Fungi
1. Fungi are eukaryotic organisms.
2. Fungal membranes contain ergosterol rather than cholesterol found in other eukaryotic membranes.
3. The cell wall surrounding fungal cells, which differs in composition from bacterial cell walls, contains chitin, glucans, and protein.
1. Molds, or filamentous fungi, are composed of a mass of branching, thread-like tubular filaments (hyphae) that elongate at their tips.
• Septate hyphae are divided into individual walled-off cells, each containing a nucleus.
• Aseptate (coenocytic) hyphae are hollow and multinucleate.
2. Yeasts are unicellular, usually round fungi.
3. Dimorphic fungi exist as molds or yeasts depending on temperature or other environmental factors.
4. Dematiaceous fungi are dark colored and usually from soil.
1. All fungi can reproduce asexually, and asexually reproducing forms are most commonly encountered in clinical situations.
D Conditions conducive to fungal infections
• Although fungi are ubiquitous in the environment, they generally colonize tissues and cause infection only when the body’s normal defenses or the normal flora are disrupted.
1. Disruption of the body’s physical, chemical, or physiologic barriers
• Intact skin, pH, fatty acids in the skin, normal bacterial flora, and various humoral factors normally prevent fungal infection.
2. Immunosuppression, particularly loss of CD4 TH1 responses
E Types of fungal infections (mycoses)
• Fungal infections and the agents causing them are commonly classified based on the site of disease or the immune status of the host.
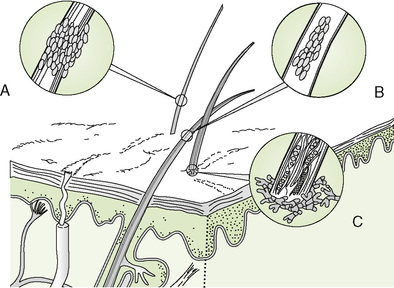
1. Superficial mycoses involve the keratinized outermost layers of skin, hair, and nails.
2. Cutaneous mycoses involve the keratin-containing epidermis and deeper layers of the hair, skin, and nails.
3. Subcutaneous mycoses involve the dermis, subcutaneous tissues, muscles, and fascia.
4. Systemic mycoses often originate in the lungs but disseminate to other organs (especially in immunocompromised individuals).
5. Opportunistic mycoses generally occur only in patients with compromised immune systems (e.g., cancer patients receiving immunosuppressive therapy and human immunodeficiency virus [HIV]-infected individuals).
F Diagnosis of fungal infections
• Fungal infections mimic other diseases and therefore must be distinguished through careful differential diagnosis (Table 28-1).
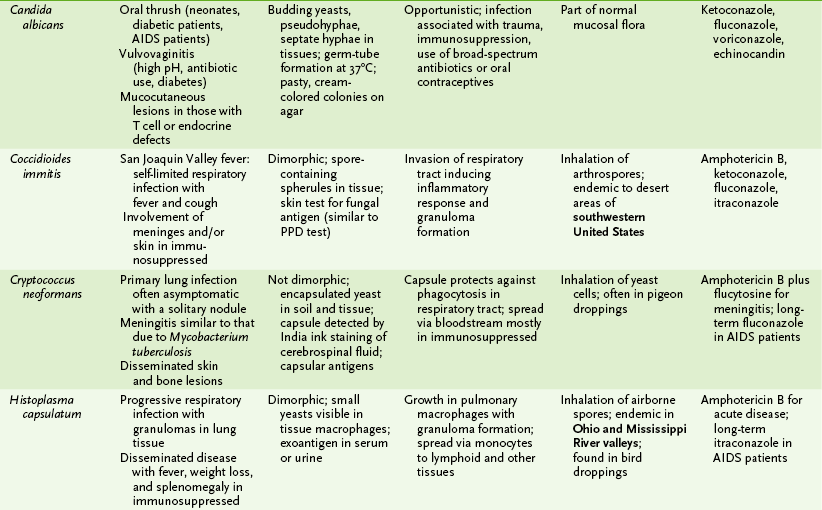
TABLE 28-1
Differential Diagnosis of Fungal Infections
| Infection | Etiologic agent | Other conditions to exclude |
| Aspergillosis | Aspergillus species | Zygomycoses and other mold infections |
| Blastomycosis | Blastomyces dermatitidis | Bacterial and viral pneumonia, atypical mycobacterial infection, other systemic mycoses, bacterial or mycobacterial skin infections |
| Candidiasis | Candida albicans | Bacterial and other fungal infections |
| Chromoblastomycosis | Dematiaceous soil fungi | Sporotrichosis, tularemia, plague, gangrene, actinomycosis, atypical mycobacterial infection |
| Coccidioidomycosis | Coccidioides immitis | Bacterial and viral pneumonia; skin infections caused by bacteria, viruses, or other fungi |
| Cryptococcosis | Cryptococcus neoformans | Meningitis caused by bacteria (e.g., Mycobacterium tuberculosis) and viruses, lung cancer, other systemic mycoses (especially histoplasmosis) |
| Histoplasmosis | Histoplasma capsulatum | Other systemic mycoses, bacterial and viral pneumonia, tuberculosis |
| Mycetoma, eumycotic | Dematiaceous soil | Mycetoma caused by soil bacteria fungi |
| Paracoccidioidomycosis | Paracoccidioides brasiliensis | Bacterial and viral pneumonia; skin infections caused by bacteria, viruses, or other fungi |
| Ringworm (tinea) | Trichophyton, Microsporum, and Epidermophyton species | Candidal infections; bacterial and viral skin infections |
| Sporotrichosis | Sporothrix schenckii | Tularemia, plague, gangrene, nocardiosis, chronic staphylococcal skin infections, atypical mycobacterial infection, other mycoses |
| Zygomycosis | Rhizopus and Mucor species | Aspergillosis and other mold infections |
1. Culture and microscopic examination
• Isolation of fungi from specimens may require culturing for up to 30 days at 25°C and 35°C on appropriate media.
