis, magenta tongue |
| Niacin, nicotinic acid | Pellagra | Dermatitis of sun-exposed areas, dementia, poor appetite, difficulty sleeping, confusion, sore mouth |
| Vitamin B6, pyridoxine | Poor appetite, lassitude, oxaluria | |
| Pantothenic acid | Nausea, abdominal pain, paraesthesiae, burning feet | |
| Biotin | Dermatitis, depression, lassitude, muscle pains, electrocardiogram abnormalities, blepharitis | |
| Folic acid | Macrocytic anaemia, thrombocytopenia and megaloblastic bone marrow | |
| Vitamin B12 | Subacute combined degeneration, macrocytic anaemia | |
| Vitamin C, ascorbic acid | Scurvy | Poor wound healing, fatigue, limb pain, shortness of breath, difficulty sleeping, gingivitis, perifollicular purpura, hyperkeratosis |
| Vitamin D, ergo-/cholecalciferol | Rickets/osteomalacia | Bone pain, proximal myopathy |
| Vitamin E, tocopherol | Haemolysis, posterior column signs, ataxia, muscle wasting, retinitis pigmentosa-like changes, night blindness | |
| Vitamin K, phylloquinone and other menaquinones | Bruising, purpura, nose and GI bleeds | |
| Trace elements | ||
| Iron | Koilonychia, smooth tongue, anaemia, oesophageal web | |
| Zinc | Acrodermatitis enteropathica | Peristomal/perinasal/perineal erythema, thin hair, diarrhoea, apathy, anorexia, growth failure, hypoglycaemia |
| Copper | Microcytic hypochromic anaemia, neutropenia, scurvy-like bone lesions, osteoporosis | |
| Chromium | Peripheral neuropathy, hyperglycaemia | |
| Selenium | Cardiomyopathy | |
| Iodine | Goitre | |
Table 12.2 World Health Organization classification of body weight
| Category | BMI/Quetelet index |
|---|---|
| Underweight | <18.5 |
| Healthy weight | 18.5-24.9 |
| Overweight | 25-29.9 |
| Moderately obese | 30-34.9 |
| Severely obese | 35-39.9 |
| Morbidly obese | >40 |
Physical examination of the GI tract and abdomen
General signs
Systemic features of GI disease may be evident on general examination. Peripheral signs of chronic liver disease are listed in Box 12.3. Of these, the most common and useful are spider naevi (Fig. 12.1) (the presence of up to five small ones can be normal) and palmar erythema (Fig. 12.2) (the blotchy appearance often being more important than the overall redness). Inflammatory bowel disease may give rise to clubbing of the hands, arthritis, uveitis and skin changes including erythema nodosum (tender raised red lumps on the extensor surface of the limbs) and the much rarer pyoderma gangrenosum. Anaemia accompanies many GI diseases, as does oedema, and lymphadenopathy can be secondary to GI malignancy.
