Chapter 11 Forehead and Temple
RECONSTRUCTIVE PRINCIPLES
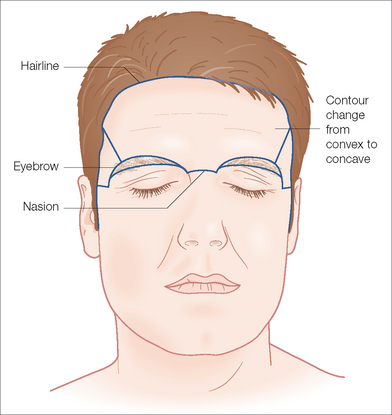
The forehead and temple constitute one-third of the face. This region includes the area from the natural frontal hairline superiorly and laterally, extending inferiorly to the zygomatic arch and curving above the superior aspect of the orbit to include the eyebrows and the nasal root. It is subdivided into five cosmetic units: central forehead, right and left lateral forehead (temple), and right and left eyebrow (Figure 11.1). There are several points to consider when evaluating this area including the inherent properties of the skin in the region, the underlying bone structure, the relaxed skin tension lines (RSTL) and wrinkles, the hair-bearing areas, the age of the patient, and the elastic properties of the surrounding tissue.
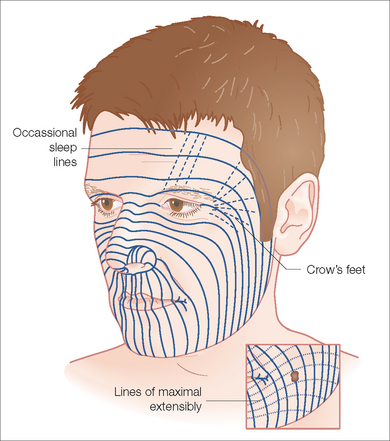
Adherence to the underlying frontalis musculature causes the thick skin of the central forehead to be relatively inelastic compared to the skin of the lateral forehead, which is more loosely attached to the underlying temporalis fascia, allowing comparatively easier manipulation. The underlying boney structure changes from convex centrally to concave laterally as seen in the surface anatomy. RSTL and natural wrinkles and furrows should be evaluated for potential hiding places for suture lines (Figure 11.2). The RSTLs are horizontal across most of the forehead, perpendicular to the underlying frontalis musculature, and curve in an inferior fashion laterally. The hair-bearing areas of the brows and the abutting scalp can help with camouflaging scar lines but can also limit flap design. In the younger patient, the skin is more elastic and the collagen thicker than in the older patient. The relative increased skin elasticity and regularity will cause greater wound expansion after excision of a lesion, leading to a longer suture line. At times after undermining a lesion, the elastic properties of the skin will declare the direction of least tension to close the wound, which can be different from the forces on the wound before undermining. Using your fingers or skin hooks to approximate the edges of an undermined defect will help determine the direction of closure, which avoids tension.
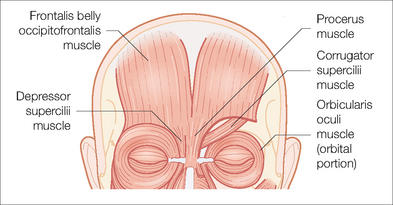
The frontalis, corrugator, and the superior aspect of the orbicularis oculi muscles make up the underlying musculature of the forehead (Figure 11.3). The frontalis muscle, lying just below the subcutaneous tissue, is a vertically oriented muscle that is continuous with the galea aponeurotica superiorly and interdigitates with the procerus, orbicularis oculi, corrugator supercilii, depressor supercilii, and skin of the eyebrow inferiorly. Frontalis contraction causes brow elevation and is responsible for cutaneous horizontal creases. The temporal branch of the facial nerve is responsible for the action of the frontalis with denervation resulting in unilateral brow ptosis and loss of forehead motion. The width of this muscle can be easily palpated and often noted clinically by the extent of the forehead crease. The corrugator supercilii muscle is a paired muscle originating at the medial end of the superciliary arch and inserting into the frontalis and skin of the brow. It acts via the temporal nerve to pull the brow together and downward, causing vertical glabellar frown lines. These muscles are often the target of botulinum toxin injections to ameliorate the rhytids between the eyebrows. The orbicularis oculi lies beneath the eyebrow. Its action assists in closure of the eye through temporal nerve innervation. The superficial musculoaponeurotic system (SMAS) envelops the frontalis muscle and then forms the galea aponeurotica.
