Commonly affect children, developmentally challenged or psychiatric patients, and inebriated adults
 Most ingested foreign bodies traverse GI tract without problem: < 1% cause obstruction or perforation
Most ingested foreign bodies traverse GI tract without problem: < 1% cause obstruction or perforation
• Retained surgical items
• Intentionally retained surgical material
 after ingestion. Swallowing batteries is relatively common and can cause bowel perforation or obstruction as the acid in the battery may leak out.
after ingestion. Swallowing batteries is relatively common and can cause bowel perforation or obstruction as the acid in the battery may leak out.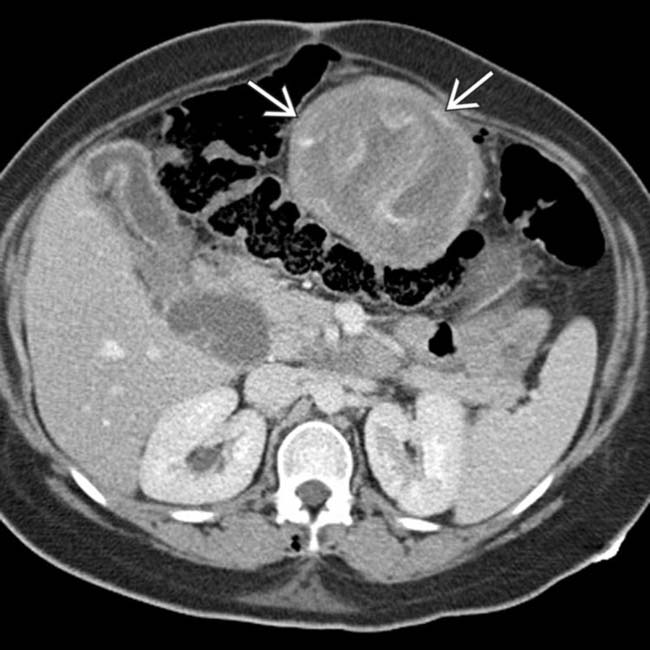
 . Note the wavy, serpiginous pattern within the mass and the well-defined wall.
. Note the wavy, serpiginous pattern within the mass and the well-defined wall.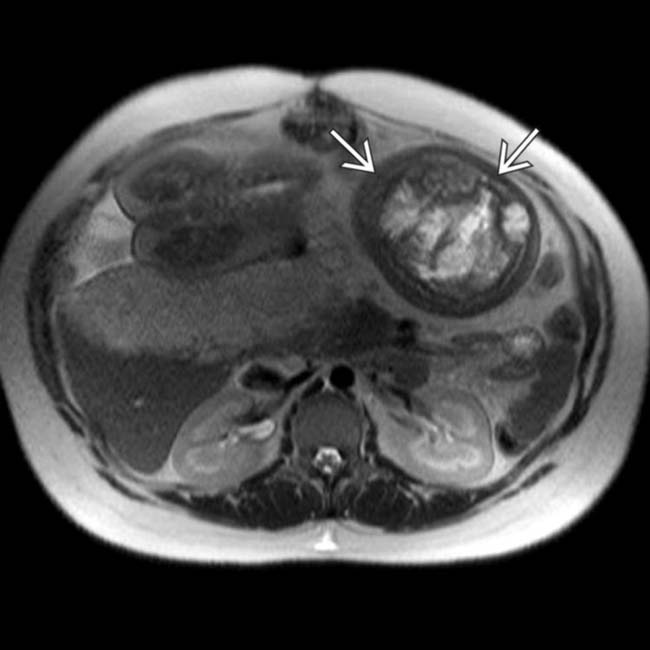
 , with wavy, high T2 signal and a well-defined T2-hypointense wall.
