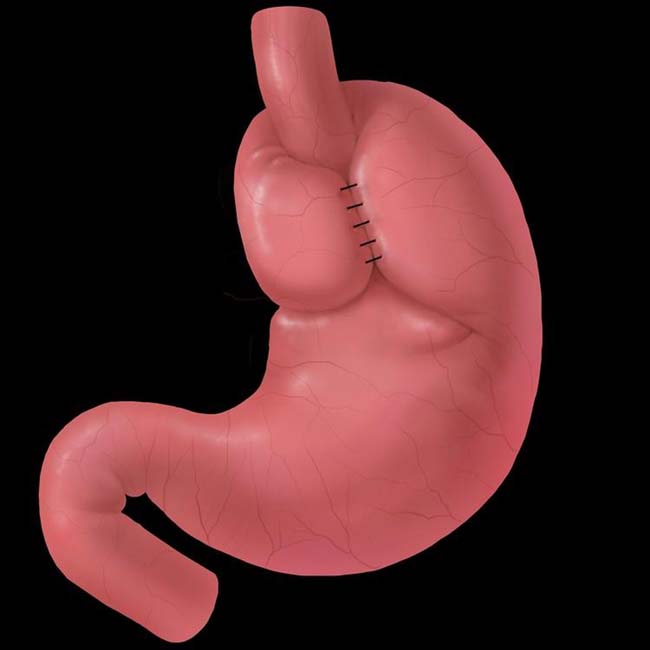
GE junction (at B ring) will be above diaphragm; intact wrap around proximal stomach (neoesophagus) will be below diaphragm
IMAGING
 in its expected subdiaphragmatic location as a filling defect within the air-filled fundus. The distal 3 cm of the esophageal lumen is compressed as it passes through the wrap.
in its expected subdiaphragmatic location as a filling defect within the air-filled fundus. The distal 3 cm of the esophageal lumen is compressed as it passes through the wrap.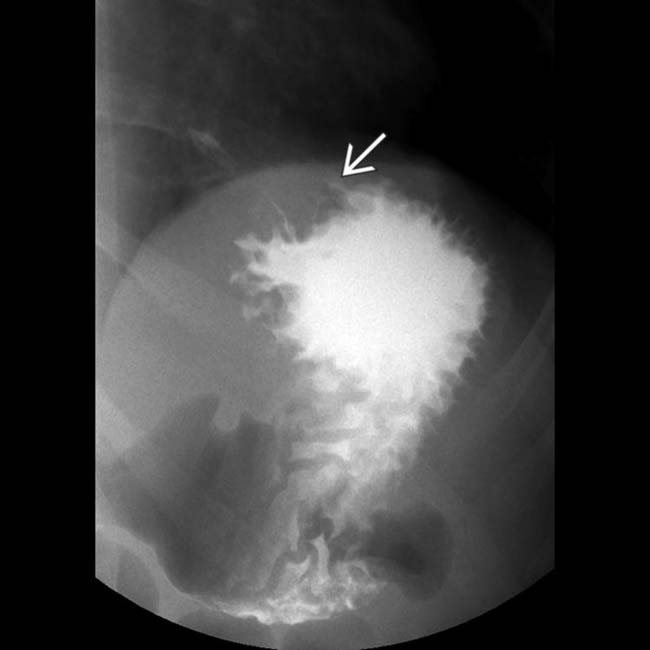
 as a filling defect with the barium pool in the fundus.
as a filling defect with the barium pool in the fundus.
 within the gastric fundus. The metallic staple line is evident within the wrap. The mass effect of the wrap tends to decrease with time following surgery.
