Chapter 78 Fracture Complications After Anterior Cruciate Ligament Reconstruction
Anterior cruciate ligament (ACL) reconstruction is one of the most frequently performed operative procedures with more than 100,000 reconstructions performed annually in the United States alone.1 Autogenous bone–patellar tendon–bone (BPTB) presents the most frequently used graft choice by orthopaedic surgeons in the United States, Canada, and Europe.2 This procedure includes creation of large bony defects in the tibia, femur, and patella for graft harvesting and fixation.2,3 The effects of bony defects on bone strength have become a major concern in orthopaedic trauma surgery, and their relevance in the development of postoperative fracture after ACL reconstruction is increasingly recognized.4,5 Complications have been reported to occur in 1.8% to 24% of ACL reconstructions.6–8 Serious complications after ACL reconstruction include arthrofibrosis, donor site pain, patella tendinitis, patella tendon rupture, and avascular necrosis of the femoral condyles. Fracture following ACL reconstruction presents a devastating complication that may involve the tibia, patella, or femur.
Femur Fracture
Femur fracture following ACL reconstruction has been reported in isolated cases as a result of distal femoral bone defects created for extraarticular fixation of a GoreTex prosthetic graft,9 a ligament augmentation device,10 iliotibial band tenodesis,11 or femoral post fixation.12 Supracondylar femur fracture after arthroscopic ACL reconstruction without intraoperative complications or use of supplemental fixation has also been reported.13,14 Fracture of the femoral diaphysis has also been described after ACL reconstruction and was caused by multiple perforations of the Beath pin trough’s femoral metaphyseal–diaphyseal junction.15 Although femur fractures are reported with increasing frequency after ACL reconstruction, this complication is likely underreported and its exact incidence is not known.
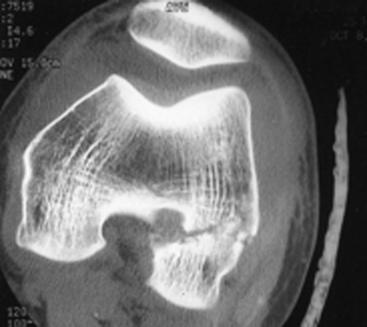
Physical examination in patients with this complication always produces marked tenderness, muscular guarding, bony crepitation, and a large effusion. Plain radiographs and computed tomography (CT) scans are helpful to identify the fracture pattern and will often show that the fracture occurred through the intraosseous tunnel created in the posterior distal femur. CT scans may demonstrate increased bone tunnel diameter (Fig. 78-1).
Several factors predispose the anatomical area of the femoral tunnel to developing a distal femur fracture after arthroscopic ACL reconstruction. The presence of the large femoral tunnel likely acts as a predisposing factor due to the localized stress-rising effect of the bony defect.16–20 This effect results from a concentration of local stresses around the femoral defect and reduced energy-absorbing capacity from the decreased amount of bone available to withstand the applied load.17 Because bone with stress concentration behaves in a more brittle fashion, the increased local stresses can reach the ultimate stress of the bone at much lower applied loads.19 Depending on the geometry of the defect, strength reductions of 20% to 90% may occur.18,19 Insertion of allogenic or autogenous bone graft into the defect, such as in BPTB ligament reconstruction, has not been shown to significantly change the mechanical weakening of the bone.19 The combination of greater localized stresses and decreased load-absorbing capacity predisposes the area of the defect to failure. Aside from the bony defect, additional stress concentration in the distal femur results from the change in the bony moment of inertia due to the acute change of sagittal, axial, and coronal geometry of the posterior condylar flare and intercondylar notch.18,19 The bony geometry of the distal femur has been found to play a critical role in the structural properties and prediction of fracture load.21,22 Geometric analysis of the distal femur has shown the thinnest cortical shell to be in the posterior aspect of the distal femur,23 therefore predicting the lowest fracture load in the anatomical region of the femoral tunnel.
Decreased bone mineral density of up to 20% has been observed after knee ligament injury and may also contribute to the increased fracture risk after ACL reconstruction due to decreased bending strength in the distal femur.22,24 Bone bruising of the lateral femoral condyle, which is frequently associated with ACL rupture, may also compromise the biomechanical properties in the lateral femoral condyle and predispose to earlier failure of the bruised bone.25 When the area of the bony defect is subjected to tensile stress, as with extension trauma to the knee, the load strength of the already vulnerable posterior distal femur is even further reduced.17,18 However, because the bone in this anatomical region is predominantly under compression, the likelihood of fracture development and crack propagation is decreased. This may explain why femur fracture does not occur more frequently after arthroscopic ACL reconstruction.
