Large polyps may show internal color flow vascularity

 . An elective laparoscopic cholecystectomy for presumed biliary colic revealed cholesterolosis and cholesterol polyps.
. An elective laparoscopic cholecystectomy for presumed biliary colic revealed cholesterolosis and cholesterol polyps.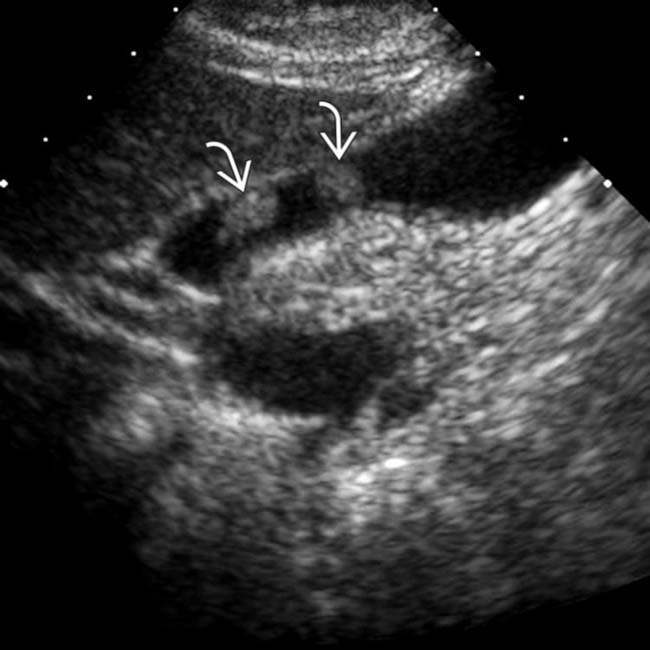
 in the GB that measure < 1 cm in size. While the data suggests nodules < 1 cm harbor a very low risk of malignancy, most society guidelines suggest imaging follow-up.
in the GB that measure < 1 cm in size. While the data suggests nodules < 1 cm harbor a very low risk of malignancy, most society guidelines suggest imaging follow-up.
 . Their small size, echogenicity, multiplicity, and stability at follow-up sonography indicate hyperplastic (cholesterol) polyps.
. Their small size, echogenicity, multiplicity, and stability at follow-up sonography indicate hyperplastic (cholesterol) polyps.
 . The likelihood of neoplasia increases with polyp size, but most GB polyps are hyperplastic.
. The likelihood of neoplasia increases with polyp size, but most GB polyps are hyperplastic.IMAGING
General Features
Ultrasonographic Findings
CLINICAL ISSUES
Presentation
Natural History & Prognosis
• Natural history and management of polyps has been an area of great debate, with no management consensus
• Large prospective study of incidental polyps < 10 mm showed no change in size in 2- and 5-year follow-ups
• Retrospective study of 346 incidental polyps demonstrated growth in only 1% of cases; no lesions < 6 mm were neoplastic
Treatment
• Current recommendations
 Cholecystectomy if patient is symptomatic or if there is coexisting gallstone or PSC (regardless of size of polyp)
Cholecystectomy if patient is symptomatic or if there is coexisting gallstone or PSC (regardless of size of polyp)
 Polyp > 18-20 mm: CT, PET, &/or EUS for preoperative staging → open cholecystectomy with possible resection of adjacent liver tissue
Polyp > 18-20 mm: CT, PET, &/or EUS for preoperative staging → open cholecystectomy with possible resection of adjacent liver tissue
 Cholecystectomy if patient is symptomatic or if there is coexisting gallstone or PSC (regardless of size of polyp)
Cholecystectomy if patient is symptomatic or if there is coexisting gallstone or PSC (regardless of size of polyp) Polyp > 18-20 mm: CT, PET, &/or EUS for preoperative staging → open cholecystectomy with possible resection of adjacent liver tissue
Polyp > 18-20 mm: CT, PET, &/or EUS for preoperative staging → open cholecystectomy with possible resection of adjacent liver tissue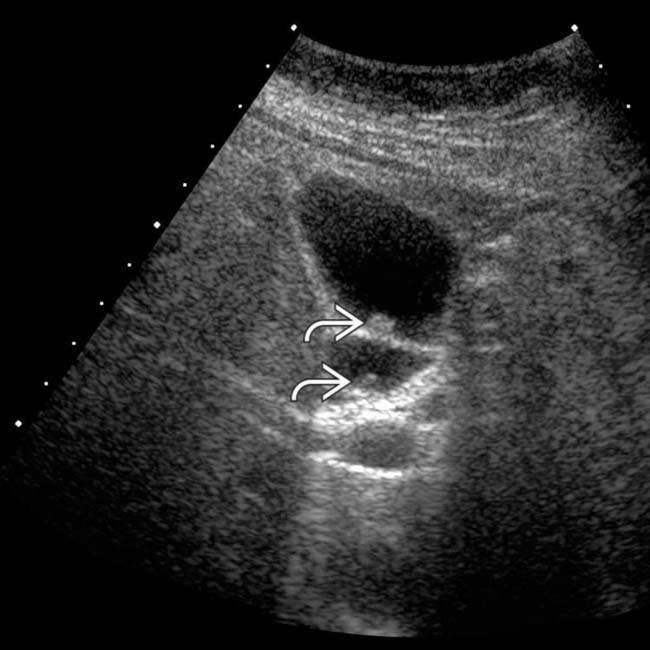
 . Assessment of mobility during real-time examination helps to differentiate between polyps and small, nonshadowing stones or sludge.
