Content usually sterile without GB inflammation
• GB empyema: Pus-filled, inflamed, and distended GB secondary to acute cholecystitis with suppurative intraluminal infection
 , findings consistent with gallbladder hydrops.
, findings consistent with gallbladder hydrops.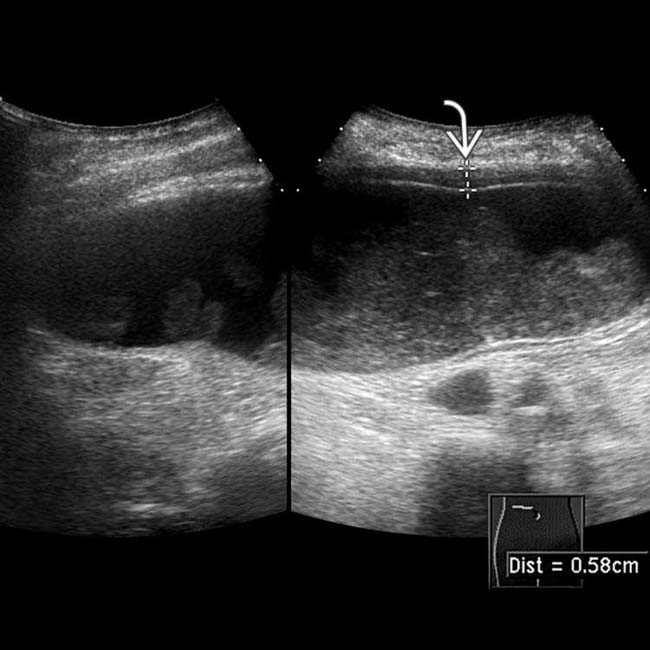
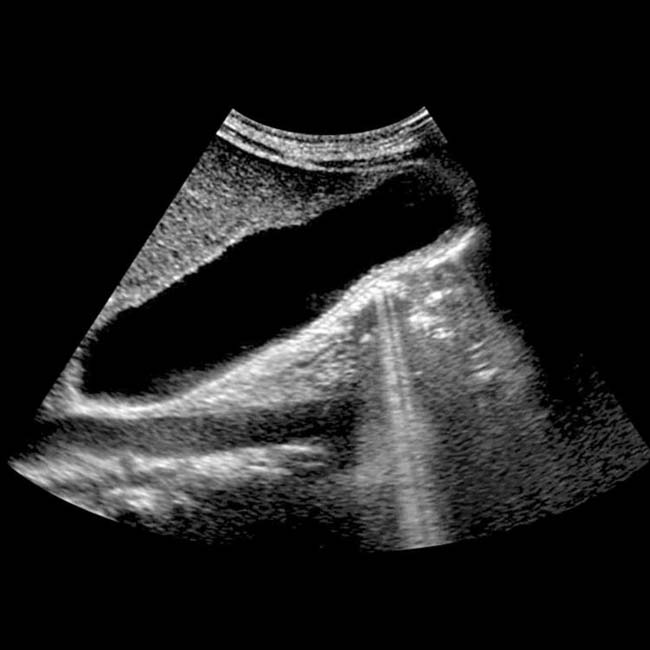
 and rounded but mobile internal echogenic sludge.