, with wavy, high T2 signal and a well-defined T2-hypointense wall.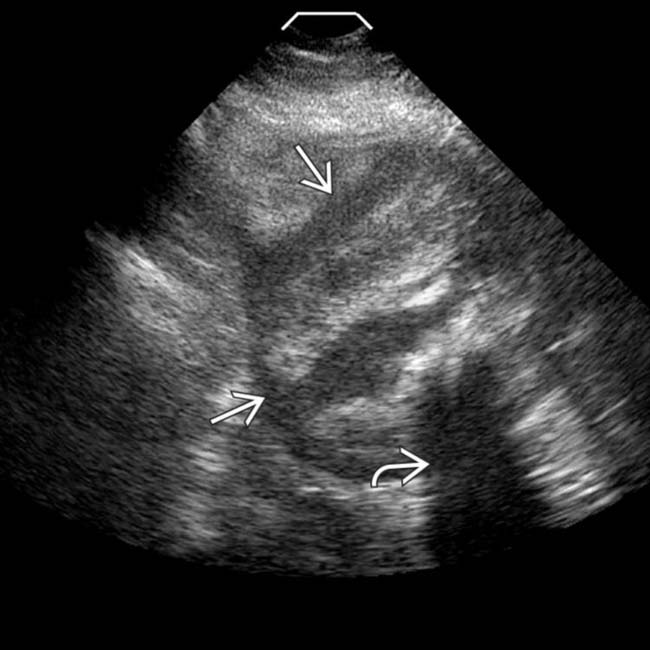
 and internal alternating bands of hyper- and hypoechogenicity. Some of the hyperechoic bands with posterior acoustic shadowing
and internal alternating bands of hyper- and hypoechogenicity. Some of the hyperechoic bands with posterior acoustic shadowing  may reflect gas within the mass.
may reflect gas within the mass.IMAGING
Ingested Foreign Bodies
• Commonly affected patient groups
• General principles
 Elongated or sharp objects may impact at point of intestinal narrowing or sharp angulation
Elongated or sharp objects may impact at point of intestinal narrowing or sharp angulation
 Common ingested foreign bodies and management
Common ingested foreign bodies and management
 Foreign bodies vary in radiopacity and conspicuity on radiography vs. CT
Foreign bodies vary in radiopacity and conspicuity on radiography vs. CT
 Examine entire GI tract for additional FBs
Examine entire GI tract for additional FBs
 Elongated or sharp objects may impact at point of intestinal narrowing or sharp angulation
Elongated or sharp objects may impact at point of intestinal narrowing or sharp angulation
 Common ingested foreign bodies and management
Common ingested foreign bodies and management
– Longer objects > 6 cm in length (eating utensils, toothbrushes) are unlikely to traverse duodenum and should be retrieved endoscopically
 Foreign bodies vary in radiopacity and conspicuity on radiography vs. CT
Foreign bodies vary in radiopacity and conspicuity on radiography vs. CT
 Examine entire GI tract for additional FBs
Examine entire GI tract for additional FBs
– For most nonsharp foreign bodies, begin with visual inspection of oropharynx and plain radiographs
Inserted Foreign Bodies
• Objects may be inserted during sexual practice, as a result of an assault, to hide drugs and other illegal paraphernalia, or even sharp objects/weapons in prison setting
Retained Surgical Items
• Occurs in roughly 1/18,000 inpatient surgeries, but more common in abdomen (1/1,000-1,500 laparotomies)
• Crucial to distinguish intentional or expected objects from unintended
 Common intentional devices: Surgical drains, rubber retention sutures, metallic clips for wound closure, hemoclips, or intraarterial, intravenous, and intraintestinal catheters
Common intentional devices: Surgical drains, rubber retention sutures, metallic clips for wound closure, hemoclips, or intraarterial, intravenous, and intraintestinal catheters
 Common intentional devices: Surgical drains, rubber retention sutures, metallic clips for wound closure, hemoclips, or intraarterial, intravenous, and intraintestinal catheters
Common intentional devices: Surgical drains, rubber retention sutures, metallic clips for wound closure, hemoclips, or intraarterial, intravenous, and intraintestinal catheters• Identification of retained surgical sponges or towels on imaging
 Gossypiboma:Foreign body reaction to cotton fabric of sponge or towel left inside patient produces inflammatory mass with sponge at center