Because bony remodeling has been shown to decrease stress concentration around bony defects after 8 to 12 weeks,18 this would be expected to decrease the predisposition for femur fracture after ACL reconstruction. However, bone tunnel healing of the femoral tunnel has been shown to be delayed by the exposure to biological factors from the joint.26 A previous report demonstrating fracture through the femoral tunnel 2 years after ACL reconstruction27 suggests that the stress concentration effect of the femoral tunnel continues for a prolonged period after surgery.
Bone tunnel enlargement after ACL reconstruction is well documented and occurs in as many as 68% of cases after ACL reconstruction. The etiology of this clinical phenomenon is not completely understood, but it is thought to be related to a combination of multiple biological and mechanical factors. A better understanding of the clinical relevance of bone tunnel enlargement is still evolving.28 Previous experimental studies have shown that the breaking strength of bone decreases in direct proportion to the size of a bony defect.16 Based on these findings, enlargement of the femoral tunnel may have clinical relevance for the development of supracondylar femur fracture after ACL reconstruction by further decreasing the mechanical fracture resistance. Bone tunnel enlargement has also been suggested to increase the risk for tibial plateau fracture after ACL reconstruction.5,29 Given the frequency of ACL reconstruction and high incidence of bone tunnel enlargement, the potential predisposing effect of this phenomenon for fracture of the distal femur needs to be further examined.
During ACL reconstruction, a tunnel is drilled into the distal femur for subsequent graft fixation. Femoral tunnel placement is performed arthroscopically in accordance with recent technique recommendations.2,3 To optimize graft positioning, the femoral tunnel is placed as far posterior as possible while carefully avoiding disruption of the posterior cortex. This is commonly achieved by the use of a femoral tunnel placement guide with built-in offset that maintains a 1- to 2-mm-thick posterior cortical rim. Disruption of the posterior cortex can result from posterior placement of the femoral tunnel.7 This complication is different than fracture through the femoral tunnel. However, it should be carefully avoided because it may facilitate development of a fracture of the lateral femoral condyle12 (Fig. 78-2). ACL reconstruction using computer-assisted navigation systems for tunnel placement or using a two-incision technique for ACL reconstruction may be able to reduce the risk for this complication.30
Anatomical open reduction is critical to avoid premature arthritis and may also be able to maintain the graft in the isometric position. Fracture fixation by interfragmentary screws, supracondylar blade plate, dynamic compression plate, and intramedullary nail has all been described9–12 after femur fracture following ACL reconstruction. Permanent loss of knee motion has been described in some cases after distal femoral fracture fixation.10,12,15 Early open reduction and internal fixation using condylar locking plates provide effective fracture fixation with limited soft tissue dissection and reduced postoperative morbidity and may allow for graft retention.13 A proactive treatment approach facilitates early recovery, full range of motion, excellent subjective knee rating, high functional outcome scores, and return to pivoting sports.13 Following anatomical fracture fixation, intraoperative stability testing may reveal a functional ACL graft without the need for revision ACL reconstruction. If anatomical fracture fixation does not maintain graft function, revision ACL reconstruction may be performed at the time of fracture fixation or at a later time.
Patella Fracture
Patella fracture represents a devastating complication following ACL reconstruction using BPTB autograft and has been reported with an incidence of 0.2 to 0.8%.5,31,32 Patella fractures after ACL reconstruction are more frequently observed in women and older patients.33 These fractures can occur intraoperatively or postoperatively. Intraoperative fractures are very rare and most often result from technical errors such as harvesting too large a bone block. More frequently, injuries occur between 5 and 12 weeks postoperatively.31,32,34 These fractures in the early postoperative period are considered a major complication because they may interfere with graft remodeling and produce significant chondral damage and persistent anterior knee pain. Most fractures are transverse and occur at the proximal margin of the defect created during bone block harvesting35 (Fig. 78-3). The transverse fracture pattern usually results from indirect injuries to the patella, such as rapid eccentric contractions of the quadriceps muscle. Stellate and Y-type fracture patterns have been described after direct-impact injuries to the weakened patella.36 Longitudinal patella fractures may also occur from vertical troughs created by past-pointing with the saw blade. Patella fractures can be displaced or nondisplaced and may or may not be symptomatic.36,37 Most fractures cause a disturbance of the extensor mechanism and are easily diagnosed. However, silent nondisplaced patella fractures have been reported after ACL reconstruction as a cause of chronic anterior knee pain and long-term functional limitation.37
Multiple factors have been suggested to contribute to the development of this complication. Decreased vascularity to the central portion of the patella after graft harvest has been suggested to contribute to the risk for postoperative patellar fracture. The intraosseous blood supply of the patella is composed of the midpatellar, polar, and quadriceps tendon system.38 The disruption of these vessels during graft harvest can impair healing of the harvest site and may even affect the remaining normal bone.