and rounded but mobile internal echogenic sludge.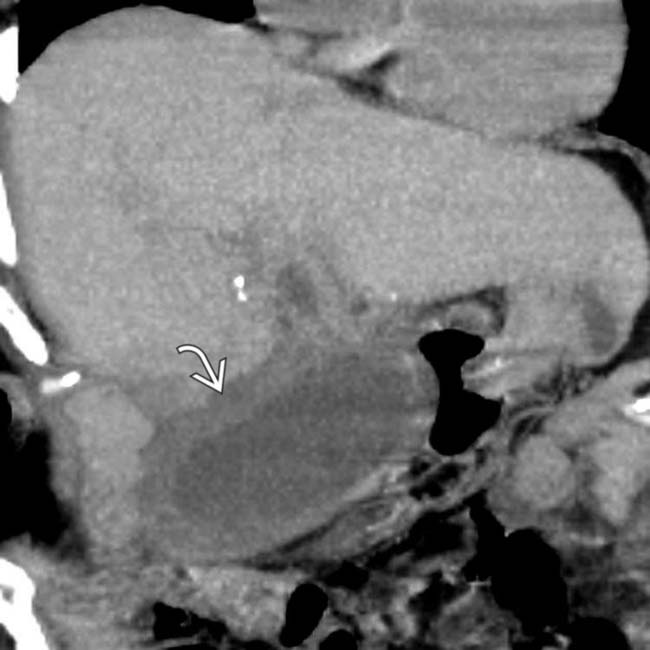
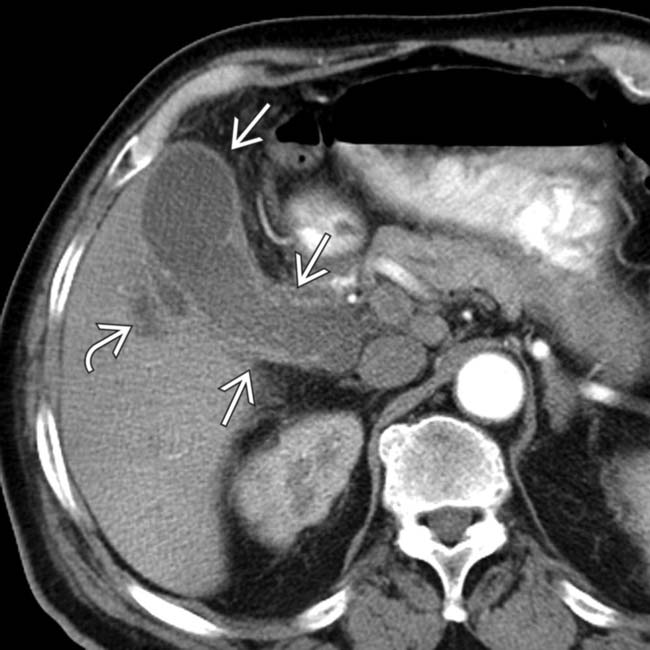
 . Because the patient was considered a poor surgical candidate, she was treated with percutaneous cholecystostomy, which yielded thick bile with a heavy growth of bacteria, consistent with empyema of the gallbladder.
. Because the patient was considered a poor surgical candidate, she was treated with percutaneous cholecystostomy, which yielded thick bile with a heavy growth of bacteria, consistent with empyema of the gallbladder.DIFFERENTIAL DIAGNOSIS
Gangrenous Cholecystitis
• GB wall necrosis and gangrene occurs in 1/4 of patients with acute cholecystitis (usually elderly, diabetic, or immunocompromised patients)
 .
.
 . Lack of contrast within the GB in the hepatobiliary phase suggests that this chronic asymptomatic hydrops is due to a cystic duct obstruction.
. Lack of contrast within the GB in the hepatobiliary phase suggests that this chronic asymptomatic hydrops is due to a cystic duct obstruction.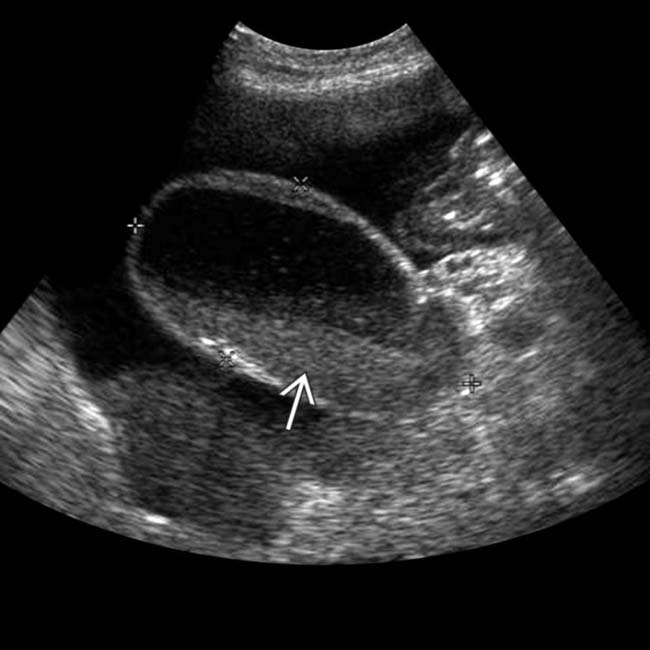
 . The patient had a positive Murphy sign and underwent cholecystectomy, which demonstrated cholecystitis and empyema.
. The patient had a positive Murphy sign and underwent cholecystectomy, which demonstrated cholecystitis and empyema.