Gossypiboma:Foreign body reaction to cotton fabric of sponge or towel left inside patient produces inflammatory mass with sponge at center
 Gossypiboma:Foreign body reaction to cotton fabric of sponge or towel left inside patient produces inflammatory mass with sponge at center
Gossypiboma:Foreign body reaction to cotton fabric of sponge or towel left inside patient produces inflammatory mass with sponge at center
– Produces variable degree of inflammation, fibrosis, and adhesions to adjacent abdominal structures
Intentionally Retained Surgical Material
• Oxidized regenerated cellulose (Gelfoam or Surgicel)
 Bioabsorbable sterile knitted fabric deliberately left in place within surgical bed at end of procedure to produce hemostasis
Bioabsorbable sterile knitted fabric deliberately left in place within surgical bed at end of procedure to produce hemostasis
 Upon contact with blood, the fabric induces rapid hemostasis by inducing thrombus formation, and swells into gelatinous mass, trapping air (gas) within its interstices
Upon contact with blood, the fabric induces rapid hemostasis by inducing thrombus formation, and swells into gelatinous mass, trapping air (gas) within its interstices
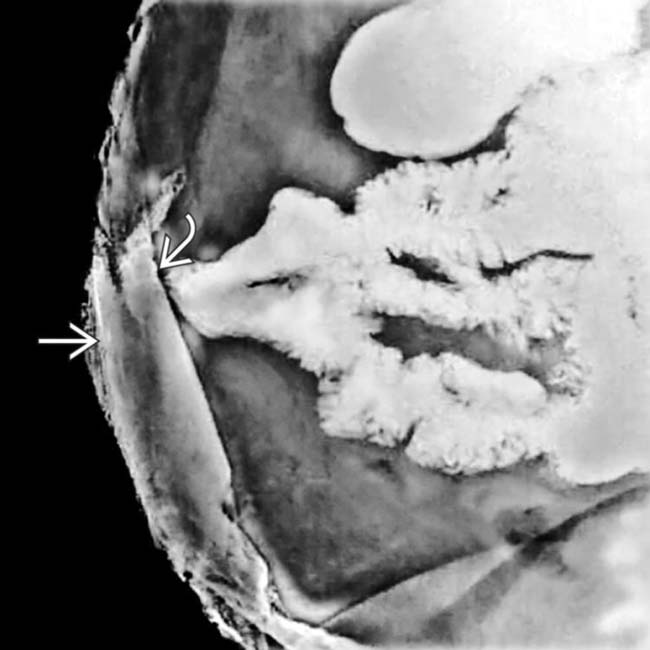
 Has radiographic and CT appearance of tightly packed, swirled, or linear gas bubbles without much fluid content
Has radiographic and CT appearance of tightly packed, swirled, or linear gas bubbles without much fluid content
 Bioabsorbable sterile knitted fabric deliberately left in place within surgical bed at end of procedure to produce hemostasis
Bioabsorbable sterile knitted fabric deliberately left in place within surgical bed at end of procedure to produce hemostasis Upon contact with blood, the fabric induces rapid hemostasis by inducing thrombus formation, and swells into gelatinous mass, trapping air (gas) within its interstices
Upon contact with blood, the fabric induces rapid hemostasis by inducing thrombus formation, and swells into gelatinous mass, trapping air (gas) within its interstices Has radiographic and CT appearance of tightly packed, swirled, or linear gas bubbles without much fluid content
Has radiographic and CT appearance of tightly packed, swirled, or linear gas bubbles without much fluid content

 in the small bowel, perforating the small bowel and extending into the abdominal wall.
in the small bowel, perforating the small bowel and extending into the abdominal wall.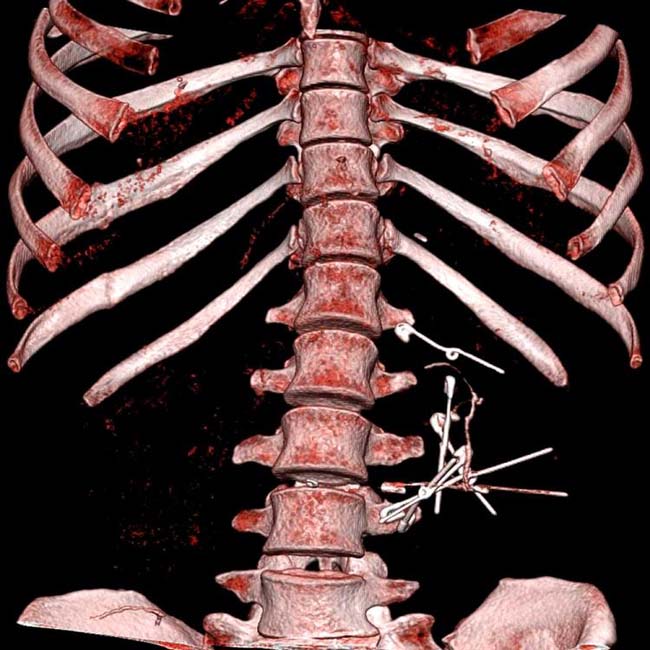

 within the bladder. The object turned out to be a penlight which was subsequently retrieved in the cystoscopy suite.
within the bladder. The object turned out to be a penlight which was subsequently retrieved in the cystoscopy suite.
 in the expected position of the rectum. Under general anesthesia the plastic dildo was retrieved.
in the expected position of the rectum. Under general anesthesia the plastic dildo was retrieved.
 has caused an inflammatory stricture
has caused an inflammatory stricture  of the adjacent small bowel, which is thickened with mucosal hyperemia.