In knee flexion, the patella is subject to posterior forces along the superior and inferior poles and an opposing anterior force when the posterior surface of the patella contacts the femur. This three-point bending force on the patella has been hypothesized to be the force that acts on the weakened patella, resulting in many of the indirect patella fractures that occur when the knee is flexed.39
Biomechanical studies have shown that the anterior cortex of the patella has the highest load resistance and that superior transverse cuts during graft harvest can reduce patellar resistance by 30% to 40%.31 The transverse bone cut has been shown to average more than 13 mm in width because of subtle motion of both the patella and the cutting instrument. Attention to surgical technique with smaller transverse bone cuts can help minimize the weakening effect on the anterior patellar cortex. Drill holes at the corners of the planned osteotomy can also be helpful to prevent past-pointing and undesired propagation of the bone defect beyond the outline of the osteotomy. Several authors have pointed out that the dimensions of the grafted bone plug should not exceed 9 to 10 mm in width. Using a 7-mm-wide sagittal blade and angling the blade can reduce the width of the true traversal cut. In addition to the width of the bone defect, its length and depth are important. Graft length of less than 50% to 66% of the patellar length is recommended with minimum graft length of 20 mm.40 Similarly, depth of the graft should not exceed one-third of the measured depth of the patella.41
Harvesting the BPTB graft acts as a significant stress riser on the patellar bone.42 This stress-rising effect is directly correlated with the size of the bone defect. Tapered bone defects cause less patellar stress concentration compared with square or trapezoidal defects but are still associated with significantly higher stress concentration than in the normal patella. Taking the larger trapezoidal bone plug from the tibia and a triangular plug from the patella has been suggested as a technique to reduce the patellar defect size and stress concentration.40,43 Packing the patella defect with cancellous bone grafts has been recommended by many authors.38,40–42,44–47 Bone grafting has been shown to decrease the stress-rising effect and can help to normalize the strength and resistance of the harvest site.44 Grafting the bony defect is particularly recommended for graft sites wider than 10 to 12 mm or deeper than 6 mm.38 In addition to graft size and shape, the grafting technique is also important. Use of a circular oscillating saw can create lower stresses on the corners, removes smaller grafts, and creates a rounded bottom of the trough.48
It has been theorized that some patella fractures after ACL reconstruction result from a weakened patella and abnormal patellar tracking due to a deconditioned quadriceps, which in turn increases the patellofemoral contact stresses. Early quadriceps conditioning and proprioceptive exercises decrease abnormal patellar positioning and tracking.5,31 Improved quadriceps strength and function may also help restore normal gait pattern and thereby prevent direct fractures from falls or from sudden uncoordinated muscle contraction.
