Foot and Ankle
Joseph S. Park, Venkat Perumal
Foot and Ankle
General Guidelines
Preoperative antibiotics are given half an hour before the incision is made
A tourniquet is applied according to the surgeon’s preference
An Esmarch bandage or pneumatic tourniquet may be used
All bony prominences should be adequately padded
Review the pertinent anatomy and mark the palpable landmarks
Regional Anatomy
Osteology
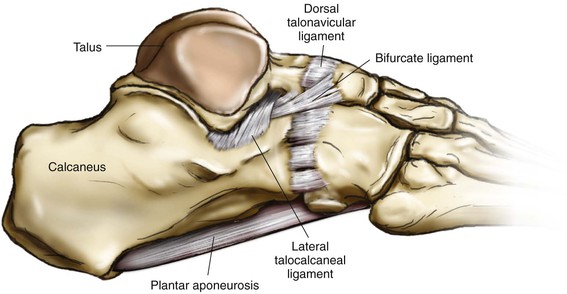
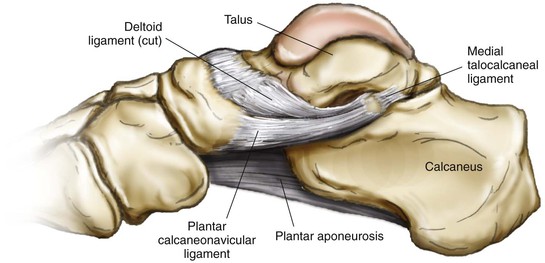
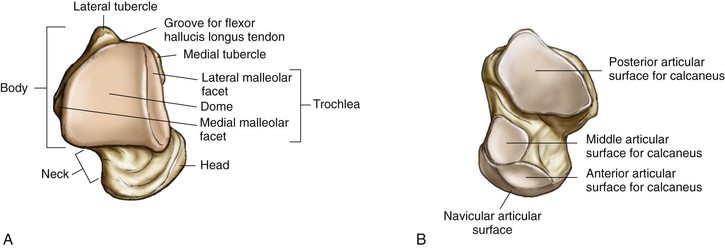
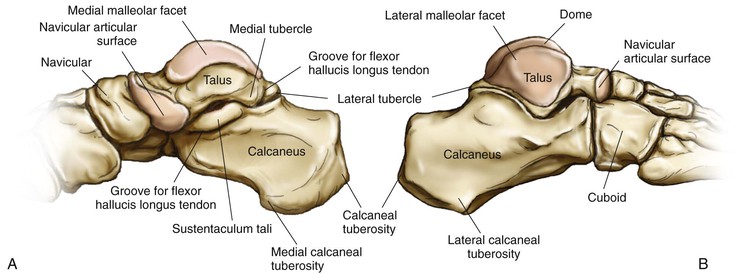
Talus (Fig. 8-1)
Three parts: body, neck, and head
No muscles or tendons are attached
The superior surface is a dome with a large articular facet
