FOREARM, WRIST, AND HAND

SPECIAL TESTS FOR LIGAMENT, CAPSULE, AND JONT INSTABILITY2–5
Relevant Special Tests
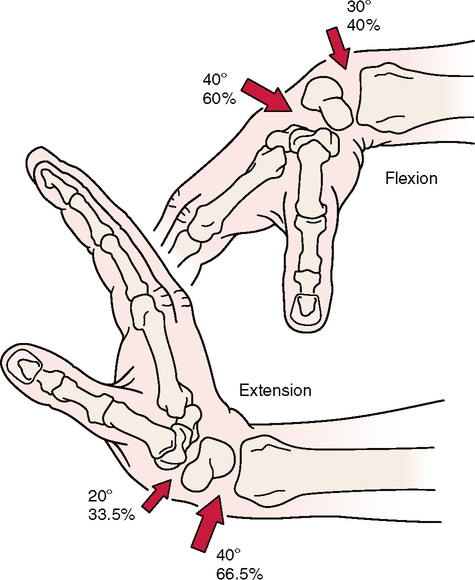
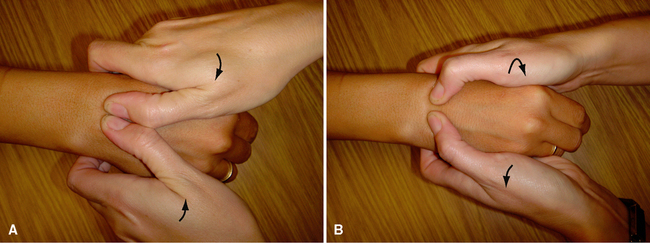
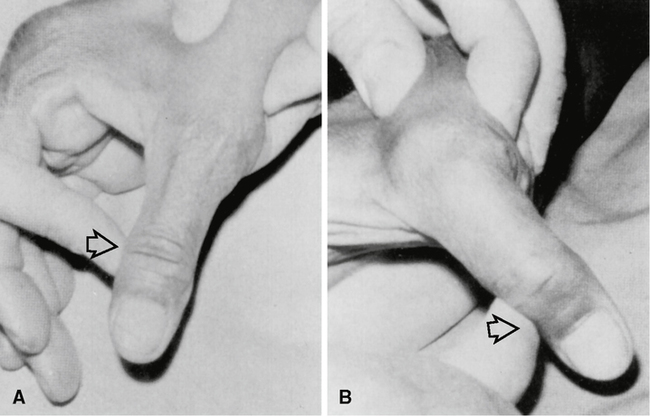
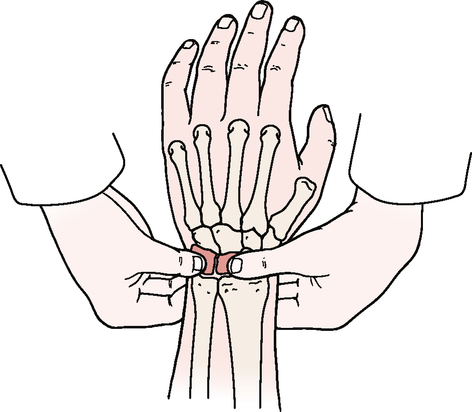
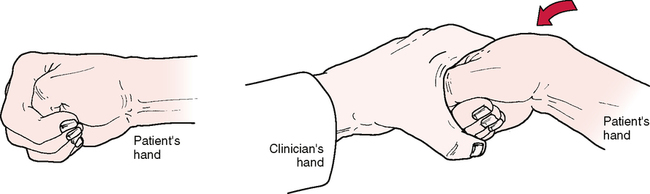
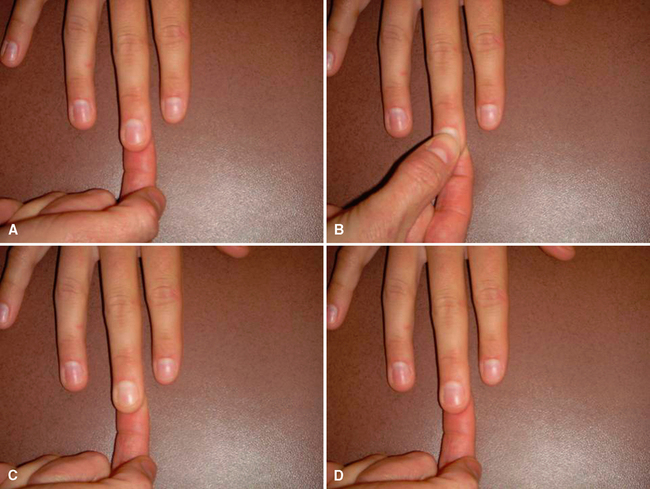
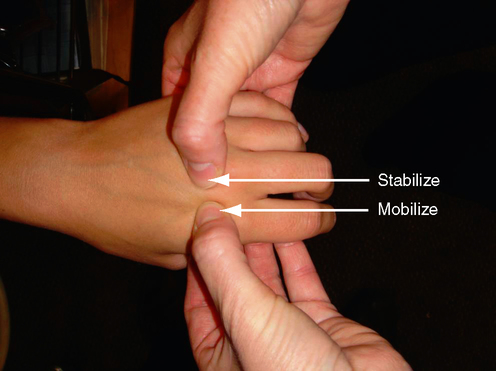
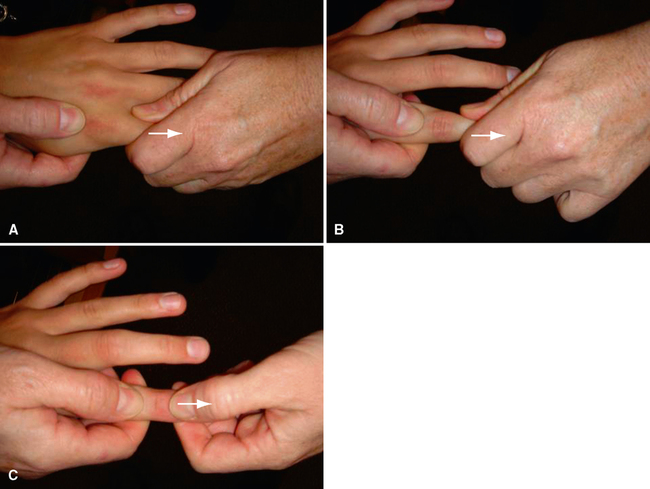