. Assessment of mobility during real-time examination helps to differentiate between polyps and small, nonshadowing stones or sludge.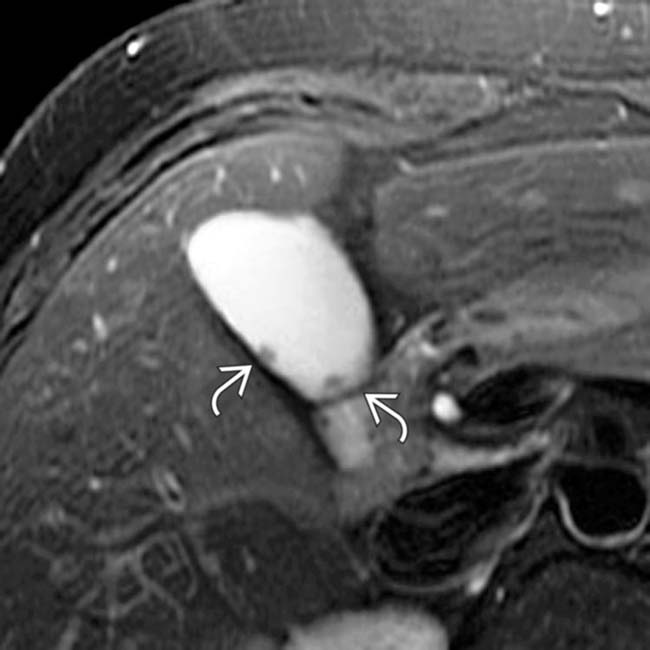
 . These incidental polyps were stable 2 years later. Although tiny polyps are rarely malignant, ultrasound surveillance is typically advocated. How long and at what interval these small polyps should be followed is controversial.
. These incidental polyps were stable 2 years later. Although tiny polyps are rarely malignant, ultrasound surveillance is typically advocated. How long and at what interval these small polyps should be followed is controversial.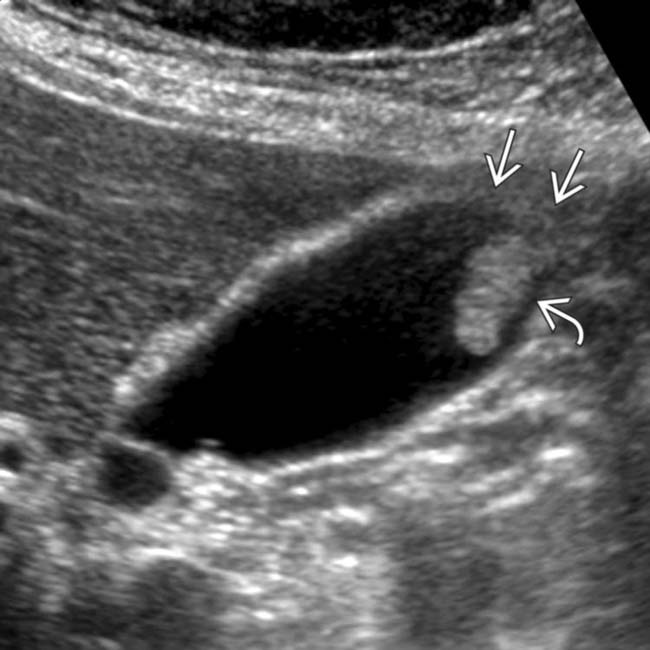
 within the GB fundus. Loss of reflectivity of the adjacent GB wall
within the GB fundus. Loss of reflectivity of the adjacent GB wall  might suggest a neoplastic polyp. This and the size of the polyp prompted elective cholecystectomy, which revealed a solitary but large cholesterol polyp.
