Chapter 17 Fractures of the Distal Humerus
Plating Techniques
Introduction
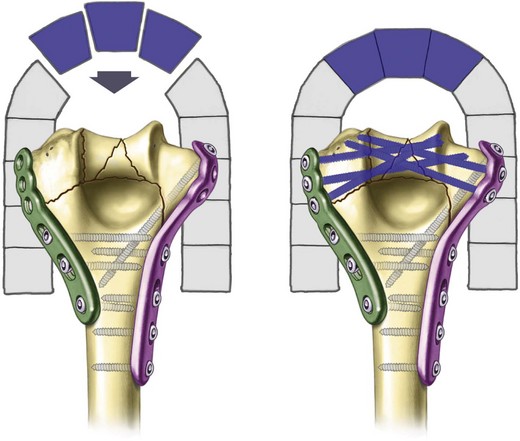
Severe comminution, bone loss and osteopenia predispose distal humerus fractures to unsatisfactory results due to inadequate fixation. Poor outcomes include contracture, secondary to prolonged immobilization thought necessary to protect the fixation, and non-union. In an effort to reproducibly obtain stable fixation in the presence of osteoporosis or comminution, we have developed an improved fixation technique for fractures of the distal humerus based on principles that enhance fixation in the distal fragments and provide compression at the supracondylar level.1–4 The key to the stability achieved with this fixation construct is that it combines the features and stability of an arch while locking the two columns of the distal humerus together.
Background
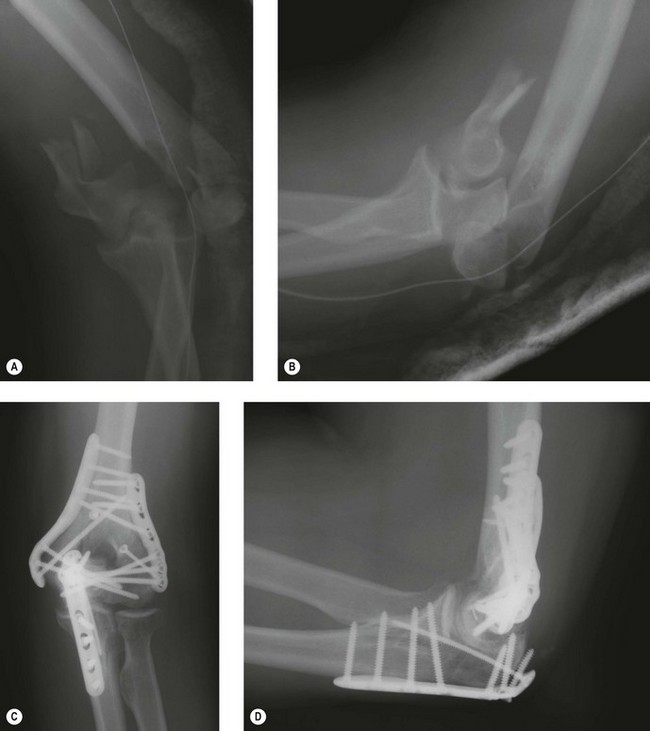
The critical concept being presented here is the idea that stability of the distal humerus is achieved by the creation of an architectural structure. The bone fragments rely for stability on their integration with the structure, rather than on fixation by screw threads. The concept is borrowed from modern architecture and the application of civil engineering principles to surgery. The interdigitation of screws within the distal segment rigidly attaches the articular fragments to the shaft by linking the two columns together. This permits stability to be achieved in such cases as low transcondylar (Fig. 17.1) or severely comminuted (Fig. 17.2) fractures.
Surgical techniques
Exposure
I prefer to perform this operation with the patient in the supine position. If assistance is limited, the lateral decubitus position with the arm over a bolster or arm holder may be easier. A sterile tourniquet is inflated only for dissection of the ulnar nerve, which is transposed anteriorly. An olecranon osteotomy provides the greatest exposure and is recommended in the setting of intra-articular comminution. The TRAP (triceps-reflecting anconeus pedicle) approach provides adequate exposure for a surgeon experienced with the technique.5 This involves combining the Bryan–Morrey and modified Kocher approaches to reflect the triceps in continuity with the anconeus.