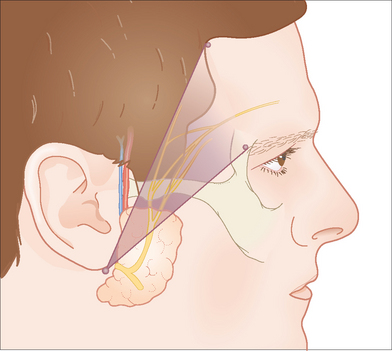
The temporal branch of the facial nerve runs with the SMAS in the temple roughly along a line drawn 0.5 cm below the tragus to a point about 1.5 to 2.0 cm above the outer margin of the orbit where the branches enter the muscle from its deep aspect (Figure 11.4). This nerve is particularly vulnerable over the zygoma where it lies quite superficially just beneath the subcutaneous fat. Upon reaching the frontalis muscle, the temporal nerve courses along its undersurface with smaller nerve branches coursing more superficially.1,2 One should undermine in the superficial aspect of the subcutaneous plane with particular care over the zygoma when closing defects located in the region of the lateral forehead. When undermining around defects located on the central forehead and brow area, the ideal plane of dissection lies just superficial to the SMAS, covering the regional muscles if the defect is no deeper than the subcutaneous tissue. However, defects that violate the frontalis muscle require repair of the muscle and undermining in the avascular plane beneath the muscle overlying the periosteum.3
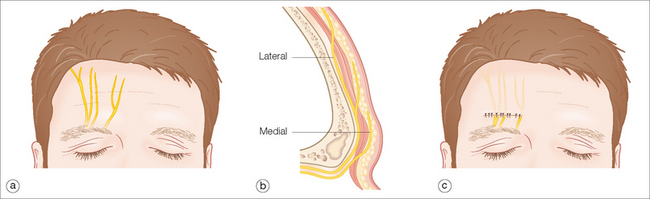
Sensory innervation of the central forehead originates from branches of the supraorbital and supratrochlear nerves. The pattern of division of these nerves into four or five branches is variable and often asymmetric: however, a common feature is the plane in which these nerves travel with respect to their location. These nerves exit their foramen centrally and quickly penetrate the musculature before continuing in the superficial subcutaneous plane. As one progresses laterally, these nerves course along the underside of the frontalis muscle before changing planes to the superficial subcutaneous plane.4 Consequently, horizontal closure on the central forehead will produce a temporary fan-shaped area of numbness superior to the closure (Figure 11.5). Patients should be made aware of this prior to any surgical incision in this area.