Box 12.3 Peripheral stigmata (signs) of chronic liver disease
Skin, nails and hands
 Spider naevi – small telangectatic superficial blood vessels with a central feeding vessel
Spider naevi – small telangectatic superficial blood vessels with a central feeding vessel
 Leuconychia – expansion of the paler half-moon at the base of the nail
Leuconychia – expansion of the paler half-moon at the base of the nail
 Palmar erythema – seen on the thenar and hypothenar eminence – often with blotchy appearance
Palmar erythema – seen on the thenar and hypothenar eminence – often with blotchy appearance
 Dupytren’s contracture – can occur in the absence of liver disease
Dupytren’s contracture – can occur in the absence of liver disease
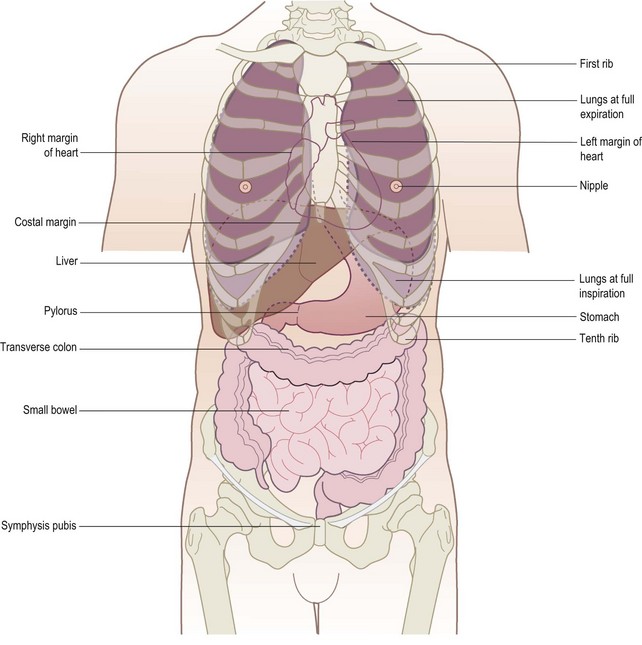
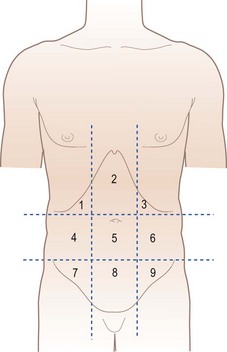
It is helpful when examining the patient, recording in notes or communicating information to colleagues to remember the surface anatomy of the structures related to the GI tract and abdomen (Figs 12.3 and 12.4) and to think of the abdomen as divided into regions (Fig. 12.5). The two lateral vertical planes pass from the femoral artery below to cross the costal margin close to the tip of the ninth costal cartilage. The two horizontal planes, the subcostal and interiliac, pass across the abdomen to connect the lowest points on the costal margin and the tubercles of the iliac crests, respectively.
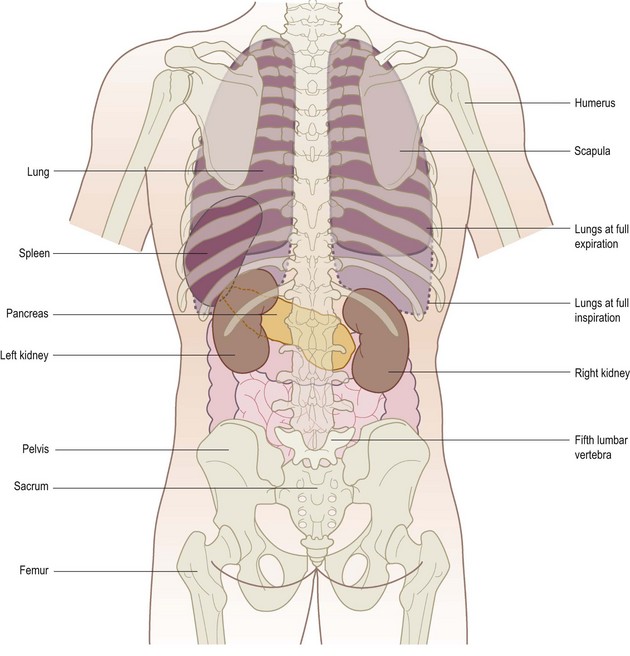
Figure 12.4 Posterior view of the external relations of the abdominal and thoracic organs. The liver is not shown.
Inspection
The patient should be lying supine with arms loosely at the sides, the head and neck supported by up to two pillows, sufficient for comfort (Fig. 12.6). A sagging mattress makes examination difficult, particularly palpation. Make sure there is a good light, that the room is warm and that the hands are warm. A shivering patient cannot relax and vital signs, especially on palpation, may be missed.
Shape
Is the abdomen of normal contour and fullness, or distended? Is it scaphoid (sunken)?
 Generalized fullness or distension may be due to fat, fluid, flatus, faeces or fetus.
Generalized fullness or distension may be due to fat, fluid, flatus, faeces or fetus.
 Localized distension may be symmetrical and centred around the umbilicus as in the case of small bowel obstruction, or asymmetrical as in gross enlargement of the spleen, liver or ovary.