Principle-based fixation technique
Stability is optimized by achieving eight technical objectives derived from the principles of (1) maximizing fixation in the distal fragments and (2) ensuring that all fixation in the distal segment contributes to stability at the supracondylar level. Six of these objectives concern the screws in the distal fragments and two concern the plates (Fig. 17.3).
Summary Box 17.1 Technical objective checklist
Concerning screws in the distal fragments (articular segment):
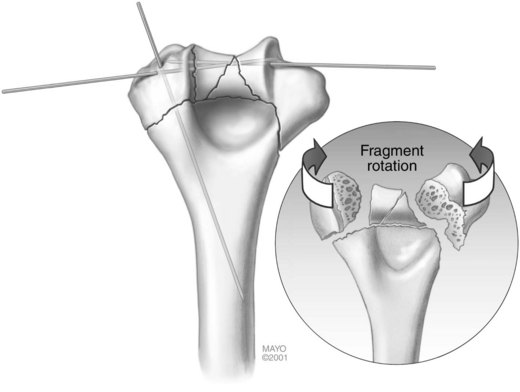
Step 1: articular surface reduction (Fig. 17.4)
The first step is articular surface reduction. The proximal ulna and radial head can be used as a template for the reconstruction of the distal humerus. Large articular fragments are provisionally fixed with smooth K-wires (Fig. 17.4). In cases with extensive comminution, fine threaded wires (1 mm) are used, then cut off and left in and used as ‘dowels’. It is necessary that these wires be placed close to the subchondral level, so as not to interfere with the passage of screws from the plates into the distal fragments. No screws are placed in the distal fragments until the plates are applied.
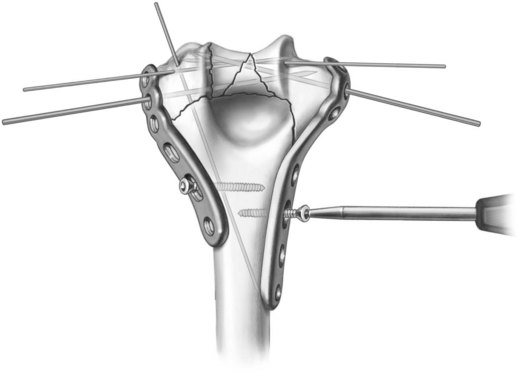
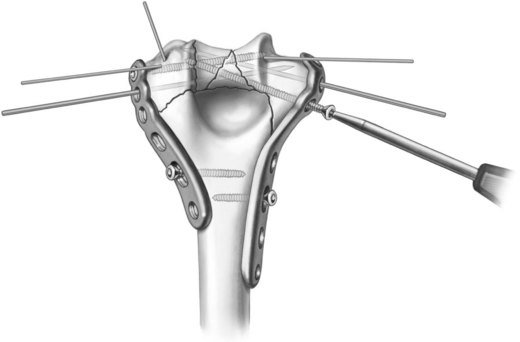
Step 2: plate placement and provisional fixation (Fig. 17.5)
Step 3: articular fixation (Fig. 17.6)
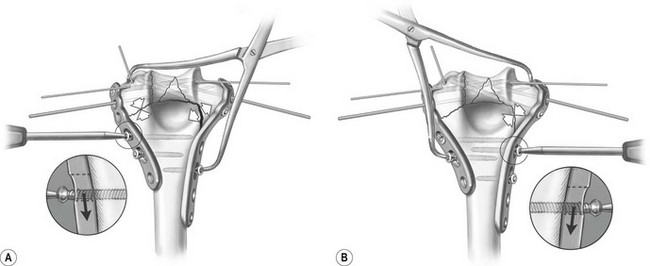
Step 4: supracondylar compression (Fig. 17.7)
The plates are then fixed proximally under maximum compression at the supracondylar level:
Step 5: final fixation (Fig. 17.8)
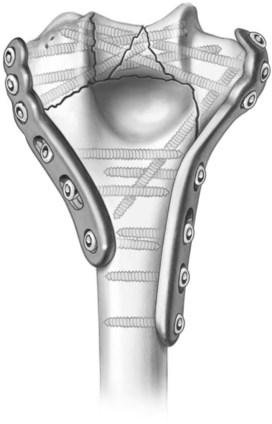
Figure 17.8 Step 5: final screw insertion. The smooth Steinmann pins are all removed and the remainder of the screws inserted. The distal screws interdigitate for maximum fixation in the distal articular fragments (as described in Fig. 3).
From Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. Surgical technique by investigation performed at the Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN. The original scientific article in which the surgical technique was presented was published in JBJS 2007; 89-A:961–969. Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
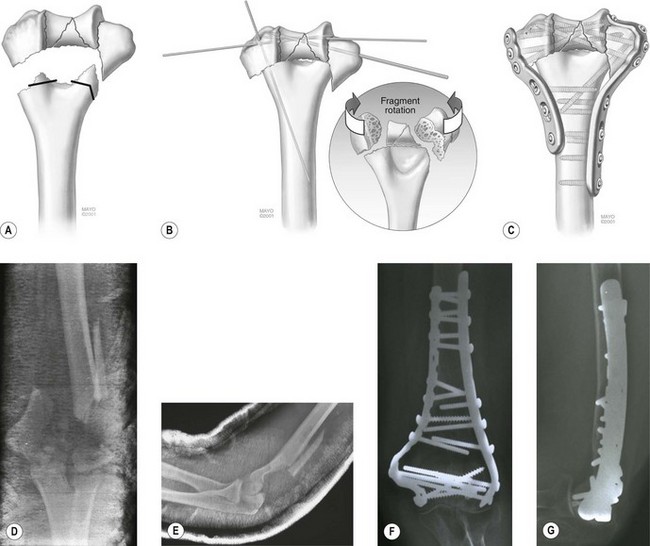
Dealing with metaphyseal bone loss
Adequate bony contact with interfragmentary compression in the supracondylar region is necessary to ensure the stability of the construct and eventual fracture union. If metaphyseal bone loss or comminution precludes an anatomical reconstruction with satisfactory bony contact, the humerus can be shortened at the distal end of the shaft. Correct alignment and geometry of the distal humerus must be confirmed. The distal segment is translated anteriorly to create a pseudo-’fossa’ for the radial head and coronoid. The shaft is burred out posteriorly to recreate an olecranon fossa. I refer to this alternative reconstructive technique as supracondylar shortening (Fig. 17.9). This technique is especially useful in cases of combined soft tissue and bone loss. Shortening by 1 cm or less has only a slight effect on triceps strength in terminal extension,6 and in cases of severe soft tissue and bone loss up to 2 cm of shortening can be tolerated without serious disturbance of elbow biomechanics.6
Outcome
Recent reports document our experience with this technique for complex distal humerus fractures.7,8 Thirty-four consecutive complex distal humeral fractures were fixed with two parallel plates applied (medially and laterally) in approximately the sagittal plane. Twenty-six fractures were AO type C3 and 14 were open. Thirty-two fractures were followed for a mean of 2 years.
1 O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113-134.
2 Sanchez-Sotelo J, Torchia M, O’Driscoll SW. Principle-based internal fixation of distal humerus fractures. Techn Hand Upper Extrem Surg. 2001;5(4):179-187.
3 O’Driscoll SW, Sanchez-Sotelo J, Torchia ME. Management of the smashed distal humerus. Orthop Clin North Am. 2002;33(1):19-33.
4 O’Driscoll SW. Optimizing stability in distal humeral fracture fixation. J Shoulder Elbow Surg. 2005;14(1 Suppl. S):186S-194S.
5 O’Driscoll S. The triceps-reflecting anconeus pedicle (TRAP) approach for distal humeral fractures and nonunions. Orthop Clin North Am. 2000;31:91-101.
6 Hughes RE, Schneeberger AG, An K-N, et al. Reduction of triceps muscle force after shortening of the distal humerus: a computational model. J Shoulder Elbow Surg. 1997;6:444-448.
7 Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique: surgical technique. J Bone Joint Surg Am. 2008;90(Suppl. 2):31-46.
8 Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. J Bone Joint Surg Am. 2007;89(5):961-969.