The lateral surface has a triangular lateral malleolar facet
The inferior surface has a large concave posterior facet for the calcaneus
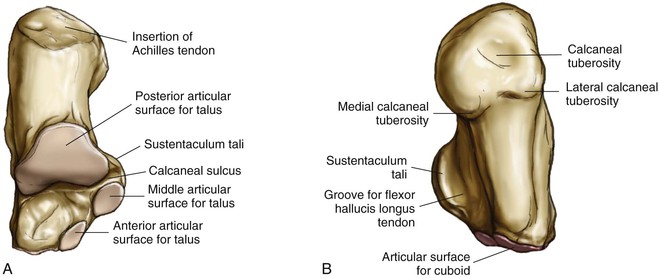
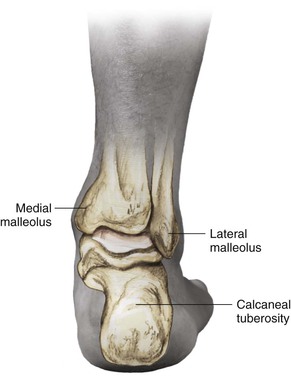
Calcaneus (Fig. 8-2)
The posterior surface has an area for insertion of the Achilles tendon
The anterior surface is triangular and concavoconvex and articulates with the cuboid
The groove of the calcaneus is between the posterior and middle facets, and it opens laterally to a rough quadrangle
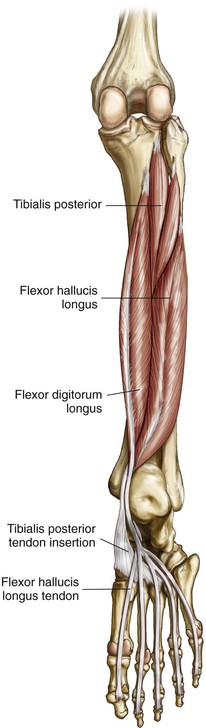
The thick medial border of the sustentaculum, with the tendons of the tibialis posterior above and the flexor digitorum longus (FDL) on its medial margin, is grooved inferiorly by the tendon of the FHL