of the adjacent small bowel, which is thickened with mucosal hyperemia.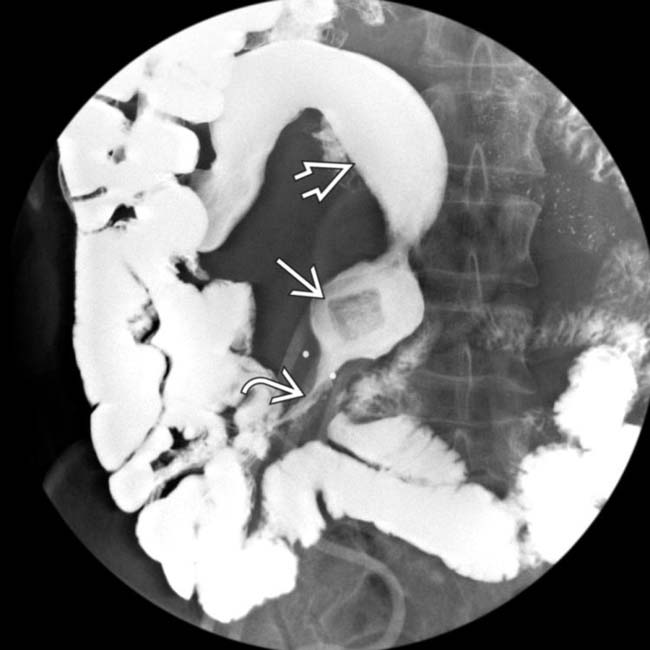
 corresponding to the clip seen on CT. Note that the stricture
corresponding to the clip seen on CT. Note that the stricture  in the immediately distal small bowel is causing mild obstruction of the dilated
in the immediately distal small bowel is causing mild obstruction of the dilated  proximal bowel.
proximal bowel.
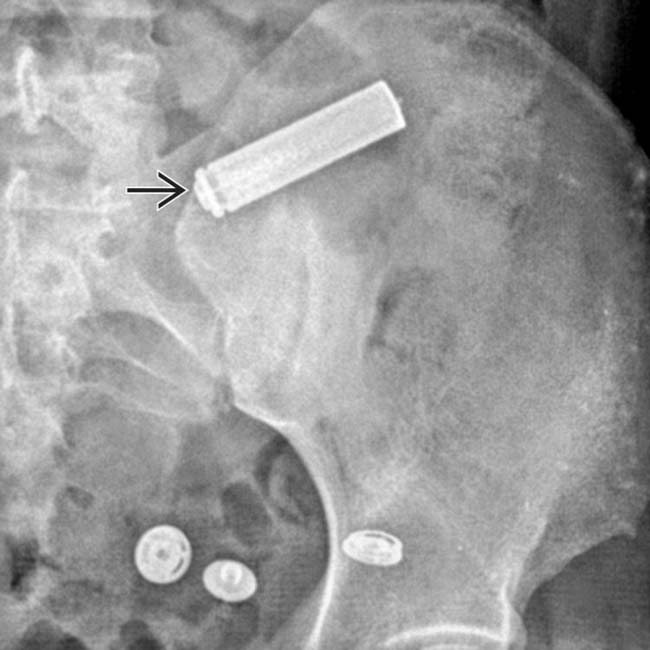
 in the pelvis, typical of a retained surgical sponge. This radiopaque tag can be directly woven into the sponge or can be attached to it.
in the pelvis, typical of a retained surgical sponge. This radiopaque tag can be directly woven into the sponge or can be attached to it.
 forming around the retained sponge, characteristic of a gossypiboma.
forming around the retained sponge, characteristic of a gossypiboma.
 consisting of swirled gas and soft tissue density, that was found to represent a surgical towel that had been left in the peritoneal cavity. Note the absence of a radiopaque marker.
consisting of swirled gas and soft tissue density, that was found to represent a surgical towel that had been left in the peritoneal cavity. Note the absence of a radiopaque marker.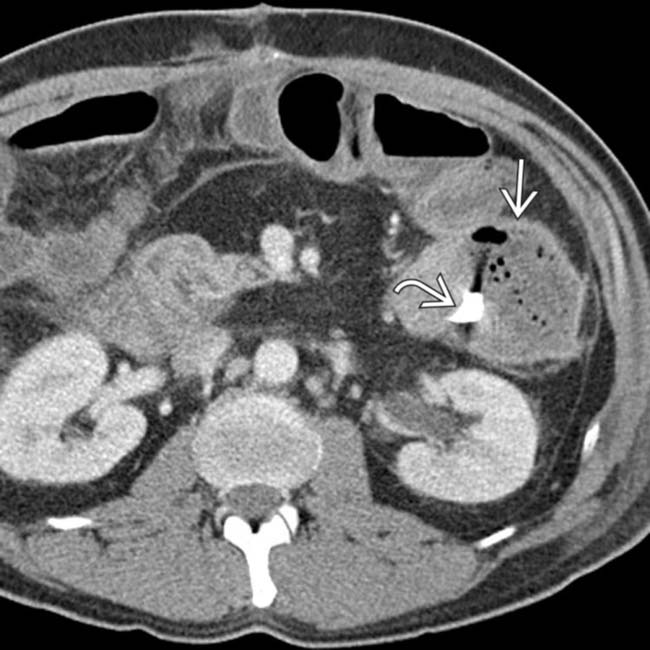
 with a well-defined wall and multiple foci of internal gas. Notice the radiopaque foreign body
with a well-defined wall and multiple foci of internal gas. Notice the radiopaque foreign body  within the collection.