within the gastric fundus. The metallic staple line is evident within the wrap. The mass effect of the wrap tends to decrease with time following surgery.IMAGING
Radiographic Findings
• Normal postoperative appearance
CT Findings
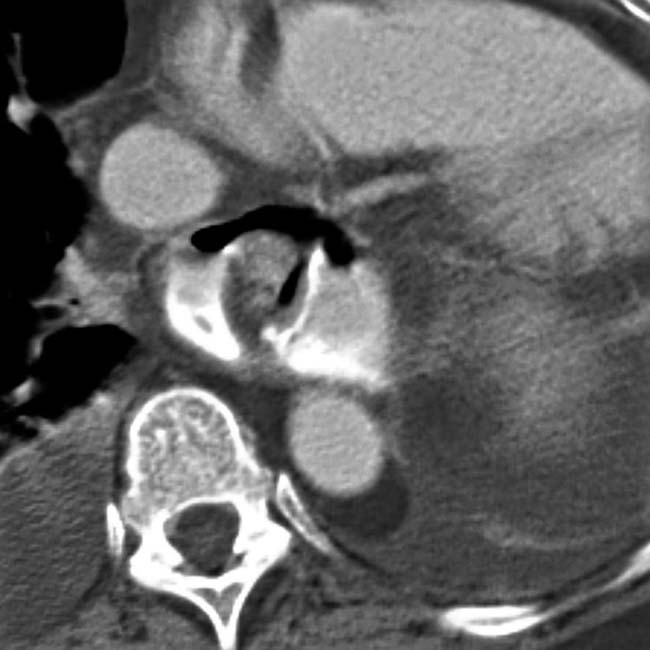
• Herniation of intact FDP through diaphragmatic hiatus; seen as mediastinal mass on coronal reformatted images
CLINICAL ISSUES
Presentation
Natural History & Prognosis
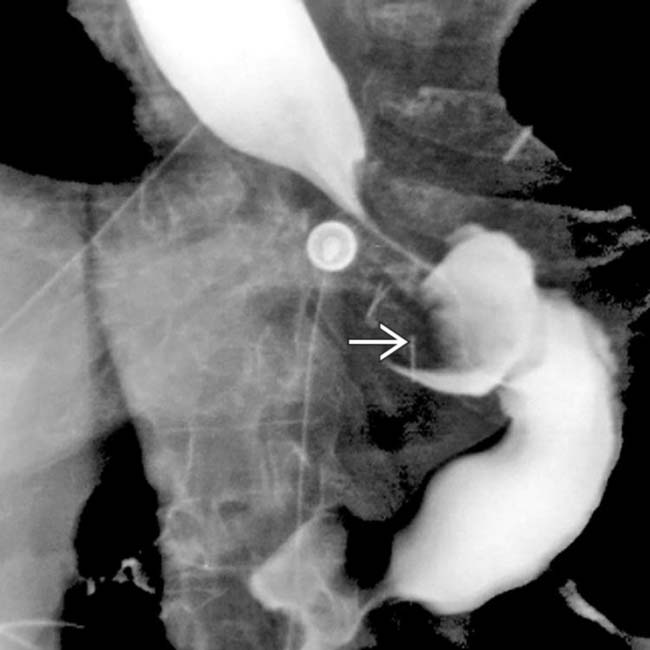
 within the gastric fundus.
within the gastric fundus.
 that constitute the wrap, but the compression of the distal esophagus is maintained.