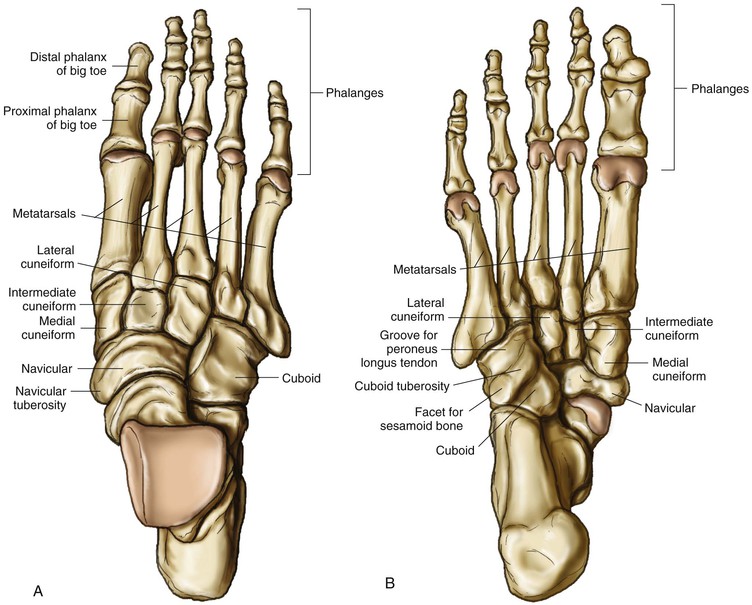
Cuboid (Fig. 8-3)
The anterior surface articulates with the fourth-fifth metatarsal base
The posterior surface articulates with the calcaneus
The superior surface has ligamentous attachments
The inferior surface has tuberosity and a groove for the peroneus tendon
The medial surface articulates with the late cuneiform and with the navicular
Sesamoids
The sesamoids are situated where tendons cross joints and change the direction of pull of tendons
The sesamoids also improve the mechanical advantage of the tendon
The medial and lateral sesamoids are constant
The following sesamoids are inconstant:
• Sesamoid of the tibialis posterior tendon