Localized distension may be symmetrical and centred around the umbilicus as in the case of small bowel obstruction, or asymmetrical as in gross enlargement of the spleen, liver or ovary.
 Make a mental note of the site of any such swelling or distension; think of the anatomical structures in that region and note if there is any movement of the swelling, either with or independent of respiration.
Make a mental note of the site of any such swelling or distension; think of the anatomical structures in that region and note if there is any movement of the swelling, either with or independent of respiration.
 Remember that chronic urinary retention may cause palpable enlargement in the lower abdomen.
Remember that chronic urinary retention may cause palpable enlargement in the lower abdomen.
A scaphoid abdomen is seen in advanced stages of starvation and malignant disease.
Movements of the abdominal wall
Visible peristalsis of the stomach or small intestine may be observed in three situations:
1 Obstruction at the pylorus. Visible peristalsis may occur where there is obstruction at the pylorus produced either by fibrosis following chronic duodenal ulceration or, less commonly, by carcinoma of the stomach in the pyloric antrum. In pyloric obstruction, a diffuse swelling may be seen in the left upper abdomen but, where obstruction is longstanding with severe gastric distension, this swelling may occupy the left mid and lower quadrants. Such a stomach may contain a large amount of fluid and, on shaking the abdomen, a splashing noise is usually heard (’succussion splash’). This splash is frequently heard in healthy patients for up to 3 hours after a meal, so enquire when the patient last ate or drank. In congenital pyloric stenosis of infancy, not only may visible peristalsis be apparent but also the grossly hypertrophied circular muscle of the antrum and pylorus may be felt as a ‘tumour’ to the right of the midline in the epigastrium. Both these signs may be elicited more easily after the infant has been given a feed. Standing behind the child’s mother with the child held on her lap may allow the child’s abdominal musculature to relax sufficiently to feel the walnut-sized swelling.
2 Obstruction in the distal small bowel. Peristalsis may be seen where there is intestinal obstruction in the distal small bowel or coexisting large and small bowel hold-up produced by distal colonic obstruction, with an incompetent ileocaecal valve allowing reflux of gas and liquid faeces into the ileum. Not only is the abdomen distended and tympanitic (hyper-resonant) but the distended coils of small bowel may be visible in a thin patient and tend to stand out in the centre of the abdomen in a ‘ladder pattern’.
3 As a normal finding in very thin, elderly patients with lax abdominal muscles or large, wide-necked incisional herniae seen through an abdominal scar.
Skin and surface of the abdomen
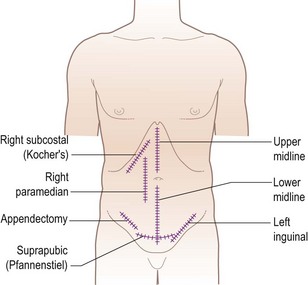
Note any scars present, their site, whether they are old (white) or recent (red or pink), linear or stretched (and therefore likely to be weak and contain an incisional hernia). Common examples are given in Fig. 12.7.
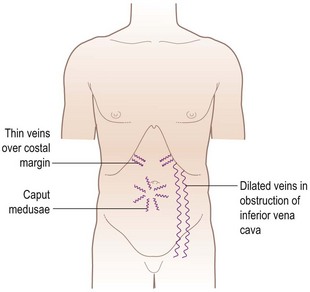
Look for prominent superficial veins, which may be apparent in three situations (Fig. 12.8): thin veins over the costal margin, usually of no significance; occlusion of the inferior vena cava; and venous anastomoses in portal hypertension. Inferior vena caval obstruction not only causes oedema of the limbs, buttocks and groins but, in time, distended veins on the abdominal wall and chest wall appear. These represent dilated anastomotic channels between the superficial epigastric and circumflex iliac veins below, and the lateral thoracic veins above, conveying the diverted blood from the long saphenous vein to the axillary vein; the direction of flow is therefore upwards. If the veins are prominent enough, try to detect the direction in which the blood is flowing by occluding a vein, emptying it by massage and then looking for the direction of refill. Distended veins around the umbilicus (caput medusae) are uncommon but signify portal hypertension, other signs of which may include splenomegaly and ascites. These distended veins represent the opening up of anastomoses between portal and systemic veins and occur in other sites, such as oesophageal and rectal varices.