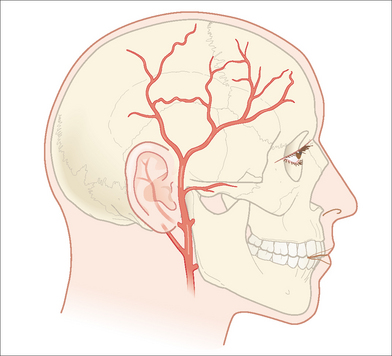
Blood supply to this region is provided by both the internal and external carotid systems. The internal carotid artery supplies the eyelids, upper nose and nasal dorsum, the forehead, and the scalp through its ophthalmic arterial branch. The ophthalmic artery branches into the supraorbital and supratrochlear arteries, which exit the skull with their corresponding nerves and veins through the supraorbital and supratrochlear foramen, respectively. Upon exiting the skull these arteries perforate the frontalis muscle and run in the subcutaneous tissue. The supraorbital foramen can be located clinically by palpation of the bony supraorbital ridge at the vertical mid-pupillary line. The supratrochlear artery courses medial to the supraorbital artery. This artery serves as the axial blood supply for the midline forehead flap. The external carotid artery branches from the common carotid and is the principal artery that supplies blood to the face. The superficial temporal artery is the terminal branch of the external carotid artery. It runs within and then above the SMAS layer of the lateral forehead. Just above the uppermost-attached portion of the ear, the artery branches into the parietal and frontal (anterior) branches (Figure 11.6). The forehead, brow, and scalp receive their arterial supply through these branches of the superficial temporal artery.1
As with defects in any location, it is best to systematically consider the reconstruction options: second intention healing, primary closure, random tissue flaps, pedicle flaps, full- and split-thickness skin graft, and Burow’s graft. Within this framework, the size, depth, and location of the defect and the patient’s anatomy will dictate which reconstructive option is best.5
Second intention healing is a method of wound management that can provide excellent cosmetic results in certain areas.6 Wounds on concave surfaces, such as the lateral forehead, heal with a better cosmetic result than wounds located on convex surfaces, such as the central forehead.7 The frontal bossing of the central forehead lends itself to healing with step-off or contour irregularities and stellate or hypertrophic scars. On the lateral forehead, wounds healing by second intention contract and result in flat or slightly depressed hypopigmented scars. In this area, hypertrophic scarring is rare and distortion of the brow, lateral canthus, and hairline is unusual even with large wounds.8 When needed, guiding sutures may be placed to direct the contraction of the scar to optimize cosmetic results or to change the vectors of the contracting scar away from or toward another anatomic region.9 Advantages of second intention healing include the low risks of hematoma formation or infection if proper care is administered. The likelihood of nerve damage or facial distortion associated with wound edge undermining and wound closure is reduced greatly.
Cosmetic factors to consider when selecting a patient for second intention healing include skin color, surrounding photo-damage, and the patient’s age. Since the scar will most likely be hypopigmented, darker skinned individuals or those with the surrounding dyschromia of photoaging will have a scar less likely to match their skin. Younger patients tend to have a better skin match after secondary intention healing than older patients, who frequently have ruddy complexions with telangiectasia, lentigines, and other colored growths that would contrast the white color of the healed site (Figure 11.7). The depth of the wound is another determining factor in choosing between first and second intention reconstruction. Shallow wounds are more likely to blend into the surrounding skin with smooth borders and will heal more quickly than full-thickness defects in the same location. Surprisingly, deep wounds with exposed bone at the base have been shown to heal safely and effectively by second intention.10 If bone is exposed, sanding the outer table of frontal bone or cranium will promote faster healing and granulation tissue formation.11 For larger defects on the upper forehead or scalp of balding men, a random tissue flap to cover the defect with exposed bone and back-grafting over the secondary defect can provide excellent coverage and cosmesis.12

Figure 11.7 White discoloration of skin grafts and second intention healing can be very unsightly on the forehead.
The kinetics of second intention healing are important when educating the patient on wound care and predicting the time needed for healing. If a partial-thickness wound exists, reepithelialization of the wound is needed for healing. Adnexal structures provide this reepithelialization. It is important to remember that the healing time needed for reepithelialization of a wound is not only proportional to the size of the wound, but also to the density of adnexal structures plentiful on the face. Preexisting scars and prior radiation therapy will decrease the number of adnexal structures and slow reepithelialization.