Nondisplaced fractures can be treated nonoperatively with rigid knee bracing. However, some authors advocate surgical fixation for all fractures because it restores the extensor mechanism and allows for immediate motion and rapid return to knee rehabilitation.31 We have successfully used cannulated screw fixation with figure-eight Fiberwire augmentation through the cannulated screws for these nondisplaced fractures. With appropriate treatment, minimal residual long-term consequences have been observed after patella fractures following ACL reconstruction with functional outcomes, comparable to patients without fracture complications.12,40
Tibia Fracture
Tibial Plateau Fracture
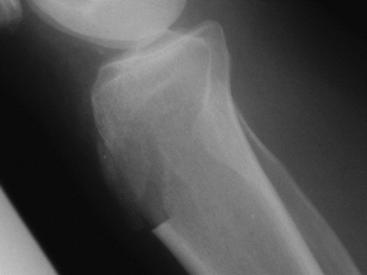
To date, six reports have described tibial plateau fracture complicating ACL reconstruction4,29,49–52 (Fig. 78-4). The fractures occur between 7 and 18 months postoperatively and are frequently induced by torsional trauma. Examination typically reveals a significant effusion and notable crepitation. Plain radiographs and CT scans are diagnostic. In all described cases, the fracture of the tibial plateau occurred through the transosseous tibial tunnel. Although no biomechanical studies have specifically addressed the mechanical effect of tibial bone tunnels, the presence of the tibial tunnel likely acts as a predisposing factor because the cortical defect acts as a stress riser.17,20 It has been well documented that cortical defects can decrease resistance to torsional forces by as much as 90%.19,20 Stress concentration is known to occur in the region of the anterior starting point of the tibial tunnel from the sudden change of the anatomical geometry of the metaphyseal–diaphyseal junction of the tibia.17 Screw holes used for post and washer fixation of the tibial graft may further increase the stress concentration. Bone tunnel enlargement has also been suggested to increase the risk for tibial fracture after ACL reconstruction.5,51
Treatment of tibial plateau fractures after ACL reconstruction has been successfully achieved by nonoperative treatment for nondisplaced fractures50 or by open reduction and internal fixation.4,5,49 Less invasive fracture fixation (LISS) (Synthes, Paoli, PA) (see Fig. 78-4) has been described with minimal postoperative morbidity and early functional recovery.51 Depending on the ability of the fracture fixation to maintain the graft in the isometric position, revision ACL reconstruction may5 or may not be necessary.51
Tibial Tubercle Fracture
Tibial tuberosity avulsion fractures have been described in rare cases of autograft BTB reconstructions.53–55 Tibial tubercle avulsion may occur ipsilaterally with primary ACL reconstruction or in the contralateral leg when using the contralateral patellar tendon autograft in revision cases. These injuries usually occur in the early postoperative period and have been described between the first postoperative day and 6 weeks postoperatively. The early occurrence of these injuries has been related to technical errors, early mechanical overload from aggressive postoperative weight bearing, and the combined stress-riser effect of the tibial bone plug harvest site and the tibial tunnel. Fractures may involve the entire tubercle or only a part of the tibial tuberosity. Patients commonly report a popping sensation with acute pain and associated inability or difficulty to extend the involved extremity. Radiographs are necessary to differentiate a tibial tubercle fracture from a patellar tendon avulsion, which can present with the same clinical findings (Fig. 78-5).
Harvesting of the central part of the tibial tubercle graft creates a thin cancellous bone bridge between the graft site and tibial tunnel. The tibial cortical defects result in a significant stress concentration, particularly on the medial aspect of the tibial tubercle. Undermining the medial or lateral insertion sites of the patellar tendon with the osteotome or oscillating saw causes further thinning of the bone bridge, which in some cases may lead to avulsion fractures. Undermining may result from a failure to account for the anatomical slope of the tibial tuberosity when making the bone cuts. Bone cuts perpendicular to the extremity axis lead to undermining, particularly of the lateral tibial tuberosity with its posterolateral slope. Sawing perpendicular to the tuberosity reduces the tendency to undermine the lateral tuberosity.53 Harvesting triangular bone blocks has also been proposed to minimize undermining and stress concentration.53 The use of round-cornered or trapezoidal bone cuts also helps minimize the stress-riser effect at the graft site. Lack of active knee extension and displacement of the fragment are indications for surgical fixation. The combination of interfragmentary screw fixation and tension band techniques provides rigid fixation that allows for immediate passive range-of-motion postoperatively and return of unrestricted knee function.53–55
In summary, fracture after ACL reconstruction is an infrequent but serious complication. Knowledge of the pathogenesis, risk factors, and specific anatomical and technical aspects that can lead to fracture complications after ACL reconstruction are important for the surgeon performing ACL reconstruction and can help prevent these devastating complications. Patients should be routinely counseled regarding these potential complications, particularly when BTB autograft is harvested.
1 Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat. 1998;139:1-119.
2 Fineberg MS, Zarins B, Sherman OH. Practical considerations in anterior cruciate ligament replacement surgery. Arthroscopy. 2000;16:715-724.
3 Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 1997;79A:1556-1576.
4 Delcogliano A, Chiossi S, Caporaso A, et al. Tibial plateau fracture after arthroscopic anterior cruciate reconstruction. Arthroscopy. 2001;17:E16.