• Sesamoid in the peroneus longus tendon
• Sesamoids under the metatarsal heads, commonly under the second and fifth heads
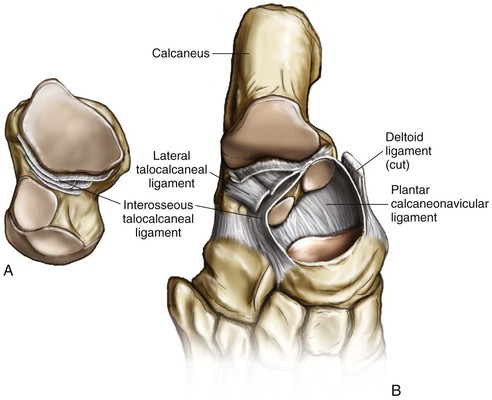
Arthrology
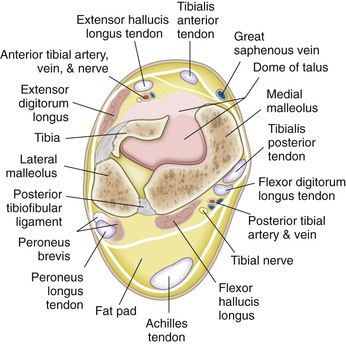
Ankle Joint (Figs. 8-5 to 8-7)
The ankle joint is a strong and stable joint
The ankle joint is a synovial hinge joint
A capsule encloses the joint and is attached to the bony articular margins
• Anterior talofibular ligament
• Posterior talofibular ligament
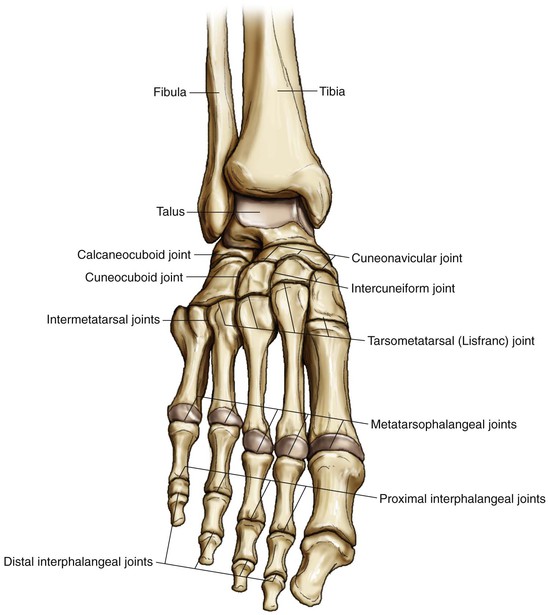
Tarsometatarsal (Lisfranc Joint) and Intermetatarsal Joints (see Fig. 8-8)
Metatarsophalangeal (MTP) and Interphalangeal Joints (see Fig. 8-8)
MTP joints are condyloid joints
Stabilized by plantar plates and oblique collateral ligaments
