CHAPTER 77 Fractional resurfacing
History
Non-ablative fractional photothermolysis was first introduced in 2005 with the introduction of the 1550-nm erbium-doped fiber laser (Reliant Technologies, Mountain View, CA). Initially the laser was approved for the soft tissue coagulation application, based largely on early studies of forearm tissue. In 2005 Khan et al. reported on the use of the first fractional resurfacing device, a 1550-nm erbium-doped fiber prototype laser system that produced microscopic columns of thermal injury surrounded by intact tissue using a handpiece that scanned across the skin up to 8 cm/second while delivering the microarray pattern to the skin. These microscopic treatment zones (MTZs) range in diameter from 70 to 100 micrometer in diameter and 250 to 800 micrometer in depth and are produced by varying the depth of the focused beam. Tissue in these coagulated zones is not vaporized and the epidermis and stratum corneum are left intact leaving the skin erythematous, edematous, but without evidence of wounding. The device is FDA cleared for the treatment of periorbital rhytids, pigmentary alteration, melasma, skin resurfacing, and surgical scars.
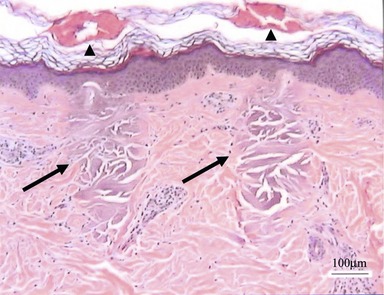
The handpiece of the fractionated laser makes direct contact with the skin’s surface and uses an intelligent optical tracking system to deliver an even array of MTZs. These are columns of tissue coagulation that show no loss in the integrity of the overlying stratum corneum (Fig. 77.1). The incipient wound healing cascade and inflammatory response in which heat shock protein-70 is a central player, initiates a number of incompletely understood events that leads to increase in collagen synthesis and collagen reorganization. Healing also involves the extrusion of damaged epidermal components, termed microepidermal necrotic debris (MEND), which clinically could be observed as a superficial exfoliation following treatment that imparts a fine rough sand paper-like feel to the skin and is associated with a mild bronzing color of the skin in the areas of treatment. This clinically translates into the observed improvement in photodamage, including softening of rhytids, tightening of pore ostia, improvement in dyschromia, and a general textural smoothening of the skin.
Physical evaluation
The cosmetic consultation visit should focus on the following:
• Complete past medical and surgical procedures including complication in the postprocedural periods.
• History of hypertrophic scarring and/or keloid formation. While there is a low risk of scarring from fractional resurfacing, a positive history of hypertrophic scarring and/or keloid formation is a marker of a perturbed wounding response and signal that caution should be exercised in treating these patients. Closer follow-up and possibly less aggressive initial treatments should be undertaken until an assessment of an individual patient’s response to therapy can be made.
• History of herpes labialis and/or HSV infections elsewhere, use of antivirals and antibiotics in the past, and allergies to these are significant. Patients with active bacterial and viral infections should delay fractional resurfacing treatments until these issues have resolved. Routine use of prophylactic antivirals is recommended for three days starting on the day of treatment.
• History of isotretinoin use over last 6 months. These patients should be excluded from treatment because of a theoretical increased risk of scarring.
• History of smoking. Patients who smoke generally heal less favorably.
• Plans for UV exposure should be gauged before the procedure as UV avoidance is necessary immediately following treatments and during the healing period.
• Thorough physical exam noting scars, dyschromia, rhytids, and skin phototype are important considerations in selection of treatment settings for particular applications.
• Photography is useful for patient feedback and part of the medical record for later reference.
Complications
Pearls & pitfalls
Pearls
• Acne and other scars should be treated as early as possible following an inciting insult. We have observed improved responses in more recent scars as compared to older ones. Surgical scars can be safely treated as early as one month following an uneventful surgery and postop recovery (Figs 77.2–77.4).
• Eyelids can be treated safely and rapidly by retraction of the eyelid skin over the orbital rim and limiting treatment to the portion of the lid that can be retracted, or in the case where eyeshields are used, to the lid margin. Rejuvenation and, in some cases, tightening may be achieved (Figs 77.5–77.7).
• When treating scarring, patients should be advised that more treatments give more results. It should be clearly stated, however, that scars cannot be erased.
• In contrast to ablative laser systems, off the face fractional resurfacing is safe and effective and has a negligible risk of scarring.
• Both hyperpigmentation and hypopigmentation can be improved with fractional resurfacing. This conundrum has yet to be explored (Figs 77.8, 77.9).


Fig. 77.2 Pre- (A) and post-treatment (B) photographs of a patient with a depressed surgical scar on the forehead treated with a series of fractional photothermolysis treatments. Improvement in pigmentation, depression and overall quality of the scar is evident.
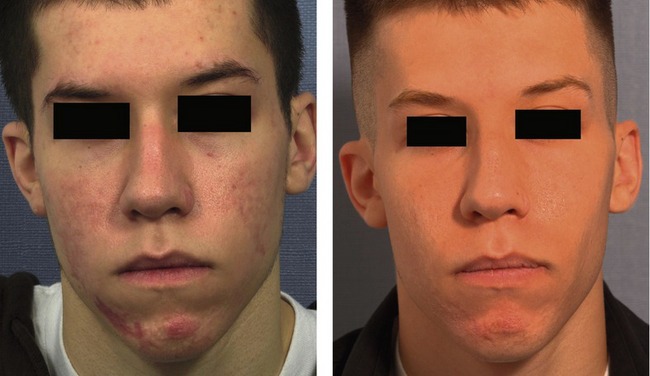


Fig. 77.4 Dramatic improvement in acne scarring is evident following a series of fractional photothermolysis treatments.
Adapted from Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med 2006;38:169–176. Reprinted with permission of John Wiley & Sons, Inc.