within the collection.
 , and once again demonstrates the linear, band-like foreign body
, and once again demonstrates the linear, band-like foreign body  within the collection.
within the collection.
 incorporated into a surgical sponge. Also note the presence of a plastic ring
incorporated into a surgical sponge. Also note the presence of a plastic ring  within the abdomen connected to the surgical sponge.
within the abdomen connected to the surgical sponge.
 and its metal tip
and its metal tip  .
.
 with extravasation of barium into a bag
with extravasation of barium into a bag  overlying the anterior abdominal wall wound. At surgery, small bowel perforation was confirmed, and a plastic Bic pen was retrieved.
overlying the anterior abdominal wall wound. At surgery, small bowel perforation was confirmed, and a plastic Bic pen was retrieved.
 but little fluid in the cholecystectomy bed, mimicking an abscess. Note the adjacent surgical clips
but little fluid in the cholecystectomy bed, mimicking an abscess. Note the adjacent surgical clips  .
.
 , which represents retained Surgicel (oxidized cellulose), placed to control continued oozing of blood. It may be impossible to distinguish this from an abscess without the proper history, and in such cases, needle aspiration may be required.
, which represents retained Surgicel (oxidized cellulose), placed to control continued oozing of blood. It may be impossible to distinguish this from an abscess without the proper history, and in such cases, needle aspiration may be required.
 in the perirenal space. This represents Surgicel, not an abscess. Note the surgical clip
in the perirenal space. This represents Surgicel, not an abscess. Note the surgical clip  at the site of resection.
at the site of resection.
 , surrounded by a large collection of fluid with an enhancing capsule
, surrounded by a large collection of fluid with an enhancing capsule  , typical for an abscess.
, typical for an abscess.
 within the right side of the abdomen.
within the right side of the abdomen.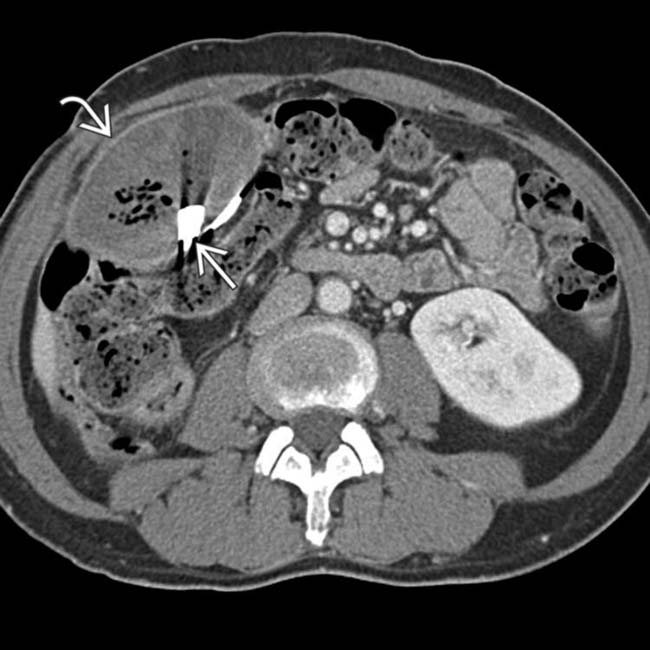
 within the right side of the abdomen. Immediately adjacent to the encapsulated fluid collection is a thin, radiopaque structure
within the right side of the abdomen. Immediately adjacent to the encapsulated fluid collection is a thin, radiopaque structure  that corresponds to the structure seen on the radiograph. This is a classic appearance of a gossypiboma, a retained surgical sponge that has resulted in a chronic abscess or foreign body reaction.
that corresponds to the structure seen on the radiograph. This is a classic appearance of a gossypiboma, a retained surgical sponge that has resulted in a chronic abscess or foreign body reaction.