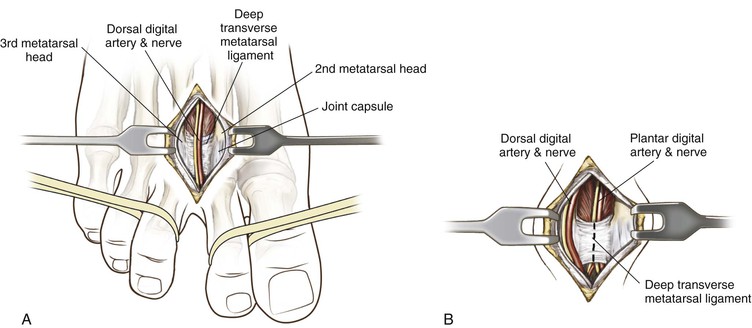
Deep transverse ligaments connect all five MTP joints
The second toe is long axis, and adduction-abduction is performed by interossei
Interphalangeal joints are hinge joints
• Interphalangeal joints only provide plantar flexion movement
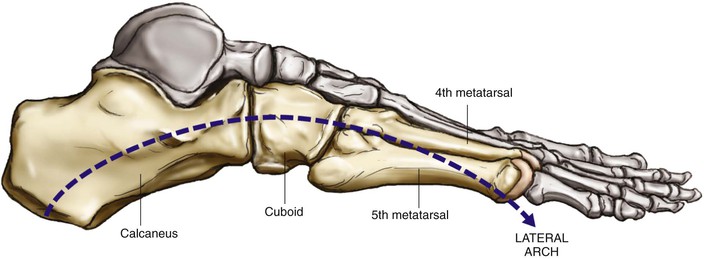
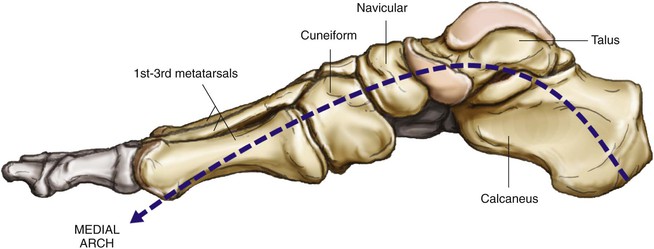
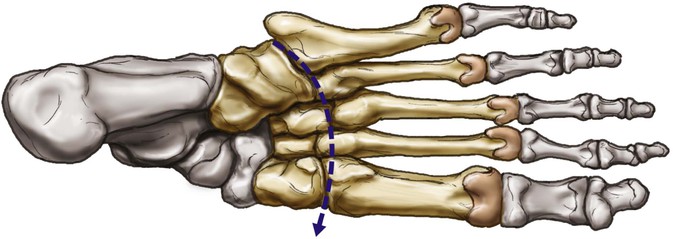
Arches of the Foot
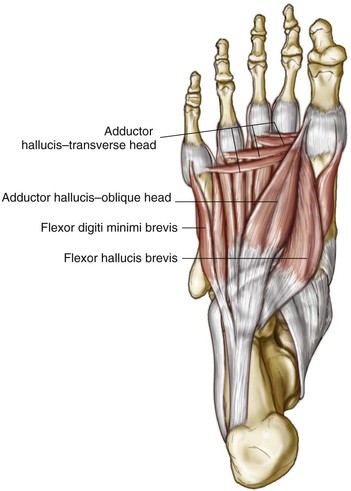
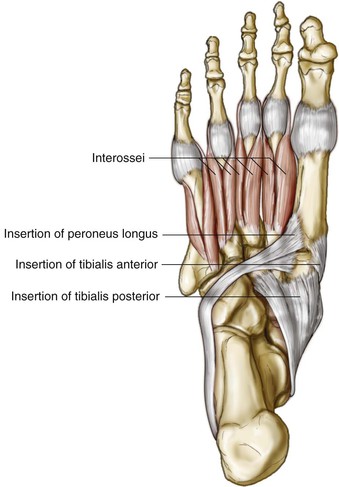
Muscles
Extrinsic Muscles
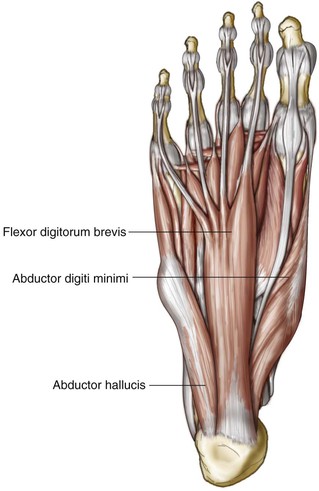
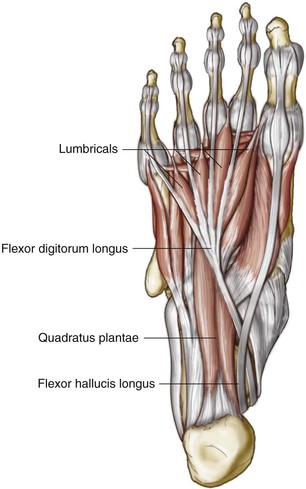
Muscles are in the leg, but their tendons function within the foot