The healing of full-thickness wounds is also influenced by a number of other factors including the size and location of the wound, the method of wounding, and the presence of wound contaminants. During the first period of healing, the lag phase, there is little to no change in the size of the wound, and it can actually enlarge slightly because of the elasticity of the surrounding skin. Later, during the exponential phase, healing occurs at a more constant rate. The healing time for full-thickness wounds is not directly proportional to the size of the wound; rather it has a logarithmic relationship to the surface area of the wound. Therefore larger wounds take only slightly longer to heal than smaller wounds. Identical wounds made on the face and leg will heal at different rates. Wounds in acral locations take longer to heal because of a variety of factors including venous dependency, a decreased number of blood vessels, and fewer adnexal structures. The rate of wound closure is independent of wound shape. The relationship of healing time to shape is best described as being dependent on the diameter of the largest circle that can be contained within the wound margins.13
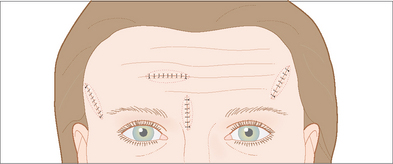
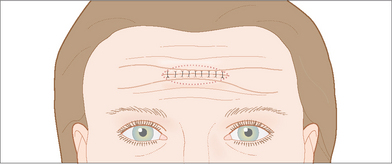
Horizontal and vertical primary closures are the mainstays of reconstruction on the forehead. Vertical closures are especially well suited in the glabella and central forehead where they can be hidden. Similarly horizontal closures can be camouflaged by the RSTL that run across the forehead superior to the eyebrow (Figure 11.8). The radial orientation of closures on the lateral forehead and temple will utilize the greatest amount of tissue movement as well as follow the RSTL of the crow’s feet (Figure 11.9). In order to determine the best direction of closure in these areas, skin hooks can be used to approximate the skin edges in different directions.
Vertical closures place the tension vector in a horizontal direction and will prevent brow distortion. Vertical closures also offer several other advantages on the forehead. Vertical closures avoid the typical V-shaped areas of temporary numbness that extend superiorly above horizontally oriented forehead closures. A vertically oriented approximation of skin edges also avoids distortion or pinching together of horizontal RSTL possibly occurring with horizontal closure (Figure 11.10). Care must be taken to reapproximate the horizontal RSTL on each side of the vertical closure. This advantage must be weighed against the possibility of a white vertical scar line that can be visibly prominent on the forehead of patients with a ruddy complexion (Figure 11.11). A vertical white scar even with perfectly smooth contours is often more noticeable than a horizontal scar line hidden within a RSTL (Table 11.1).
| VERTICAL CLOSURE |
|---|
| HORIZONTAL CLOSURE |
|---|
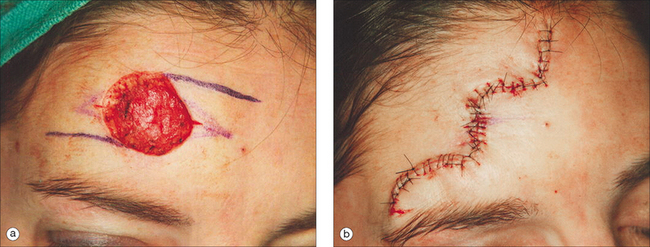
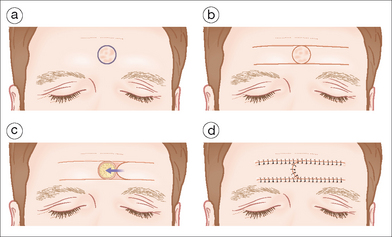
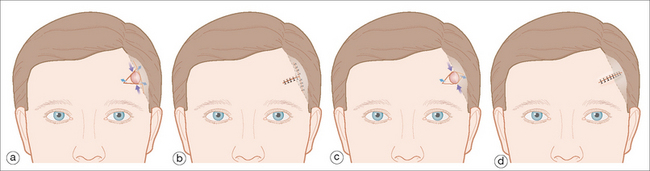
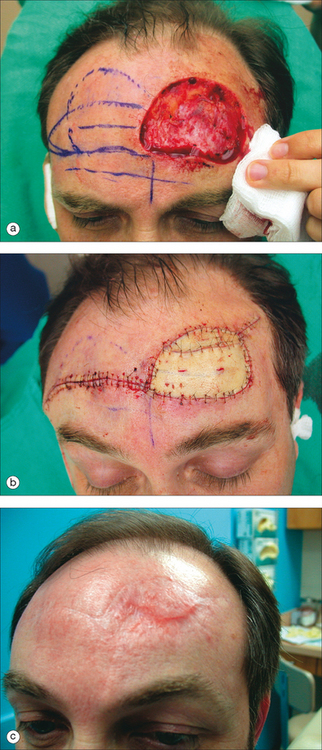
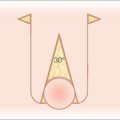