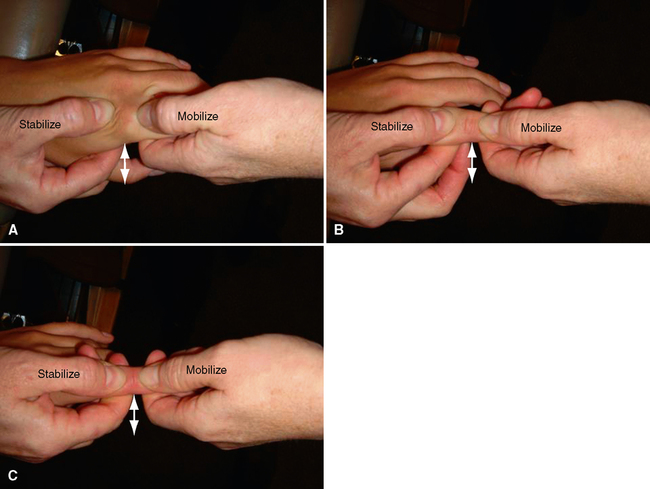
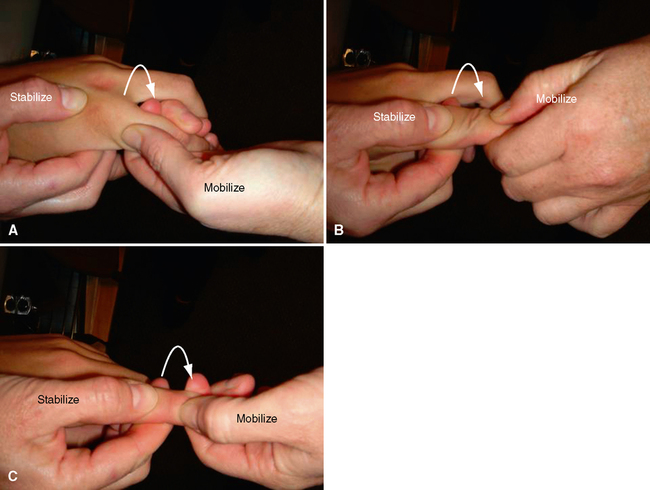
Ligamentous instability test for the fingers
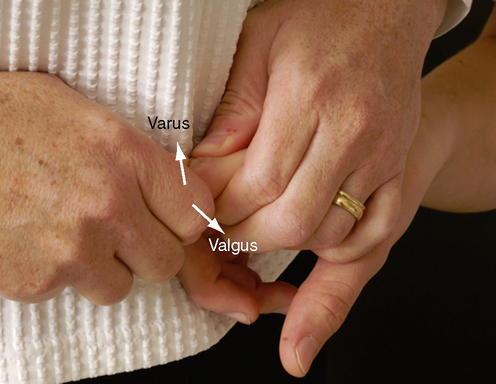
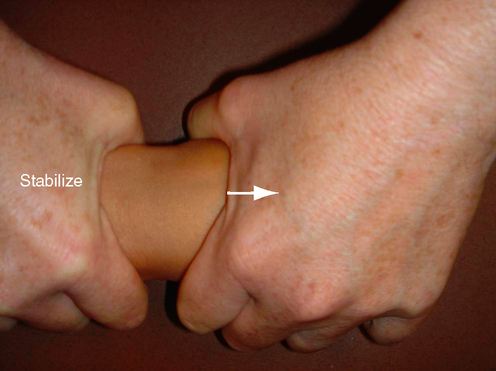
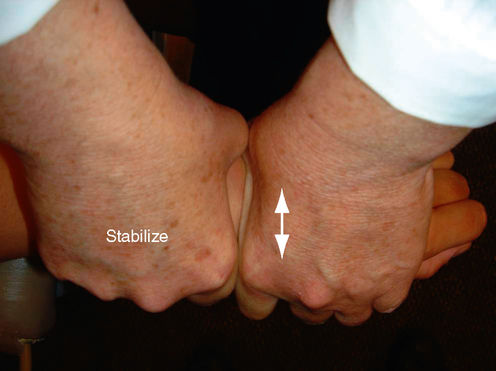
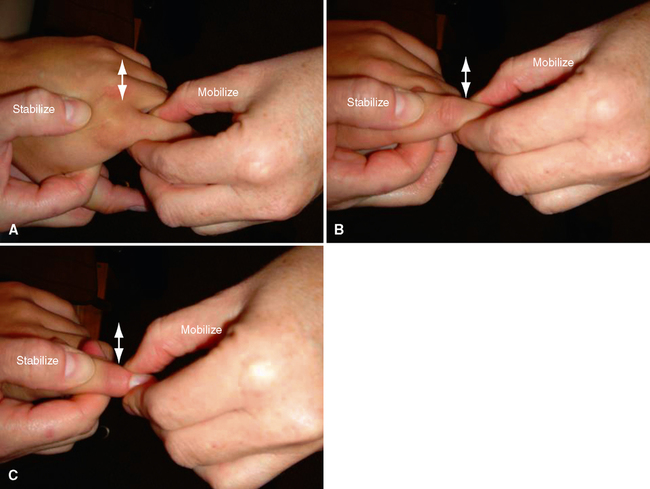
Thumb ulnar collateral ligament laxity or instability test
Suspected Injury
Relevant Signs and Symptoms
• Localized pain may occur over the injured tissue, especially when the individual is gripping, using the hand, or weight bearing on the hand.
• Generalized pain may be present.
• Swelling may or may not be present.
• Clicking or catching may be noted with functional use.
• The patient may complain of weakness in the hand and wrist.
SPECIAL TEST FOR MUSCLE OR TENDON PATHOLOGY17–19
Relevant Special Test
Relevant History
• Recurrent episodes are common.