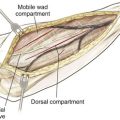
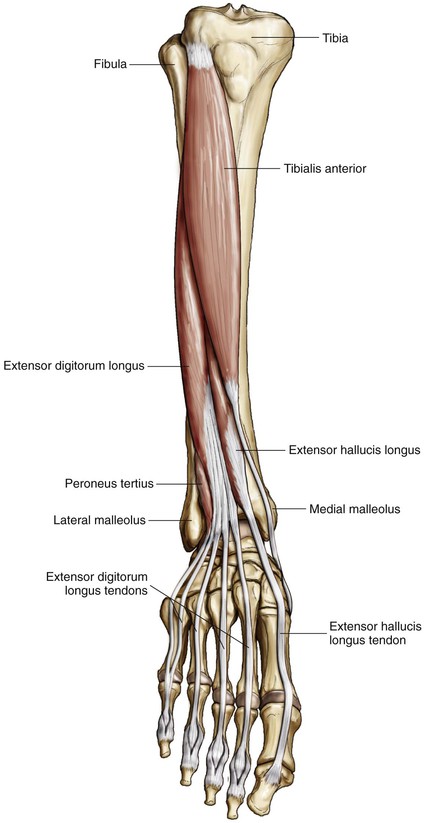
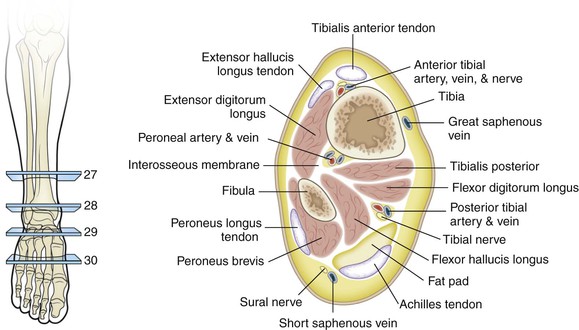
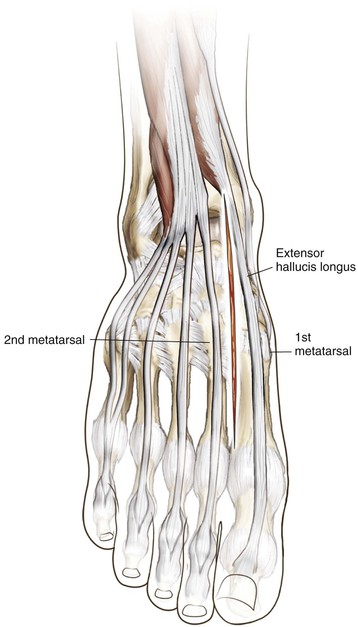
• Anterior compartment (innervated by the deep peroneal/anterior tibial nerve; Fig. 8-12)
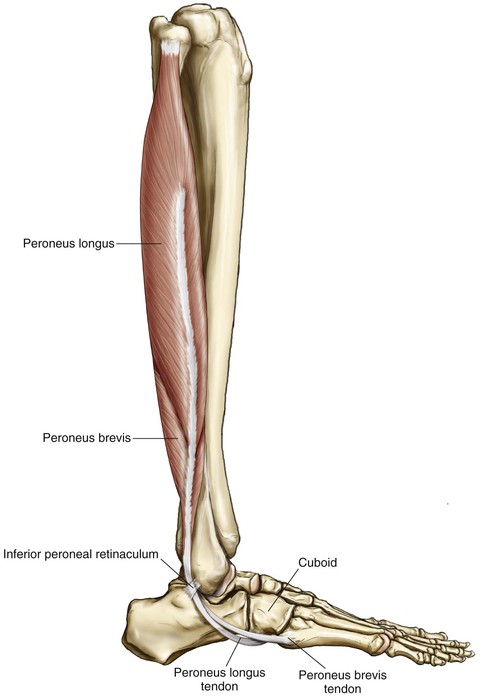
• Lateral compartment (innervated by the superficial peroneal nerve; Fig. 8-13)
• Peroneus longus and brevis muscle
• Tendons descend together in a common tendon sheath underneath the superior peroneal retinaculum
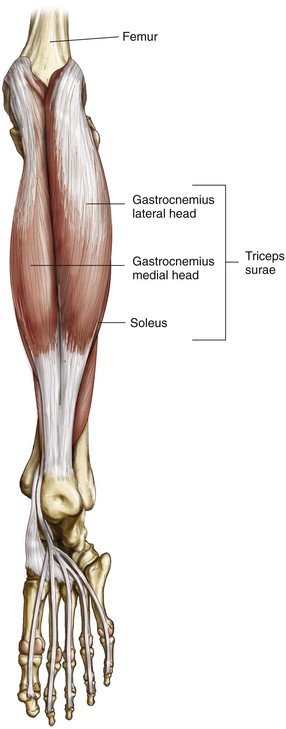
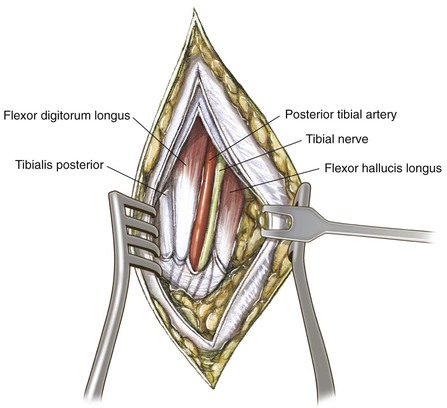
• Posterior compartment (innervated by the posterior tibial nerve; Figs. 8-14 to 8-16)
• Flexor digitorum longus (FDL)
• Flexor hallucis longus ( FHL)