At times, the size of the wound and the subsequent need to redirect tension vectors requires the use of a random tissue flap. Classically the H-flap, bilateral advancement flap, has been utilized on the forehead.14 The limbs of this flap are designed to fall within horizontal RSTL, and the vertical component is aligned in the middle of the defect. The length of the flap should be limited to three to four times the width, and the tension on the vertical aspect of the flap should be minimized so that vascular compromise does not produce tissue necrosis. The use of horizontal tension vectors with the H-flap avoids lifting the brow. Also because the tissue is advanced as a unit horizontally, a distortion or pinching of the RSTL does not occur. Since the deeper planes of tissue are fixed at the lateral aspect of the forehead, extending the flap or widening the zone of undermined tissue will not significantly increase the amount of laxity available for closure. Advancement flaps on the forehead displace the redundant tissue and allow placement of the majority of the wound in a horizontal fashion along the well-hidden RSTL. Often a single advancement flap designed along horizontal brow lines will provide enough tissue movement for closure of the defect and eliminate one-half of the required incisions. Similarly, an O-to-Z flap can be designed to provide bilateral horizontal tissue recruitment with half as much linear scar length as the classical H-flap.15 This tissue movement is more accurately considered a bilateral rotation flap than a bilateral advancement flap (Figure 11.12). Harahap described a modified version of the bilateral advancement flap.16 A 30° wedge of tissue is removed from the distal end of one advancement flap. The resulting elliptical wound is sutured together and advanced as a single unit. This better matches the shape of the flap to the shape of the defect (Figure 11.13) (Table 11.2).
TABLE 11.2 BILATERAL ADVANCEMENT FLAP VERSUS BILATERAL ROTATION FLAP
| BILATERAL ADVANCEMENT FLAP |
|---|
| BILATERAL ROTATION FLAP |
|---|
For defects adjacent to the hair-bearing areas of the scalp a bilateral advancement flap, O-to-T or V-to-T flap, can be designed so that the top of the T runs along the abutment of the scalp to the forehead.16 The standing tissue cones produced by the closure can then be excised into the hairline. An alternative to this closure is a primary advancement closure designed so that half of the scar extends into the hairline (Figure 11.14). With either the A-to-T or primary advancement closure, a line scar extending onto the forehead will be present. Advantages of the primary closure are a shorter overall scar line and a more simple surgery requiring less undermining. This is particularly useful over the areas where the temporal artery and nerve course (Table 11.3).
TABLE 11.3 PRIMARY CLOSURE VERSUS A-TO-T CLOSURE
| PRIMARY CLOSURE |
|---|
| A-TO-T CLOSURE |
|---|
Other flaps utilized in forehead and temple reconstruction include transposition and single rotation flaps.18–20 Transposition (single or double) and single rotation flaps are best used in the superior lateral forehead area on defects of all sizes, but are especially useful in recruitment of tissue for large defects. Both types of flaps have a broad base and good blood supply. Transposition and rotation flaps can recruit the lax skin of the cheek and neck for repair of larger defects of the lateral forehead (Figure 11.15). Cervical-cheek rotation flaps should be designed so that the incisions are hidden in the preauricular area or the hairline, without distorting the natural hairline or moving hair onto the forehead. When a large defect is present, undermining in the superficial subcutaneous plane of the cheek and neck avoids potential nerve damage. When removing the tissue redundancy created by rotation of these flaps, it is important to avoid back-cutting into the base of the flap and compromising the blood supply of the flap.