a. Sabouraud agar, Mycosel agar
b. Antibacterial antibiotics are often included in the medium to inhibit bacterial overgrowth.
• Specific histologic stains can be used for direct visualization of fungi in tissue specimens.
• Sugar utilization tests (similar to the fermentation tests for Enterobacteriaceae) are useful in identifying yeasts.
2. Detection of fungal antigens in blood or cerebrospinal fluid (CSF) by Ouchterlony (double-immunodiffusion) test or enzyme-linked immunosorbent assay
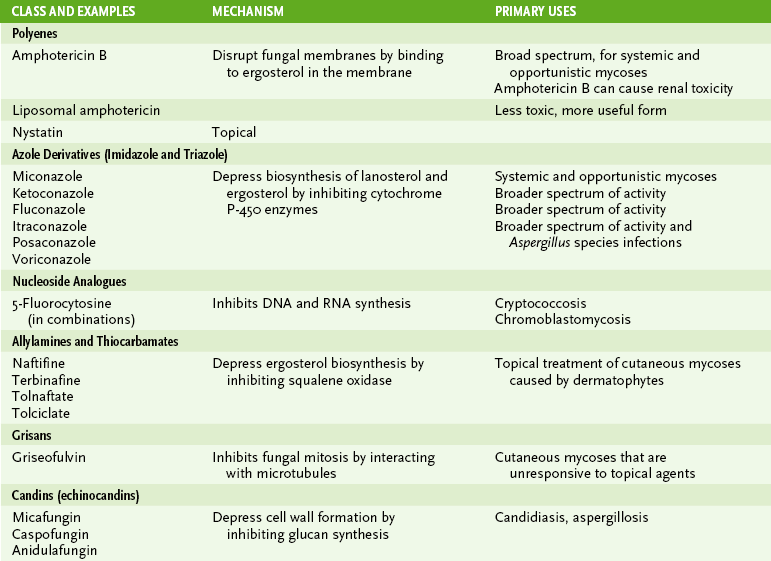
• Table 28-2 lists common drugs used in treating mycoses and their mode of action.
II Superficial and Cutaneous Mycoses
1. Caused by various Trichophyton, Microsporum, and Epidermophyton species, collectively referred to as dermatophytes.
2. These infections are generally restricted to keratin-containing tissues and may elicit cellular immune responses, leading to inflamed, outward-spreading lesions. They may also contribute to seborrhea and dandruff.
• Ringworm, the common name for these infections, describes the lesions, which are in the form of a ring and resemble a worm burrowing in the skin.
• Tinea plus modifier specifically indicates the site involved. For example:
III Subcutaneous, Opportunistic, and Systemic Mycoses
• Pertinent information about common mycoses and the fungi causing them are summarized in Table 28-3.