5 Brownstein B, Bronner S. Patella fracture associated with accelerated ACL rehabilitation in patients with autogenous patella tendon reconstructions. J Orthop Sports Phys Ther. 1997;26:168-172.
6 Small NC. Complications in arthroscopy: the knee and other joints. Arthroscopy. 1986;2:253-258.
7 Graf B, Uhr F. Complications of intraarticular anterior cruciate reconstruction. Clin Sports Med. 1988;7:835-848.
8 Hughston JC. Complications of anterior cruciate ligament surgery. Orthop Clin N Am. 1985;16:237-240.
9 Ternes JP, Blasier RB, Alexander AH. Fracture of the femur after anterior cruciate ligament reconstruction with a GORE-TEX prosthetic graft. Am J Sports Med. 1993;21:147-149.
10 Radler C, Wozasek GE, Seotz H, et al. Distal femoral fracture through the screw hole of a ligament augmentation device. Arthroscopy. 2000;16:737-739.
11 Noah J, Sherman OH, Roberts C. Fracture of the supracondylar femur after anterior cruciate ligament reconstruction using patellar tendon and iliotibial tenodesis. Am J Sports Med. 1992;20:615-618.
12 Berg EE. Lateral femoral condyle fracture after endoscopic anterior cruciate ligament reconstruction. Arthroscopy. 1994;10:693-696.
13 Mithoefer K, Gill TJ, Vrahas MS. Supracondylar femoral fracture after arthroscopic reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 2005;87A:1591-1596.
14 Wilson TC, Rosenblum WJ, Johnson DL. Fracture of the femoral tunnel after an anterior cruciate ligament reconstruction. Arthroscopy. 2004;20:E45-E47.
15 Wiener DF, Siliski JM. Distal femoral shaft fracture: A complication of endoscopic anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:244-247.
16 Bechtol CO, Lepper H. Fundamental studies in the design of metal screws for internal fixation of bone. J Bone Joint Surg. 1956;38A:1385.
17 Brooks DB, Burstein AH, Franke VH. The biomechanics of torsional fractures: the stress concentration effect of a drill hole. J Bone Joint Surg. 1970;52A:507-514.
18 Burstein AH, Currey J, Frankel VH, et al. Bone strength. The effect of screw holes. J Bone Joint Surg. 1972;54A:1143-1156.
19 Johnson BA, Fallat LM. The effect of screw holes on bone strength. J Foot Ankle Surg. 1997;36:446-451.
20 Clark CR, Morgan C, Sonstegard DA, et al. The effect of biopsy hole shape and size on bone strength. J Bone Joint Surg. 1977;59:213-217.
21 Augat P, Reeb H, Claes LE. Prediction of fracture load at different skeletal sites by geometric properties of the cortical shell. J Bone Miner Res. 1996;11:1356-1363.
22 Stromsoe K, Hoiseth A, Alho A, et al. Bending strength of the femur in relation to non-invasive bone mineral assessment. J Biomech. 1995;28:857-861.
23 Guy P, Krettek C, Manns J, et al. CT-based analysis of the geometry of the distal femur. Injury. 1998;29:C16-C21.
24 Sievanen H, Kannus P, Heinonen A, et al. Bone mineral density and muscle strength of lower extremities and long-term strength training, subsequent knee ligament injury and rehabilitation. Bone. 1994;15:85-90.
25 Johnson DL, Bealle DP, Brand JC, et al. The effect of geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med. 2000;28:152-155.
26 Berg EE, Pollard ME, Kang Q. Intraarticular bone tunnel healing. Arthroscopy. 2001;17:189-195.
27 Manktelow AR, Haddad FS, Goddard NJ. Late femoral condyle fracture after anterior cruciate ligament reconstruction. Am J Sports Med. 1998;26:587-590.
28 Wilson TC, Kantaras A, Atay A, et al. Tunnel enlargement after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:543-549.
29 Thietje R, Faschingbauer M, Nurnberg HJ. Spontaneous fracture of the tibia after replacement of the anterior cruciate ligament with absorbable interference screws. A case report and review of the literature. Unfallchirurg. 2000;103:594-596.
30 Koh J. Computer-assisted navigation and anterior cruciate ligament reconstruction: accuracy and outcomes. Orthopedics. 2005;28:S1283-S1287.
