98 Fungal Infections
Candida Albicans
Clinical Manifestations and Management
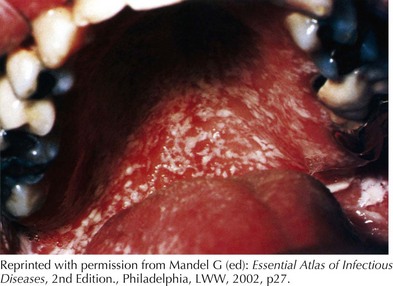
Oral candidiasis, also known as oral thrush, is a candidal infection of the oral-pharyngeal mucosa (Figure 98-1). It can affect up to 2% to 5% of otherwise healthy newborn infants and present as early as 7 to 10 days of life. In immunocompetent children, it is most common in infants and presents as adherent white plaques on the buccal or gingival mucosa. Removal of these plaques can result in localized bleeding. It can present with no symptoms or with increased fussiness and decreased feeding. Oral thrush is uncommon in children older than 12 months except after antibiotic use. Without recent antibiotic use, one may consider a primary immunodeficiency, diabetes mellitus, or HIV infection. Pseudomembranous candidiasis can be diagnosed clinically or by the identification of yeast cells and pseudohyphae by Gram stain or potassium hydroxide prep. Thrush can be treated with nystatin applied directly to the oral mucosa for 7 to 10 days. Thrush caused by antibiotic use generally resolves as the offending agent is discontinued. Bottle nipples and pacifiers should be sterilized as well to prevent reinfection.
Aspergillus Fumigatus
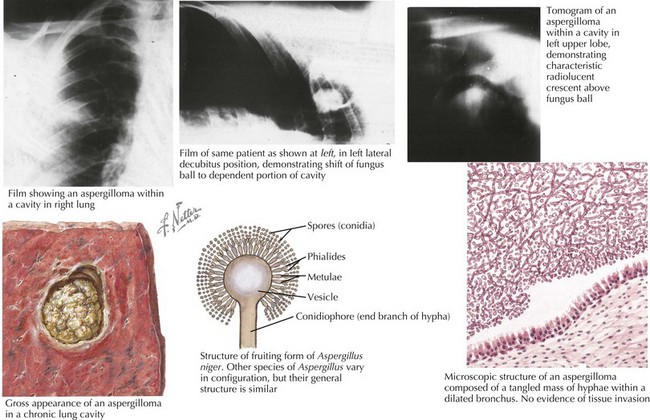
Aspergillus is a mycelial fungus, ubiquitous in the environment found in the soil and on decaying plants. A. fumigatus is the most common species isolated clinically, followed by Aspergillus flavus. Exposure occurs commonly by inhalation of conidia (spores); however inhalation of contaminated aerosols and direct inoculation of skin also occur. Some estimate that most people inhale hundreds of A. fumigatus conidia per day. Once inhaled Aspergillus can colonize the upper and lower respiratory tract. In an immune competent host, macrophages and neutrophils prevent the development of invasive disease. Immunocompromised children are at risk for invasive respiratory disease and for hematogenous dissemination. Invasive aspergillosis in an otherwise healthy child with no known risk factors should prompt an evaluation for chronic granulomatous disease. Aspergillus-related diseases may be hypersensitivity (IgE) mediated, saprophytic (noninvasive), or invasive (Figure 98-2).
Cryptococcus Neoformans
Clinical Presentation and Management
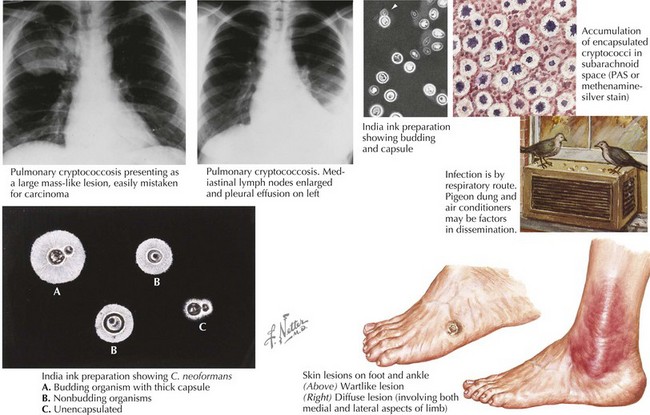
Pneumonia is the most common form of cryptococcosus and may be asymptomatic in up to one third of immune competent hosts. Symptoms may include fever, pleuritic chest pain, and constitutional symptoms. Chest radiograph may show diffuse interstitial infiltrates and hilar lymphadenopathy (Figure 98-3). Dissemination following pulmonary disease is uncommon except where there is a deficiency in cell mediated immunity—HIV, leukemia, SLE, congenital immunodeficiency, chronic cutaneous candidiasis. HIV infection is the most common immune compromised state for Cryptococcal infection. In addition, Cryptococcus is an AIDS defining infection in HIV patients.