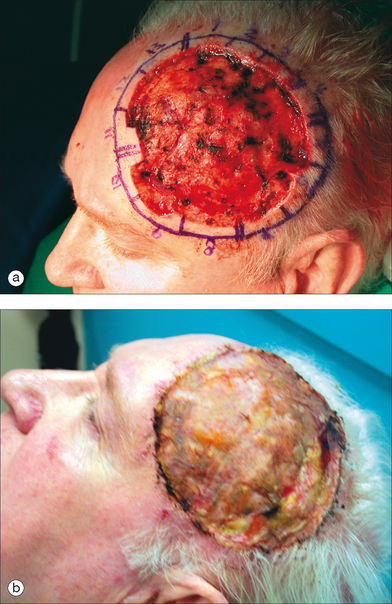
At times defects are too large for primary closures or random tissue flaps, and a split- or full-thickness graft is needed for closure (Table 11.4). A full-thickness skin graft includes full-thickness epidermis and dermis, whereas a split-thickness skin graft includes the entire epidermis but only a portion of the papillary or reticular dermis. Both types of grafts allow wound healing to occur at a more rapid rate than by second intention healing alone and reduce the contraction that can occur by second intention mechanisms. Because the donor area for split-thickness skin graft heals by second intention healing, a large amount of tissue can be taken from one site without the need for closure of this donor site, which is, therefore, the major advantage to split-thickness skin grafts. Another advantage in poorly vascularized defects such as those extending to periosteum or exposed bone is a higher success rate of the split-thickness grafts over their full-thickness counterparts because of lower nutritional requirements.21–23 The color, texture, and contour match to the surrounding skin are not as good with a split-thickness graft as with a full-thickness graft: however, these grafts do provide coverage for very large defects (Figure 11.16). The step-off deformity occurring when utilizing grafts can be minimized by beveling the edge of the defect before graft placement or waiting a period of time before placement of the graft so that granulation tissue on the base of the wound appears.24,25
| SPLIT-THICKNESS SKIN GRAFTS (STSG) |
|---|
| FULL-THICKNESS SKIN GRAFTS (FTSG) |
|---|
| BUROW’S |
|---|
Full-thickness skin grafts (FTSG) offer the advantages of a better match for skin texture, color, and thickness as well as reducing wound contraction when compared to STSG. When choosing a donor site, a relatively non-actinically damaged area should be chosen with similar thickness and color as the area to be repaired. The most commonly used donor sites for the forehead and temple area are the skin of the clavicle, retroauricular area, neck, or adjacent forehead skin. Utilizing adjacent skin for a FTSG (aka Burow’s or regional graft) provides an excellent skin match with regard to color and texture (Figure 11.17).26–28 Furthermore closure of this donor site effectively reduces the size of the defect. The donor site closures can be hidden in RSTL on the forehead or in the hairline of the temple and eliminate the need for a second surgical site to provide donor tissue (Figure 11.18).
Successful reconstruction of the eyebrow clearly restores a cosmetically critical hair-bearing area of the face. Several methods of repair can be used to preserve this cosmetic unit, depending on the size and location of the defect. Second intention healing is a viable option only for the most superficial of defects extending no deeper than the papillary dermis. Full-thickness defects must be repaired with first intention closure to prevent scarring patches of alopecia. Vertically oriented primary closures can be designed to restore the hair-bearing areas of the brow for defects that sacrifice an entire segment of the eyebrow. Incisions should be made at a slight angle to match the angle of the hair and minimize scar line alopecia. A small defect that only partially involves the brow or lies adjacent to the brow can be repaired in a horizontal linear fashion. With this technique, the edge of the brow camouflages the scar. As with the forehead, defects of the brow, which are too large to be closed with a primary closure, can often be repaired with a bilateral advancement flap or an O-to-T flap.29 Again, the vertical component of each flap is oriented perpendicular to the horizontally positioned eyebrow. If reconstruction of the eyebrow does not preserve the hair bulbs, hair transplantation can be done.30 Transplanting hair from the nape of the neck often provides a good cosmetic outcome on the eyebrow because hair has a shorter growth phase and therefore shorter length than that taken from the scalp. Care is taken to direct the transplanted hairs more vertical in the medial edge of the brow and more horizontal in the remainder of the brow.