that constitute the wrap, but the compression of the distal esophagus is maintained.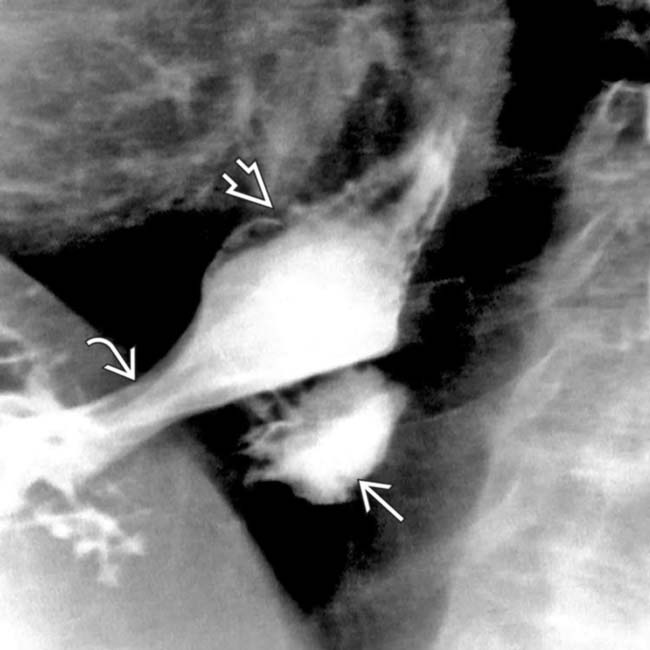
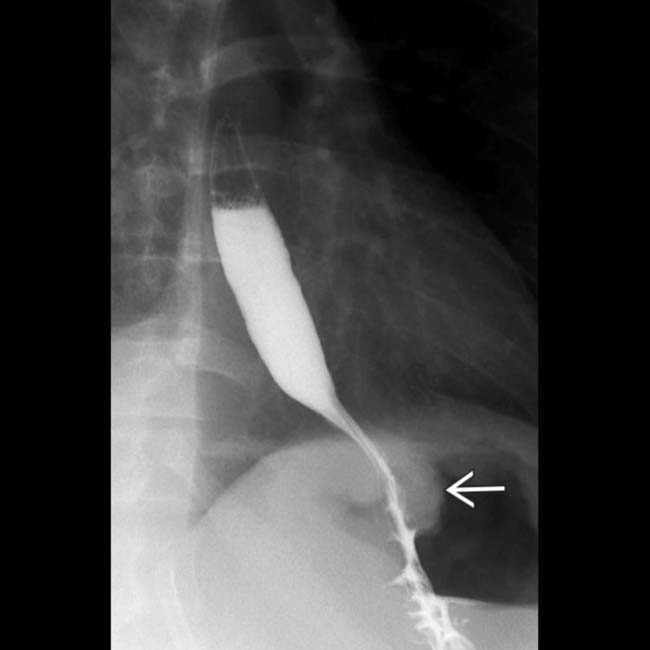
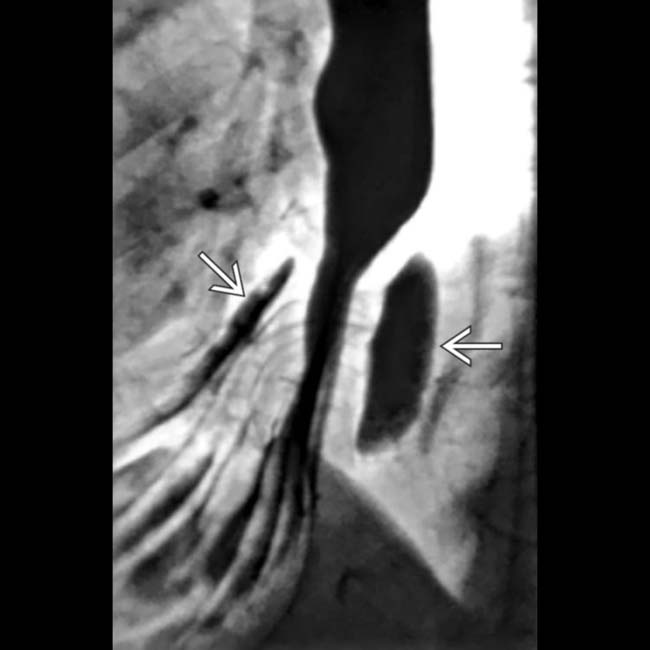
 , which has slipped through the hiatus
, which has slipped through the hiatus  . Suture disruption is implied by the loose compression of the neoesophagus. The B ring
. Suture disruption is implied by the loose compression of the neoesophagus. The B ring  marks the esophagogastric junction.