 in the expected position of the rectum. Following retrieval under anesthesia, consideration should be given to perform a contrast enema to exclude foreign body perforation of the rectum, which is a fairly common occurrence in this setting.
in the expected position of the rectum. Following retrieval under anesthesia, consideration should be given to perform a contrast enema to exclude foreign body perforation of the rectum, which is a fairly common occurrence in this setting.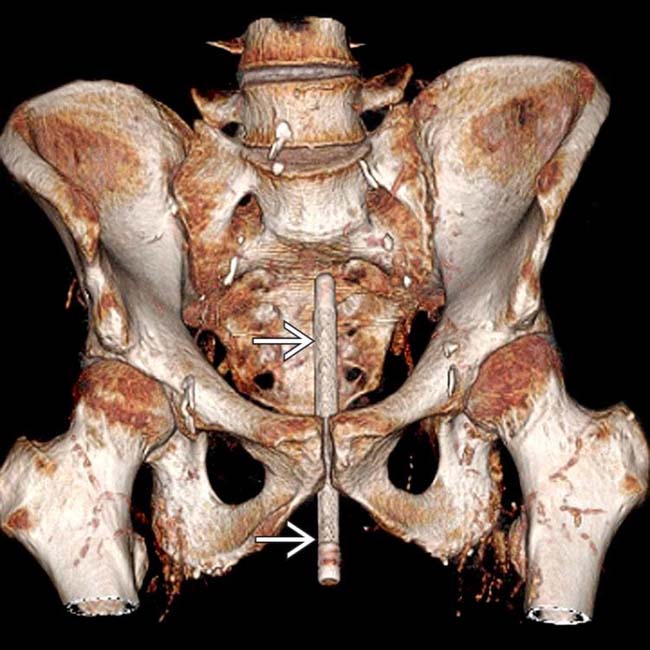
 , which turned out to be a penlight, relative to the bony structures of the pelvis. The object was retrieved in the cystoscopy suite.
, which turned out to be a penlight, relative to the bony structures of the pelvis. The object was retrieved in the cystoscopy suite.
 that is embedded within the wall of the stomach. This would not be evident on plain radiography due to its small size and minimal calcification. It is unusual for a fish bone to become embedded in the stomach; some penetrate the mucosa of the pyriform sinus, whereas most merely scratch the surface and do not become impaled.
that is embedded within the wall of the stomach. This would not be evident on plain radiography due to its small size and minimal calcification. It is unusual for a fish bone to become embedded in the stomach; some penetrate the mucosa of the pyriform sinus, whereas most merely scratch the surface and do not become impaled.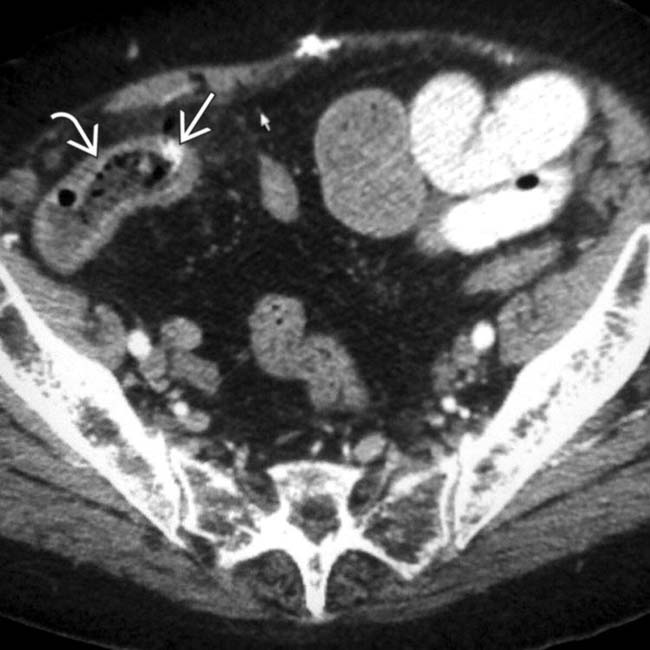
 with infiltration of the adjacent mesenteric fat. There is a thin calcific density
with infiltration of the adjacent mesenteric fat. There is a thin calcific density  within the wall of the bowel.