• Work requiring repetitive wrist motion often is cited as a factor.
• The condition may appear in women after giving birth, probably because of altered hand use in lifting the infant and positioning the baby for breast-feeding. Research also has demonstrated laxity in the wrist joint postpartum, which may contribute to the development of pain in the region.
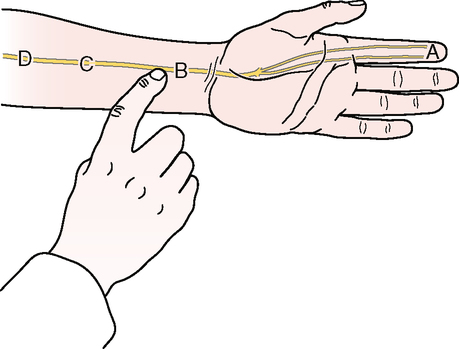
SPECIAL TESTS FOR NEUROLOGICAL SYMPTOMS22–32
Relevant Special Tests
Mechanism of Injury
• First-degree neuropraxia involves distortion of myelin about the nodes of Ranvier caused by ischemia, mechanical compression, or electrolyte imbalance, resulting in temporary loss of nerve conduction.
• Second-degree axonotmesis involves interruption of the axon with secondary wallerian degeneration but preservation of the supporting tissue around the axon. Recovery may be complete but takes longer and depends on the distance between the site of injury and the end structure (denervated muscle).
• Third-degree neurotmesis involves extensive disruption of the nerve and its supporting structures; however, although the endoneurium is disrupted, the perineurium and epineurium remain intact.
• Fourth-degree neurotmesis involves disruption of all neural components except the epineurium.
• Fifth-degree neurotmesis involves complete transection and discontinuity of the nerve, with no capacity for regeneration. Neurotmesis rarely occurs as a result of entrapment. However, when continuity has been disrupted, complete recovery is not possible, even with surgical techniques, and the eventual outcome depends on the individual circumstances.
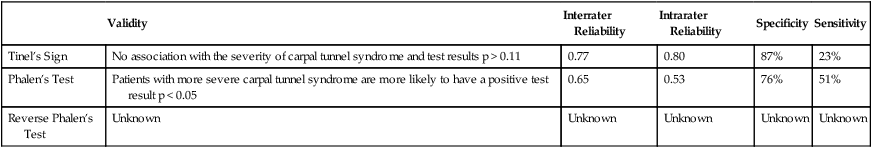
RELIABILITY/SPECIFICITY/SENSITIVITY COMPARISON30–32
| Validity | Interrater Reliability | Intrarater Reliability | Specificity | Sensitivity | |
| Tinel’s Sign | No association with the severity of carpal tunnel syndrome and test results p > 0.11 | 0.77 | 0.80 | 87% | 23% |
| Phalen’s Test | Patients with more severe carpal tunnel syndrome are more likely to have a positive test result p < 0.05 | 0.65 | 0.53 | 76% | 51% |
| Reverse Phalen’s Test | Unknown | Unknown | Unknown | Unknown | Unknown |
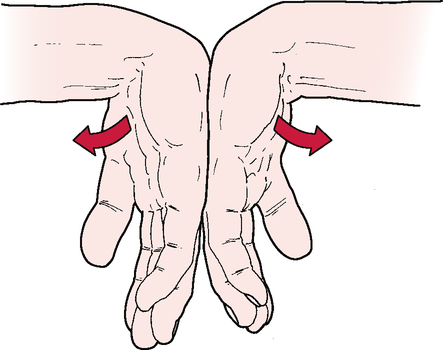
SPECIAL TESTS FOR CIRCULATION AND SWELLING IN THE WRIST AND HAND
Relevant Special Tests
Relevant Signs and Symptoms
• Swelling is more obvious on the dorsum of the hand, where the skin is looser.
• Tightness and stiffness in the hand joints often are seen.
• Rings and jewelry on the hands and fingers may fit tightly.
• Coldness or weakness in the hands and arms may be noted.
• Color changes may be seen in the upper extremity.