TABLE 28-3
Summary of Common Fungal Pathogens
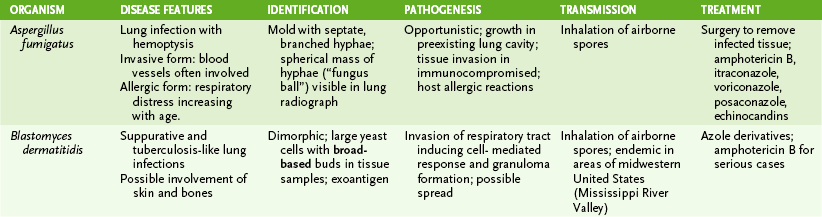
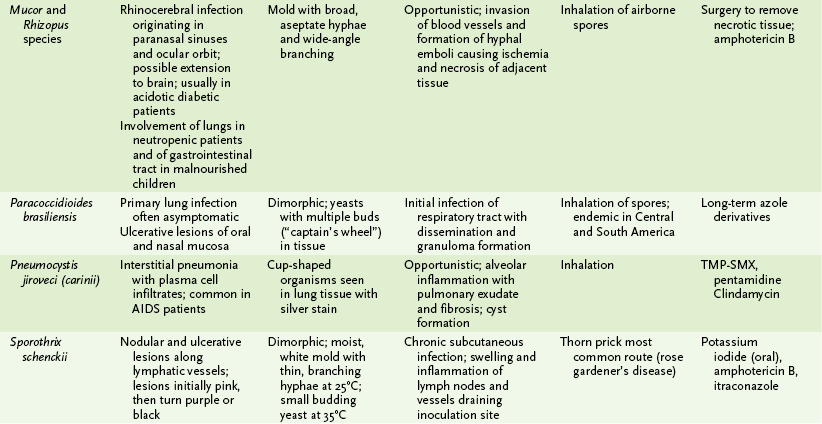
PPD, purified protein derivative; TMP-SMX, trimethoprim-sulfamethoxazole.
• These infections are often caused by melanin-containing (dematiaceous) fungi present in the soil or decaying vegetation.
• Organisms usually enter through cuts, punctures, or stabs caused by contaminated thorns or sharp tools.
• Caused by Sporothrix schenckii, a dimorphic fungus
• Chronic nodular and ulcerative nodular lymphocutaneous lesions along lymphatics (e.g., rose gardener’s disease)
• Caused by various dematiaceous soil fungi
• Verrucoid (warty) nodules with cauliflower-like appearance; pseudoepitheliomatous hyperplasia
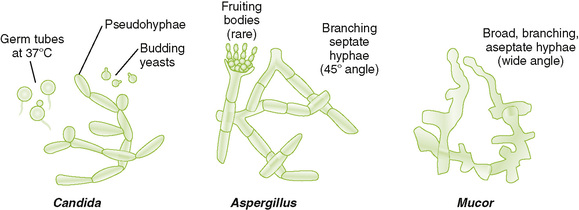
B Agents of opportunistic mycoses (Fig. 28-2)
• Major characteristics distinguishing fungi that cause opportunistic and systemic mycoses are outlined in Box 28-1.
a. Oral thrush is most common in neonates, diabetics, AIDS patients, and those receiving antibiotics or steroids.
b. Vulvovaginitis is promoted by antibiotic use, higher pH, and diabetes mellitus.
• Chronic mucocutaneous candidiasis (rarely disseminates but is resistant to treatment)
3. Aspergillus fumigatus and other Aspergillus species
• Filamentous with septate, branched hyphae; “fungus ball” in lungs seen on radiograph; induces allergic reactions
• Pulmonary infection established in preexisting cavitary lesion (fungus ball)
• Becomes invasive in immunocompromised patients, especially neutropenic patients
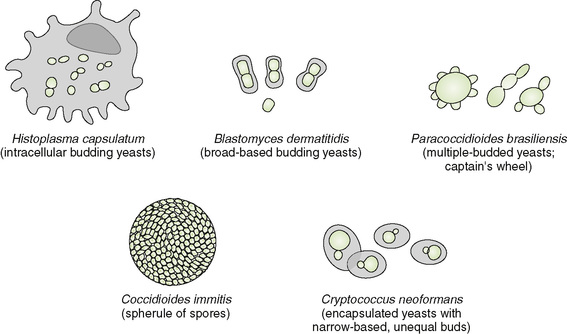
C Agents of systemic mycoses (Fig. 28-3)
• Most agents of systemic mycoses are dimorphic, existing as filamentous fungi in soil (saprobic phase) and as yeasts or spherules in tissue at 37°C (parasitic phase)
• In healthy individuals, many systemic mycoses are asymptomatic or manifest as a relatively mild, self-limited pulmonary infection.
• In immunocompromised individuals, systemic mycoses generally exhibit more serious lung involvement and often disseminate to other organs.
• Blastomycosis is marked by tuberculosis-like pneumonia with possible skin, bone, or prostate involvement.
• Primary cryptococcosis is often discovered accidentally as a solitary pulmonary nodule that may mimic carcinoma.
• Granulomatous meningitis is the most common form of systemic disease.