marks the esophagogastric junction.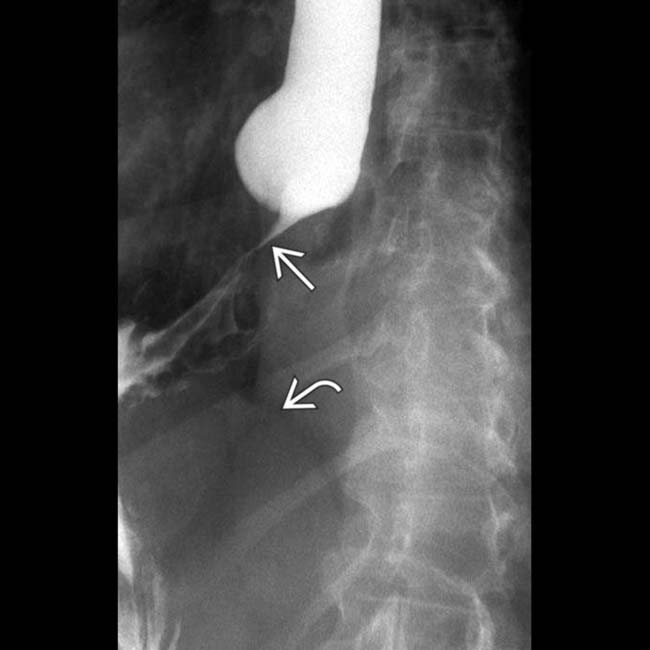
 , but well above the diaphragm
, but well above the diaphragm  .
.
 . This should not be mistaken for a perforation. Note the intact gastric folds within the wrap. The Toupet wrap is often used in older patients with poor esophageal motility, as evident in this patient by slow emptying of the esophagus and tertiary contractions.
. This should not be mistaken for a perforation. Note the intact gastric folds within the wrap. The Toupet wrap is often used in older patients with poor esophageal motility, as evident in this patient by slow emptying of the esophagus and tertiary contractions.
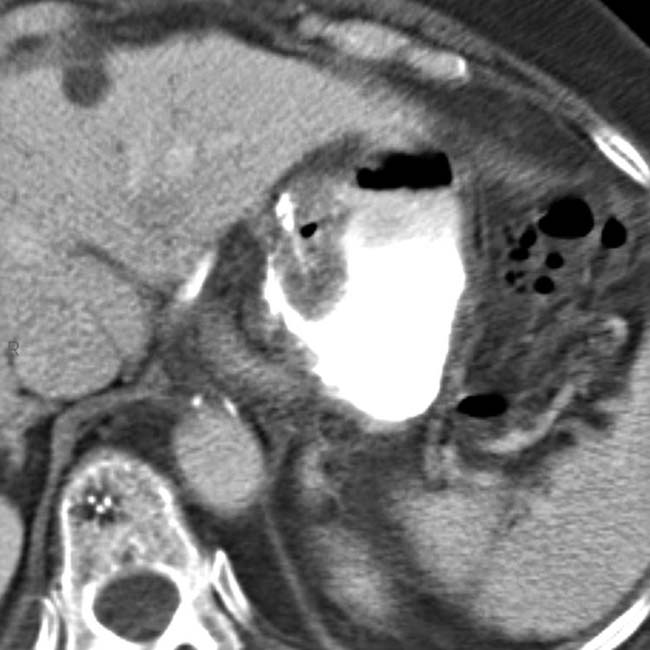
 and gas
and gas  into the mediastinum, indicating perforation of the esophagus or the wrap.
into the mediastinum, indicating perforation of the esophagus or the wrap.
 due to perforation of the Nissen FDP.