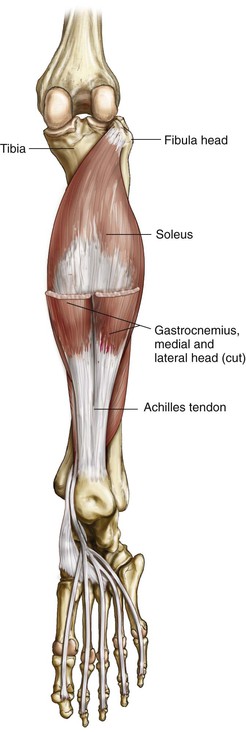
• Assisted by the peroneals, FHL, and FDL
• TA
• Assisted by the EHL, EDL, and peroneus tertius
• Eversion
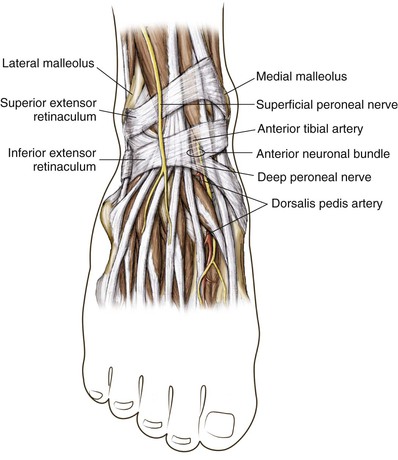
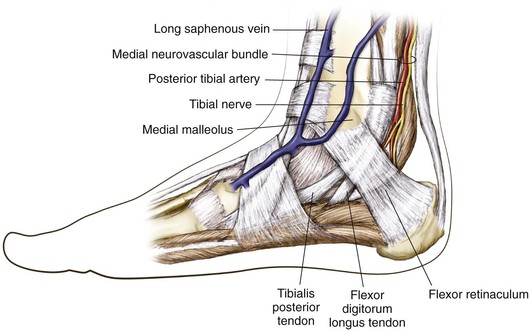
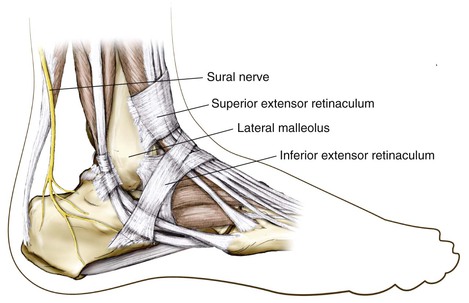
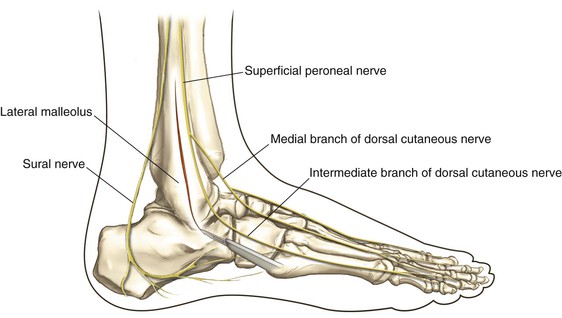
Nerves (Figs. 8-21 and 8-22)
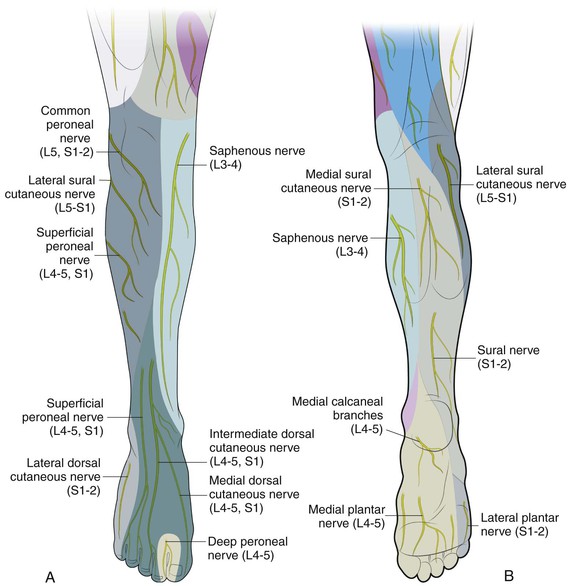
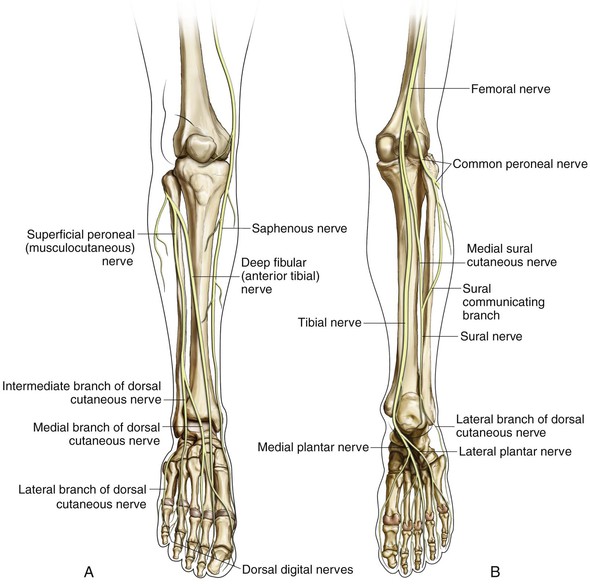
Sural Nerve
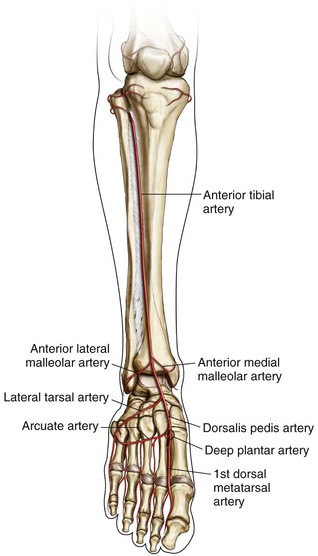
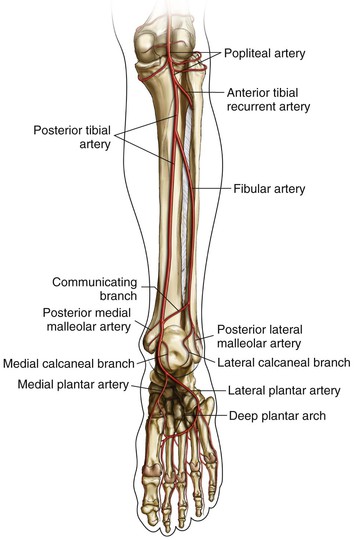
Vascularity (Figs. 8-23 and 8-24)
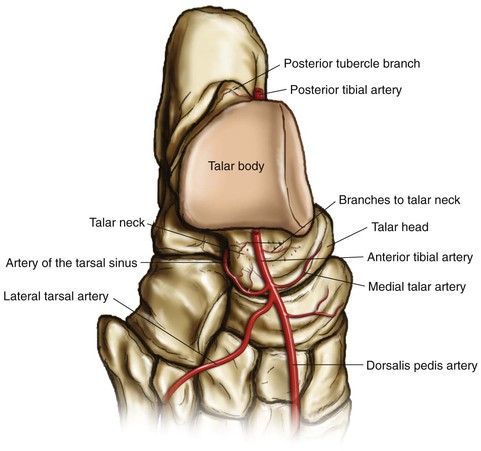
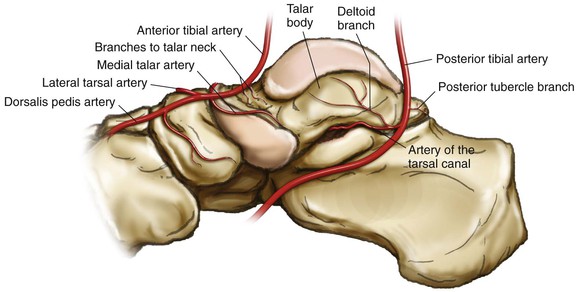
Blood Supply of the Talus (Figs. 8-25 and 8-26)
• Superior surface of the neck