within the wall of the bowel.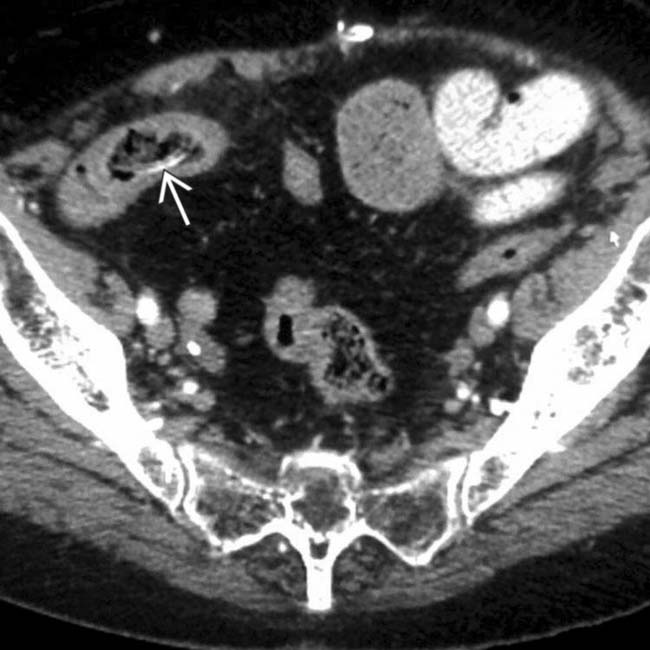
 . At surgery, a chicken bone was found to have perforated the distal ileum. Physiological points of narrowing, especially the distal ileum, are common sites of obstruction or perforation by ingested foreign bodies.
. At surgery, a chicken bone was found to have perforated the distal ileum. Physiological points of narrowing, especially the distal ileum, are common sites of obstruction or perforation by ingested foreign bodies.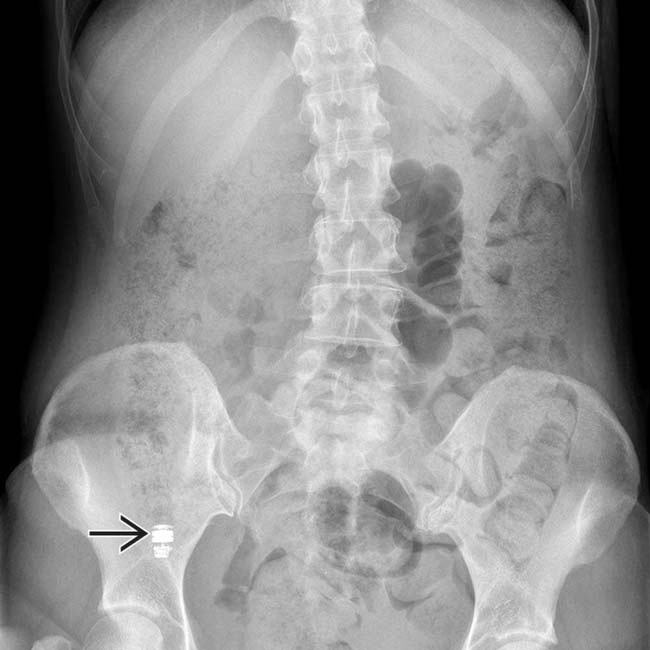
 in capsule endoscopy. This is an intentional foreign body, which should not be misinterpreted as an object of concern.
in capsule endoscopy. This is an intentional foreign body, which should not be misinterpreted as an object of concern.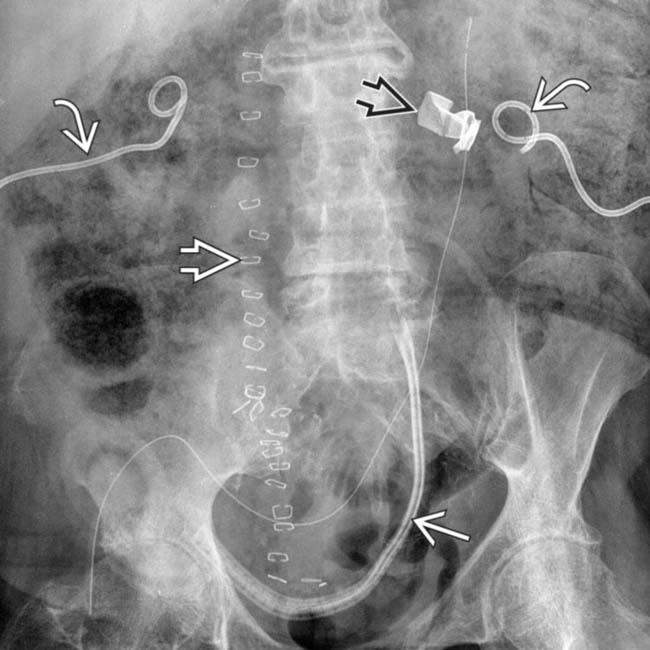
 , midline skin clips
, midline skin clips  , and surgical drains
, and surgical drains  . It might be easy to overlook the retained surgical sponge
. It might be easy to overlook the retained surgical sponge  that required opening the incision and retrieval.