31 Viola R, Vianello R. Three cases of patella fractures in 1320 anterior cruciate reconstructions with bone-patellar tendon-bone autograft. Arthroscopy. 1999;15:93-97.
32 Papageorgiou CD, Kostopoulos VK, Moebius UG, et al. Patellar fractures associated with medial-third bone-patellar tendon-bone autograft ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2001;9:151-154.
33 Sharkey NA, Donahue SW, Smith TS, et al. Patellar strain and patellofemoral contact after bone-patellar tendon-bone harvest for anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 1997;78:256-263.
34 Carreira DA, Fox JA, Freedman KB, et al. Displaced nonunion patellar fracture following use of a patellar tendon autograft for ACL reconstruction: case report. J Knee Surg. 2005;18:131-134.
35 Steen H, Tseng KF, Goldstein SA, et al. Harvest of patellar tendon (bone-tendon-bone) autograft for ACL reconstruction significantly alters surface strain in the human patella. J Biomech Eng. 1999;121:229-233.
36 Simonian PT, Mann FA, Mandt PR. Indirect forces and patella fracture after anterior cruciate ligament reconstruction with the patellar ligament. Am J Knee Surg. 1995;8:60-65.
37 Morgan-Jones RL, Cross TM, Caldwell B, et al. “Silent” transverse patellar fracture following anterior cruciate ligament reconstruction. Arthroscopy. 2001;17:997-999.
38 Benson ER, Barnett PR. A delayed transverse avulsion fracture of the superior pole of the patella after anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:85-88.
39 Carpenter JE, Kasman R, Matthews LS. Fractures of the patella. Instr Course Lect. 1994;43:97-108.
40 Christen B, Jakob R. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg. 1992;74B:617-619.
41 Malek MM, Kunkle KL, Knable KR. Intraoperative complications of arthroscopically assisted ACL reconstruction using patellar tendon autograft. Instr Course Lect. 1996;45:297-302.
42 Friis EA, Cooke FW, McQueen DA. Effect of bone block removal and patellar prosthesis on stresses in the human patella. Am J Sports Med. 1994;22:696-701.
43 DuMontier TA, Metcalf MH, Simonian PT, et al. Patella fracture after anterior cruciate ligament reconstruction with the patellar tendon: a comparison between different shaped bone block excisions. Am J Knee Surg. 2001;14:9-15.
44 Stein DA, Hunt SA, Rosen JE, et al. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18:578-583.
45 Roberts TS, Drez DJr, Parker W. Prevention of late patellar fracture in ACL deficient knees reconstructed with bone-patellar tendon-bone autografts. Am J Knee Surg. 1989;2:83-88.
46 Daluga D, Johnson C, Bach BRJr. Primary bone grafting following graft procurement for anterior cruciate ligament insufficiency. Arthroscopy. 1990;6:205-208.
47 Ferrari JD, Bach BRJr. Bone graft procurement for patellar defect grafting in anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:543-545.
48 Jackson DW, Cohn BT, Morrison DS. A new technique for harvesting the patella tendon in patients undergoing anterior cruciate ligament reconstruction. Orthopedics. 1990;13:165-167.
49 El-Hage ZM, Mohammed A, Griffiths D, et al. Tibial plateau fracture following allograft anterior cruciate ligament (ACL) reconstruction. Injury. 1998;29:73-74.
50 Morgan E, Steensen RN. Traumatic proximal tibial fracture following anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11:193-194.
51 Mithoefer K, Gill TJ, Vrahas MS. Tibial plateau fracture following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:325-328.
52 Sundaram RO, Cohen D, Barton-Hanson N. Tibial plateau fracture following gracilis-semitendinosus anterior cruciate ligament reconstruction: the tibial tunnel stress-riser. Knee. 2006;13:238-240.
53 Busfield BT, Safran MR, Cannon WD. Extensor mechanism disruption after contralateral middle third patellar tendon harvest for anterior cruciate ligament revision reconstruction. Arthroscopy. 2005;21:1268.
54 Acton KJ, Dowd GS. Fracture of the tibial tubercle following anterior cruciate ligament reconstruction. Knee. 2002;9:157-159.
55 Moen KY, Boynton MD, Raasch WG. Fracture of the proximal tibia after anterior cruciate ligament reconstruction: a case report. Am J Orthop. 1998;27:629-630.