Figs 77.5, 77.6 and 77.7 Upper eyelid tightening and improvement in eyelid aperture is observed in these patients following a series of fractional photothermolysis treatments.
Fig. 77.7 Adapted from Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med 2006;38:169–176. Reprinted with permission of John Wiley & Sons, Inc.
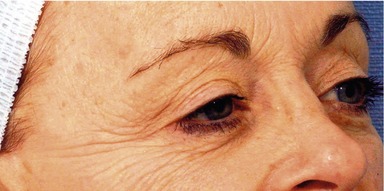

Figs 77.5, 77.6 and 77.7 Upper eyelid tightening and improvement in eyelid aperture is observed in these patients following a series of fractional photothermolysis treatments.


Figs 77.5, 77.6 and 77.7 Upper eyelid tightening and improvement in eyelid aperture is observed in these patients following a series of fractional photothermolysis treatments.


Fig. 77.8 Pre- (A) and post-treatment (B) photographs of a patient with melasma treated with a series of fractional resurfacing treatments. Improvement in melasma and hypopigmentation is also noted.
Adapted from Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med 2006;38:169–176. Reprinted with permission of John Wiley & Sons, Inc.
Pitfalls
• Inadequate cooling of the epidermis and too many repetitive passes may lead to bulk heating of the epidermis and lower layers of the skin that can result in blistering, wounding and scar formation.
• Reactivation of zoster virus and herpes simplex virus can be incited by any resurfacing method, including fractional resurfacing. As a significant portion of the general patient population sheds herpes simplex virus asymptomatically, it is imperative to prophylax with oral antiviral medication against reactivation of viral infection. Failure to do so could potentially be a serious pitfall.
• Aggressive treatment of melasma, especially in darker skin phototypes, could lead to worsening of the pigmentary alteration. It is best advised to approach such cases with caution, with lighter treatments perhaps in a “test” area to gauge a particular patient’s response to therapy.
• Unrealistic patient expectations may result in premature termination of the treatment course before full benefit is realized. Realistic patient expectations should be established during the initial consultation, and care should be taken to avoid “over-selling” the benefits of therapy. Full disclosure to a patient fully educated about the potential benefits, risks, expectations, and limitations of therapy are essential to avoid this pitfall.
• Patients with severe photodamage are not optimal candidates for fractional resurfacing. Improvement is expected to be only modest in this group. It is best to offer other methods of rejuvenation, including surgical methods and appropriate referrals, in the best interest of the patient to avoid the pitfall of a disappointed patient at the endpoint of therapy.
Summary of steps
1. Clean the skin, followed by degreasing and topical anesthesia.
2. The handpiece of the laser device makes direct contact with the skin and is rolled along the area in linear fashion.
3. The treatment energy and treatment density can be varied depending on the application.
4. Divide the face into cosmetic subunits. Treatment of contralateral subunit is completed followed by the other side of the same subunit before moving on to another subunit.
5. The maximum speed is inversely related to the treatment energy selected and with the selected MTZ density.
6. For treating scars, we tend to use a higher treatment energy with lower total density.
7. Dyschromias are best treated with more superficial penetration of the laser; thus a lower treatment energy at higher density is our choice.
8. For the application to textural improvement such are rhytids and other photoaging applications, a medium treatment energy is selected with higher density.
9. For the application to photorejuvenation of the skin, 3–5 treatments are the usual recommendations for optimal improvement.
10. Our practice is to routinely use prophylactic oral antivirals beginning the day of treatment for three days in total, with the goal of preventing reactivation of herpes virus.
Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33:295–299.
Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220:524–527.
Fisher GH, Geronemus RG. Short term side effects of fractional photothermolysis. Dermatol Surg. 2005;31:1245–1249.
Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photo-aged facial skin. Arch Dermatol. 1996;132:395–402.
Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006;38:169–176.
Glaich AS, Rahman Z, Goldberg LH, Friedman PM. Fractional resurfacing for the treatment of hypopigmented scars: a pilot study. Dermatol Surg. 2007;33:289–294.
Khan MH, Sink RK, Manstein D, et al. Intradermally focused infrared laser pulses: thermal effects at defined tissue depths. Lasers Surg Med. 2005;36:270–280.
Khatri KA, Ross V, Grevelink JM, Magro CM, Anderson RR. Comparison of erbium:YAG and carbon dioxide lasers in resurfacing of facial rhytides. Arch Dermatol. 1999;135:391–397.
Manstein D, Herron GC, Sink RK, et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426–438.
Marra DE, Yip D, Fincher EF, Moy RL. Systemic toxicity from topically applied lidocaine in conjunction with fractional photothermolysis. Arch Dermatol. 2006;142:1024–1026.
Wanner M, Tanzi EL, Alster TS. Fractional photothermolysis: Treatment of facial and nonfacial cutaneous photodamage with a 1550-nm erbium-doped fiber laser. Dermatol Surg. 2007;33:23–28.