that required opening the incision and retrieval.
 in the right lower quadrant near the ileocecal valve. There is extrinsic compression and wall thickening of the terminal ileum and colon. At surgery a toothpick was found to have perforated the terminal ileum.
in the right lower quadrant near the ileocecal valve. There is extrinsic compression and wall thickening of the terminal ileum and colon. At surgery a toothpick was found to have perforated the terminal ileum.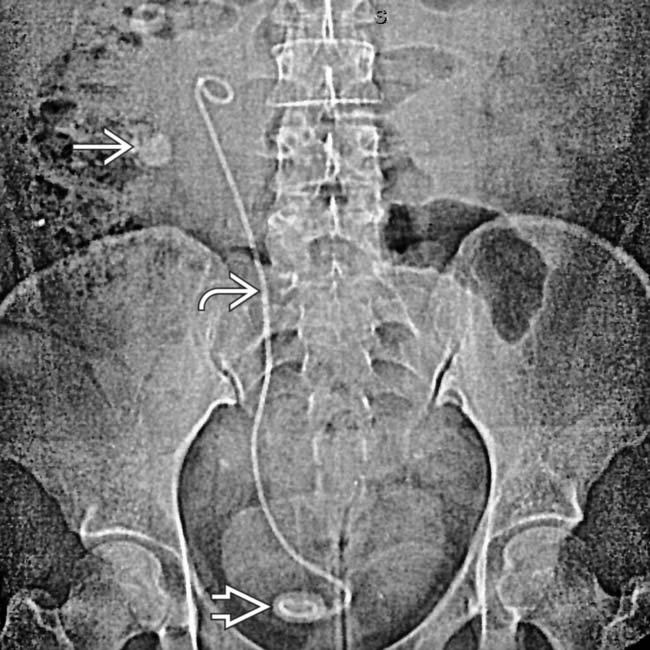
 and stones in the lower pole of the kidney
and stones in the lower pole of the kidney  and in the bladder around the distal part of the stent
and in the bladder around the distal part of the stent  .
.
 that has formed around the stent. Ureteral and biliary stents that remain in place for a long time invariably become encrusted with mineral salts, with luminal obstruction and formation of calculi within and around the stents.
that has formed around the stent. Ureteral and biliary stents that remain in place for a long time invariably become encrusted with mineral salts, with luminal obstruction and formation of calculi within and around the stents.
































































 within the prostate.
within the prostate.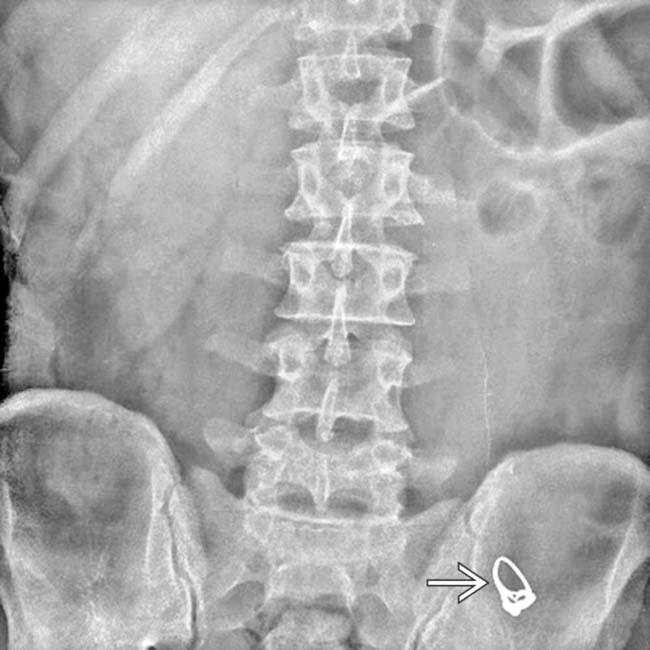
 in the lower abdomen that had been swallowed by the patient for unknown reasons. She subsequently developed acute abdominal pain.
in the lower abdomen that had been swallowed by the patient for unknown reasons. She subsequently developed acute abdominal pain.
 that represents a retained lap pad from the transplant procedure.
that represents a retained lap pad from the transplant procedure.