COMPLICATIONS
The most common complications unique to the forehead and temple involve damage to the temporal branch of the facial nerve and the superficial temporal artery. Statistically, bleeding and hematoma formation are the most frequent complications of office-based surgeries.31 Surgery on the upper lateral forehead frequently disrupts the tortuous bifurcation of the superficial temporal artery, which lies in the subcutaneous tissue. The branches of this artery can be avoided by palpating the pulse of these vessels and tracing over them with a surgical marker. When possible, these vessels should be dissected and identified then ligated with a figure of eight stitch before severing. Ligating larger vessels rather than merely using electrocoagulation will help maintain a more bloodless surgical field and reduce the risks for postoperative hematoma formation.
Within the glabella, the supratrochlear and superior orbital arteries exit the frontal bone through their respective foramens in the superior orbital rim. Because of the potential usefulness of these arteries as blood supply for paramedian forehead flaps, they should be left in tack when possible. Traveling with these arteries, the supratrochlear and supraorbital nerves provide sensory innervation of the forehead. Any injury or transection of these nerves as they course superiorly over the frontalis muscles will produce a V-shaped area of numbness above the point of insult. Over a 6- to 12-month period following surgery, new sensory innervation is generally established.32 During this time of reinnervation, a prickling or burning sensation is frequently experienced intermittently by patients (Table 11.5).
| TEMPORAL NERVE DAMAGE |
A more significant deficit is produced when forehead surgery results in a loss of motor nerve innervation. The temporal nerve is particularly susceptible to injury as it crosses the zygoma and courses through the temple area to innervate the ipsilateral portion of the frontalis muscle. Temporal nerve damage is seen as an inability to raise the forehead on the side of the injury. During and immediately following surgery, loss of muscular function is frequently seen as a result of local anesthetic infiltration and postoperative edema. These temporary deficits usually resolve by the time the patient returns for suture removal. This loss of movement can also be caused by bruising, retraction during surgery, or inadvertently suturing the nerve, thus producing a deficit that may persist for several months before resolving.33 Transection of the temporal nerve produces a permanent loss of muscular movement that usually produces a ptotic brow on the affected side. This drooping brow can be corrected by a unilateral brow lift-restoring symmetry of the forehead (Figure 11.19). In younger patients, nerve grafts can sometimes repair the lost function and symmetry of the forehead. Most surgeons prefer to wait 12 months after surgery so that other more temporary forms of nerve injury are given enough time to resolve before proceeding with a corrective procedure.
1 Clemente CD. Anatomy, a regional atlas of the human body, 4th edn. Philadelphia: Lippincott Williams &Wilkins, 1997.
2 Larrabee WFJr, Makielski KH, Henderson JL. Surgical anatomy of the face, 2nd edn. Philadelphia: Lippincott Williams &Wilkins, 2003.
3 Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology, 1st edn., London: Mosby, 2003.
4 Fatah MF. Innervation and functional reconstruction of the forehead. Br J Plast Surg. 1991;44:351-358.
5 Johnson TM, Swanson N, Baker SR. Concepts of sliding and lifting tissue movement in flap reconstruction. Dermatol Surg. 2000;26:274-278.
6 Goldwyn RM, Rueckert F. The value of healing by secondary intention for sizeable defects of the face. Arch Surg. 1977;112:285-292.
7 Mott KJ, Clark DP, Stelljes LS. Regional variation in wound contraction of Mohs surgery defects allowed to heal by second intention. Dermatol Surg. 2003;29:712-722.
8 Zitelli JA. Wound healing by secondary intention, a cosmetic appraisal. JAAD. 1983;9:407-415.
9 Albright SD3rd. Placement of “guiding sutures” to counteract undesirable retraction of tissues in and around functionally and cosmetically important structures. J Dermatol Surg Oncol. 1981;7:446-449.