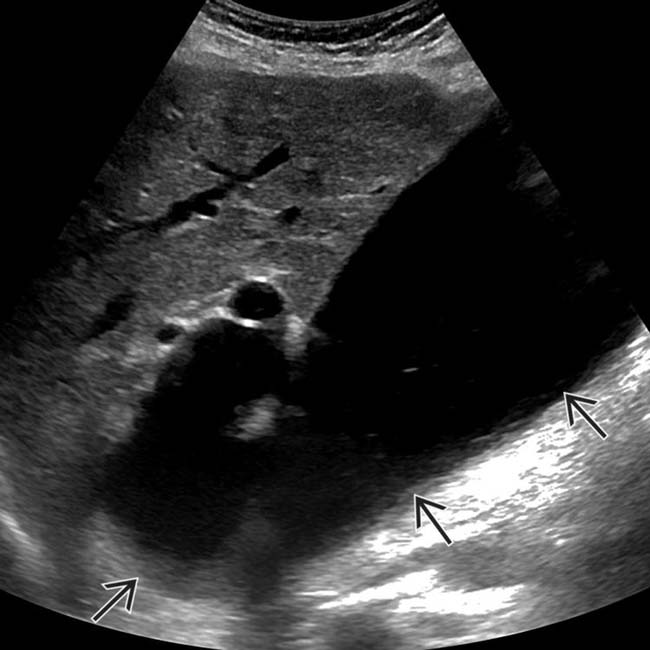
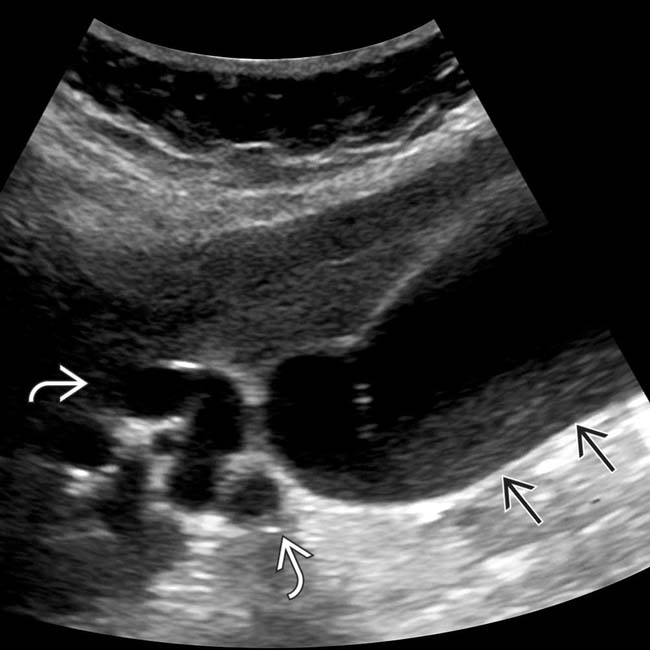
 . Sonographic Murphy sign was positive, compatible with GB empyema.
. Sonographic Murphy sign was positive, compatible with GB empyema.
 . The poor definition of the GB wall
. The poor definition of the GB wall  was suspicious for gangrene, confirmed at surgery.
was suspicious for gangrene, confirmed at surgery.
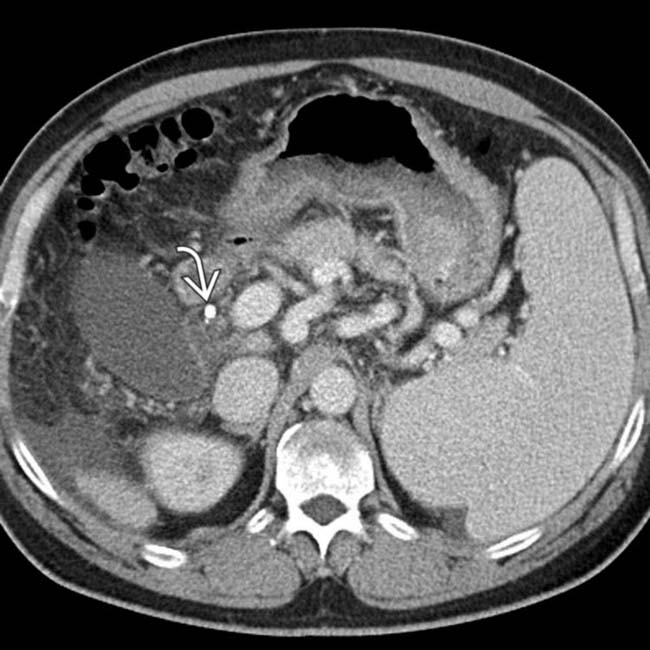
 , and a large gallstone
, and a large gallstone  , compatible with GB empyema and associated contained perforation.