Subacute or chronic meningitis is the most common manifestation of disseminated Cryptococcus and may present only as behavioral change or may present with fever and headache (see Figure 98-3). Signs of increased intracranial pressure are also common and may be life threatening. Focal neurologic signs are present in less than 10%. Classically diagnosis was made by staining CSH with India Ink where encapsulated yeast may be visualized. More recently diagnosis is enhanced by latex agglutination testing for cryptococcal antigen. Treatment of Cryptococcus depends on the status of the host and on the site of infection. Asymptomatic, immune competent hosts may be watched closely or treated with fluconazole daily for 3-12 months. Those with symptomatic or disseminated disease are treated initially with amphotericin B and fluconazole for 2-10 weeks depending on clinical response, then with single therapy with fluconazole for 6-12 months. Children with HIV who complete initial therapy for Cryptococcus should remain on lifelong suppressive therapy with fluconazole.
Common Tinea Infections
Tinea Corporis (Ringworm)
Tinea corporis is a dermatophyte infection of the glabrous (smooth and hairless) skin. The lesion is typically well demarcated, circular, and slightly erythematous, with a scaly, pustular, or vesicular border and is often pruritic (Figure 98-4). The main causative agents include Trichophyton rubrum, Trichophyton mentagrophytes, Trichophyton tonsurans, Microsporum canis, and Epidermophyton floccosum. Treatment of tinea corporis is topical with medication applied to the skin at least 2 cm beyond the border of the lesion once or twice daily (depending on the antifungal) for 2 weeks. Persistence of the lesion after 4 weeks of therapy indicates treatment failure and may require systemic therapy. Common topical antifungal therapy for tinea corporis includes miconazole, clotrimazole, terbinafine, ketoconazole, and econazole.
Other, Less Common Tinea Infections
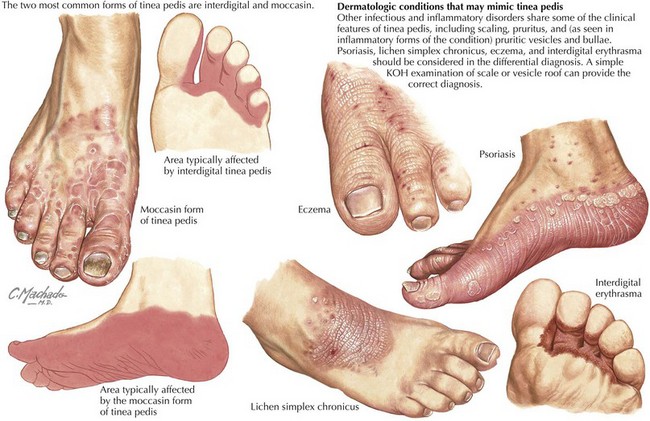
Tinea pedis: Tinea pedis is a superficial infection of the feet, often known as athlete’s foot. It often presents with pruritic vesiculopustular or vesicular lesions with associated fissuring and scaling between the toes (Figure 98-5). Tinea pedis may also present in a moccasin distribution with hyperkeratotic scales involving the soles and lateral feet. Treatment is topical. Toenails may be affected (tinea unguium) and require systemic therapy.
Burgos A, Zaoutis TE, Dvorak CC, et al. Pediatric invasive Aspergillosis: a multicenter retrospective analysis of 139 contemporary cases. Pediatrics. 2008;121(5):e1286-e1293.
Committee on Infectious Diseases American Academy of Pediatrics. Red Book, ed 27. American Academy of Pediatrics; 2006.
Gershon A, Hotez P, Katz S. Krugman’s Infectious Diseases of Children, ed 11. St. Louis: Mosby; 2003.
Jeong YJ, Kim KI, Seo IJ, et al. Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. RadioGraphics. 2007;27:617-630.
Kliegman RM, Behrman RE, Jenson HB, Stanton B. Nelson Textbook of Pediatrics, ed 18. Philadelphia: Saunders; 2007.
Kokotos F, Henry A. Vulvovaginitis. Pediatr Rev. 2006;27:116-117.
Krol D, Keels MA. Oral conditions. Pediatr Rev. 2005;28(1):15-21.
Long S, Pickering L, Prober C. Principles and Practices of Infectious Disease, ed 3. St. Louis: Elsevier; 2008.
Pappas PG, Kauffman CA, Andes D, et al. Infectious Diseases Society of America: Clinical practice guidelines for the treatment of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503-535.
Shy R. Tinea corporis and tinea capitis. Pediatr Rev. 2007;28(5):164-173.