Palpation
When palpating, the wrist and forearm should be in the same horizontal plane where possible, even if this means bending down or kneeling by the patient’s side. The best palpation technique involves moulding the relaxed right hand to the abdominal wall, not to hold it rigid (Fig. 12.9). The best movement is gentle but with firm pressure, with the fingers held almost straight but with slight flexion at the metacarpophalangeal joints and certainly avoiding sudden poking with the fingertips (Fig. 12.10).

Figure 12.9 Correct method of palpation. The hand is held flat and relaxed and ‘moulded’ to the abdominal wall.

Figure 12.10 Incorrect method of palpation. The hand is held rigid and mostly not in contact with the abdominal wall.
Palpation of intra-abdominal structures is an imperfect process in which the great sensitivity of the sense of touch and pressure is heavily masked by the abdominal wall tissue. It is unusual for structures to be very easily palpable and so it is necessary to concentrate fully on the task and to try and visualize the normal anatomical structures and what might be palpable beneath the examining hand. It may be necessary to repeat the palpation more slowly and deeply. Putting the left hand on top of the right allows increased pressure to be exerted (Fig. 12.11), such as with an obese or very muscular patient.
 Start in the left lower quadrant of the abdomen, palpating lightly, and repeat for each quadrant.
Start in the left lower quadrant of the abdomen, palpating lightly, and repeat for each quadrant.
 Repeat using slightly deeper palpation examining each of the nine areas of the abdomen.
Repeat using slightly deeper palpation examining each of the nine areas of the abdomen.
 Feel for the aorta and para-aortic glands and common femoral vessels.
Feel for the aorta and para-aortic glands and common femoral vessels.
 If a swelling is palpable, spend time eliciting its features.
If a swelling is palpable, spend time eliciting its features.
Left kidney
The right hand is placed anteriorly in the left lumbar region while the left hand is placed posteriorly in the left loin (Fig. 12.12). Ask the patient to take a deep breath in, press the left hand forward and the right hand backward, upward and inward. The left kidney is not usually palpable unless either low in position or enlarged. Its lower pole, when palpable, is felt as a rounded firm swelling between both right and left hands (i.e. bimanually palpable) and it can be pushed from one hand to the other, in an action which is called ‘ballotting’.
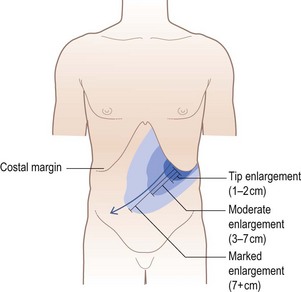
Spleen
Like the left kidney, the spleen is not normally palpable. It has to be enlarged to two or three times its usual size before it becomes palpable, and then is felt beneath the left subcostal margin. Enlargement takes place in a superior and posterior direction before it becomes palpable subcostally. Once the spleen has become palpable, the direction of further enlargement is downwards and towards the right iliac fossa (Fig. 12.13). Place the flat of the left hand over the lower-most rib cage posterolaterally, thus restricting the expansion of the left lower ribs on inspiration and concentrating more of the inspiratory movement into moving the spleeen downwards. The right hand is placed beneath the costal margin well out to the left. Press in deeply with the fingers of the right hand beneath the costal margin, at the same time exerting considerable pressure medially and downwards with the left hand (Fig. 12.14), and then ask the patient to breathe in deeply. Repeat this manoeuvre with the right hand being moved more medially beneath the costal margin on each occasion (Fig. 12.15). If enlargement of the spleen is suspected from the history and it is still not palpable, turn the patient half on to the right side, ask him to relax back onto your left hand, which is now supporting the lower ribs, and repeat the examination as above. Alternatively the spleen may be very large and the lower edge may be much lower than at first suspected. It may help to ask the patient to place the left hand on your right shoulder while palpating for the spleen.