, compatible with GB empyema and associated contained perforation.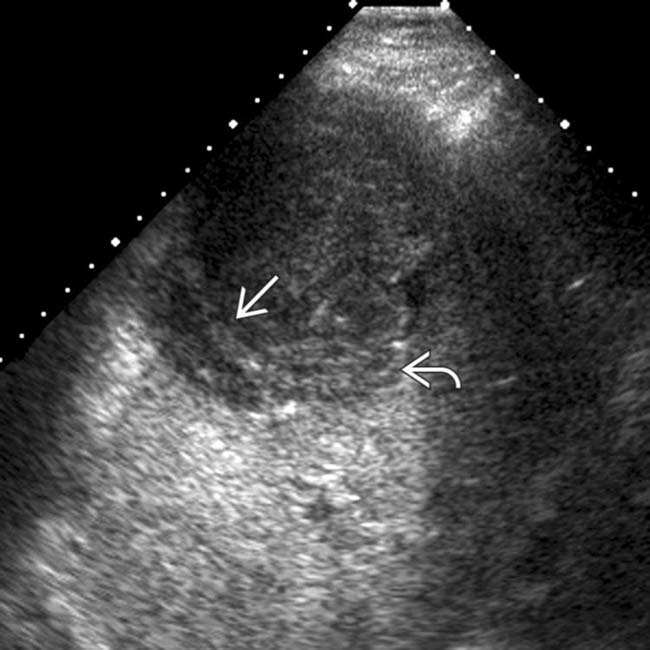
 within the gallbladder due to gangrenous cholecystitis, as well as echogenic pus
within the gallbladder due to gangrenous cholecystitis, as well as echogenic pus  within the gallbladder due to gallbladder empyema.
within the gallbladder due to gallbladder empyema.

 and a poorly defined pericholecystic fluid collection along adjacent liver
and a poorly defined pericholecystic fluid collection along adjacent liver  .
.
 and a pericholecystic fluid collection
and a pericholecystic fluid collection  . A perforated, pus-filled GB and an adjacent abscess were identified at laparotomy and cholecystectomy.
. A perforated, pus-filled GB and an adjacent abscess were identified at laparotomy and cholecystectomy.





































































 , and cystic duct dilatation
, and cystic duct dilatation  . GB distension was the most obvious manifestation of duct obstruction at ultrasound and prompted additional imaging.
. GB distension was the most obvious manifestation of duct obstruction at ultrasound and prompted additional imaging.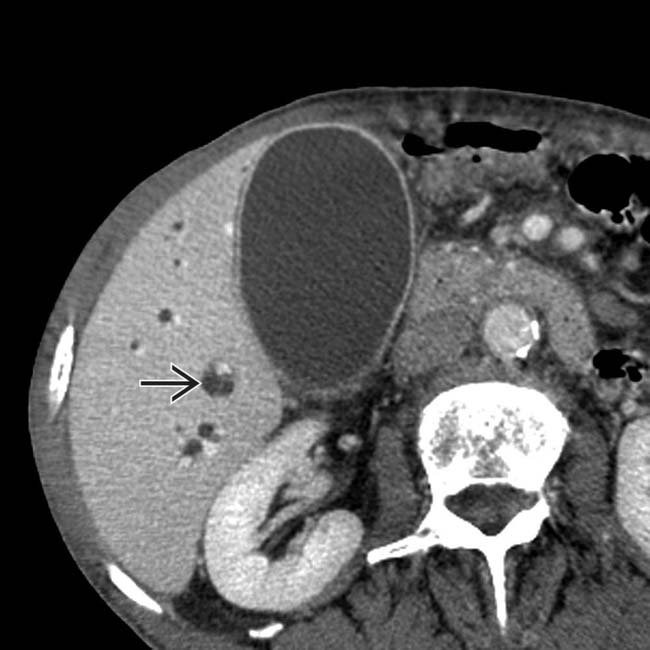
 . GB distension was due to obstruction of the distal common bile duct by a pancreatic head carcinoma (not shown).
. GB distension was due to obstruction of the distal common bile duct by a pancreatic head carcinoma (not shown).