10 Becker GD, Adams LA, Levin BC. Secondary intention healing of exposed scalp and forehead bone after Mohs surgery. Otolaryngology Head Neck Surg. 1999;121:751-754.
11 Schaefer SD, Byrd HS, Holmes RE. Forehead and scalp reconstruction after wide-field resection of skin carcinoma. Arch Otolaryngol. 1980;106:680-684.
12 TerKonda RP, Sykes JM. Concepts in scalp and forehead reconstruction. Otolaryngol Clin North Am. 1997;30:519-539.
13 Roenigk RK, Roenigk HH. Dermatologic surgery, principles and practice, 2nd edn. New York: Marcel Dekker, 1996.
14 Rose V, Overstall S, Moloney DM, Powell BW. The H-flap: a useful flap for forehead reconstruction. Br J Plast Surg. 2001;54:705-707.
15 LeVasseur JG, Mellette JR. Applications of the double O to Z flap repair for facial reconstruction. Dermatol Surg. 2001;27:79-81.
16 Harahap M. The modified bilateral advancement flap. Dermatol Surg. 2001;27:463-466.
17 Field LM. The forehead V-to-T plasty (Dieffenbach’s winged V-plasty). J Dermatol Surg Oncol. 1986;12:560-562.
18 Johnson TM, Wang TS, Fader DJ. The birhombic transposition flap for soft tissue reconstruction. J Am Acad Dermatol. 1999;41:232-236.
19 Grigg R. Forehead and temple reconstruction. Otolaryngol Clin North Am. 2001;34:583-600.
20 Sutton AE, Quatela VC. Bilobed flap reconstruction of the temporal forehead. Arch Otolaryngol Head Neck Surg. 1992;118:978-982.
21 Muller W. [Split skin and full-thickness skin grafts.]. Mund Kiefer Gesichtschir. 2000;4:S314-S321.
22 Vindenes H. [Skin transplantation.]. Tidsskr Nor Laegeforen. 1999;119:4050-4053.
23 Small RG, Sahl WJ. The use of split-thickness skin grafts for eyelid and facial reconstruction after Mohs’ fresh-tissue surgery. Ophthal Plast Reconstr Surg. 1989;5:266-270.
24 Schmid MH, Meuli-Simmen C, Hafner J. Repair of cutaneous defects after skin cancer surgery. Recent Results Cancer Res. 2002;160:225-233.
25 Bumsted RM, Panje WR, Ceilley RI. Delayed skin grafting in facial reconstruction. When to use and how to do. Arch Otolaryngol. 1983;109:178-184.
26 Zitelli JA. Burow’s grafts. J Am Acad Dermatol. 1987;17:271-279.
27 Krishnan R, Hwang L, Orengo I. Dog-ear graft technique. Dermatol Surg. 2001;27:312-314.
28 Zivony D, Siegle RJ. Burow’s wedge advancement flaps for reconstruction of adjacent surgical defects. Dermatol Surg. 2002;28:1162-1164.
29 Harris GJ, Garcia GH. Advancement flaps for large defects of the eyebrow, glabella, forehead, and temple. Ophthal Plast Reconstr Surg. 2002;18:138-145.
30 Motomura H, Muraoka M, Nose K. Eyebrow reconstruction with intermediate hair from the hairline of the forehead on the pedicled temporoparietal fascial flap. Ann Plast Surg. 2003;51:314-318.
31 Cook JL, Perone JB. A prospective evaluation of the incidence of complications associated with Mohs micrographic surgery. Arch Dermatol. 2003;139:143-152.
32 Lutz ME, Otley CC, Roenigk RK, Brodland DG, Li H. Reinnervation of flaps and grafts of the face. Arch Dermatol. 1998;134:1271-1274.
33 Flynn TC, Emmanouil P, Limmer B. Unilateral transient forehead paralysis following injury to the temporal branch of the facial nerve. Int J Dermatol. 1999;38:474-477.