due to perforation of the Nissen FDP.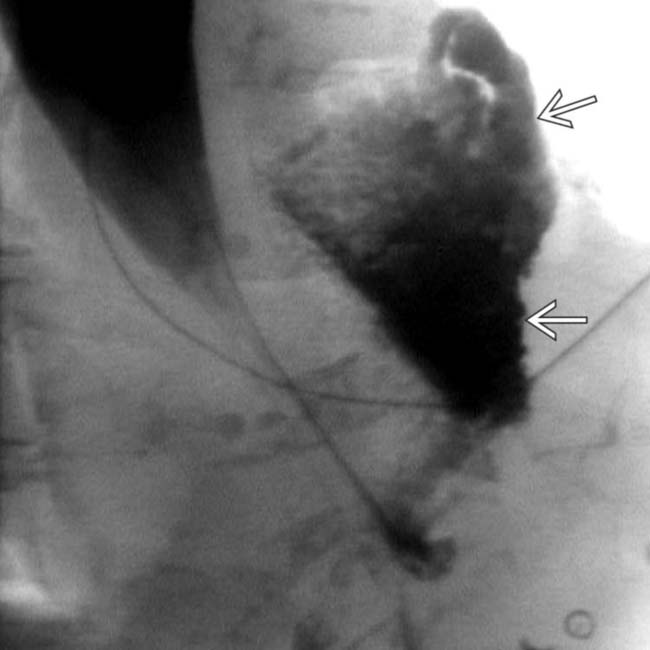
 into the mediastinum, from the distal esophagus. Very little contrast reaches the stomach.
into the mediastinum, from the distal esophagus. Very little contrast reaches the stomach.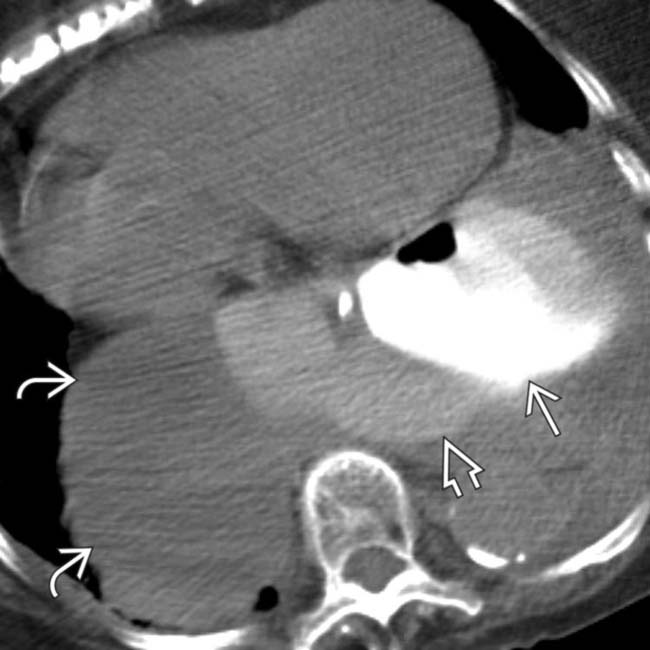
 , and residual herniation of the stomach
, and residual herniation of the stomach  . The dense collection of extraluminal contrast
. The dense collection of extraluminal contrast  indicates a leak from near the operative site.
indicates a leak from near the operative site.
 and left pleural space
and left pleural space  , indicating a leak from the distal esophagus. Very little contrast enters the stomach.
, indicating a leak from the distal esophagus. Very little contrast enters the stomach.
 that drained a loculated left hydropneumothorax (not shown here), left lower lobe pneumonia, and extravasated gas and contrast within the mediastinum
that drained a loculated left hydropneumothorax (not shown here), left lower lobe pneumonia, and extravasated gas and contrast within the mediastinum  .
.
 in the space formerly occupied by the herniated stomach. Hemothorax is also evident
in the space formerly occupied by the herniated stomach. Hemothorax is also evident  .
.
 are present from the mesh repair of the large hernia, and more mediastinal hematoma is seen
are present from the mesh repair of the large hernia, and more mediastinal hematoma is seen  . This hematoma should not be mistaken for leak of contrast medium.
. This hematoma should not be mistaken for leak of contrast medium.
 .
.
 , subsequently confirmed to be due to a leak from the operative site. A small liver laceration
, subsequently confirmed to be due to a leak from the operative site. A small liver laceration  is also seen.
is also seen.

























































































 from the FDP site.
from the FDP site.
 near the site of the FDP.
near the site of the FDP.