might suggest a neoplastic polyp. This and the size of the polyp prompted elective cholecystectomy, which revealed a solitary but large cholesterol polyp.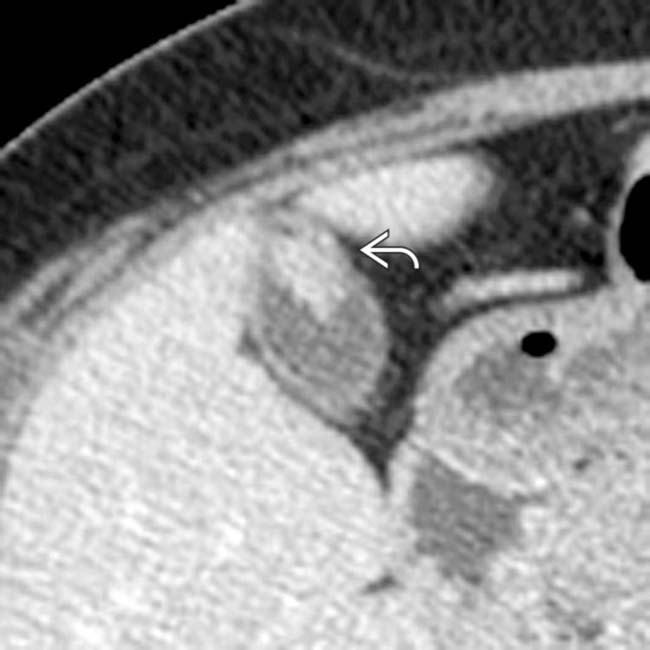
 within the GB fundus. The lack of transmural invasion at CT prompted a laparoscopic, rather than open, cholecystectomy.
within the GB fundus. The lack of transmural invasion at CT prompted a laparoscopic, rather than open, cholecystectomy.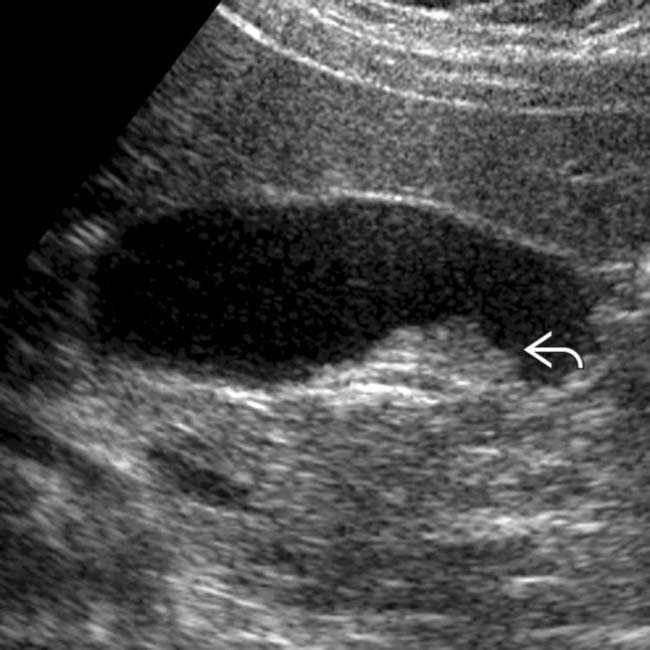
 . Laparoscopic cholecystectomy was performed because of the patient’s symptoms and the size/configuration of the polyp.
. Laparoscopic cholecystectomy was performed because of the patient’s symptoms and the size/configuration of the polyp.
 and no obvious transmural disease. An invasive GB adenocarcinoma was identified at pathology. Early stage, incidental GB carcinoma often appears as a sessile polyp at imaging.
and no obvious transmural disease. An invasive GB adenocarcinoma was identified at pathology. Early stage, incidental GB carcinoma often appears as a sessile polyp at imaging.





























































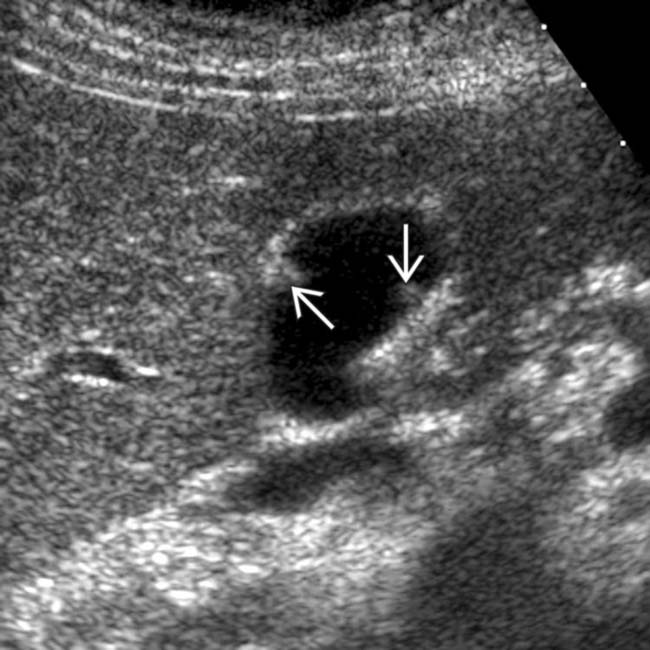
 on both the anterior and posterior walls of the GB, most consistent with cholesterol polyps.
on both the anterior and posterior walls of the GB, most consistent with cholesterol polyps.