• Medial talar arteries—medial recurrent tarsal artery (branch of the anterior tibial artery)
• Inferior surface of the neck
• Artery of the tarsal canal (branch of the posterior tibial artery)
• Deltoid branch (posterior tibial artery)
• Direct branch from the posterior tibial artery—infrequently from the peroneals
• Superior neck vessels and branches of the tarsal sinus artery
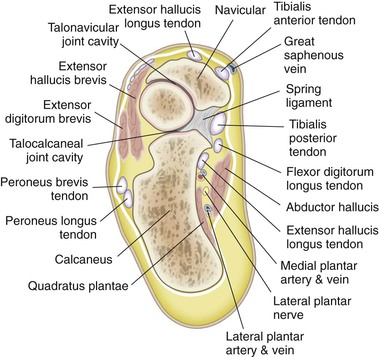
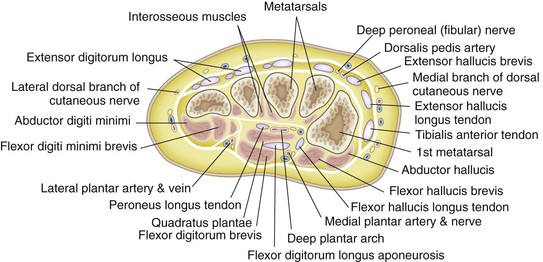
Cross-Sectional Anatomy
Foot and Ankle
Surface Landmarks
Surgical Approaches to the Ankle
Anterior Approach to the Ankle (Video 8-1)
Indications
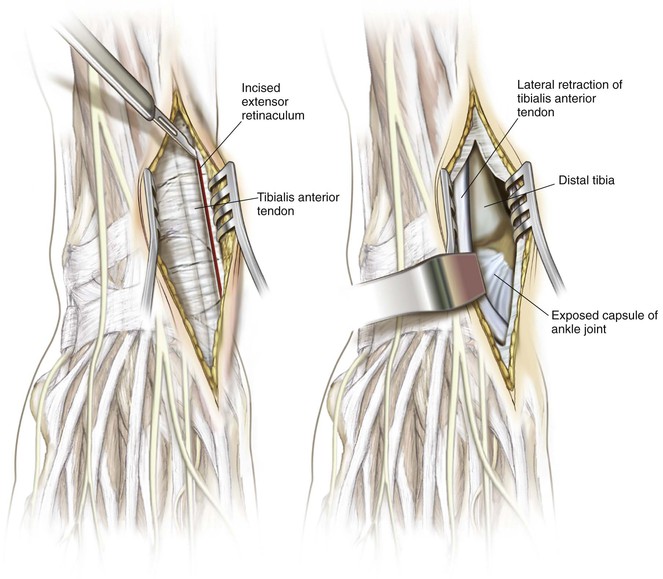
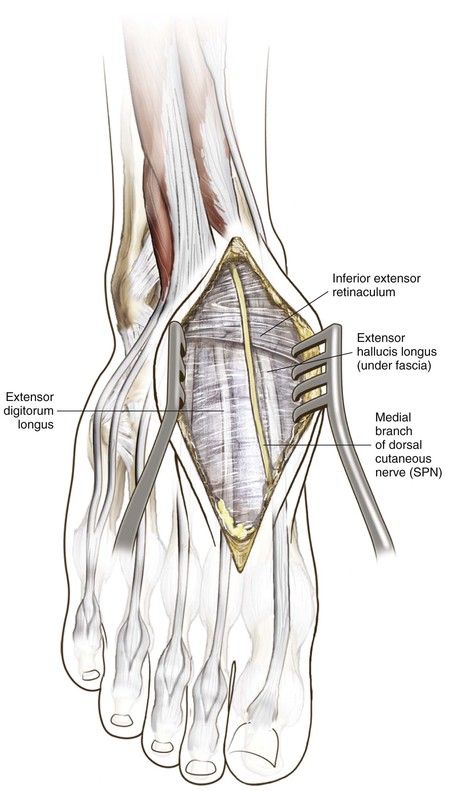
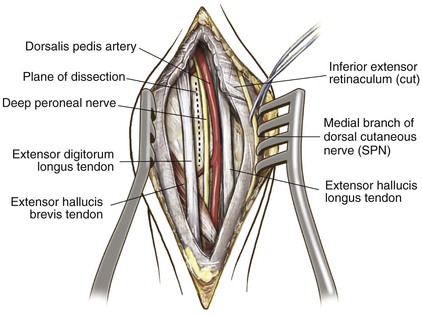
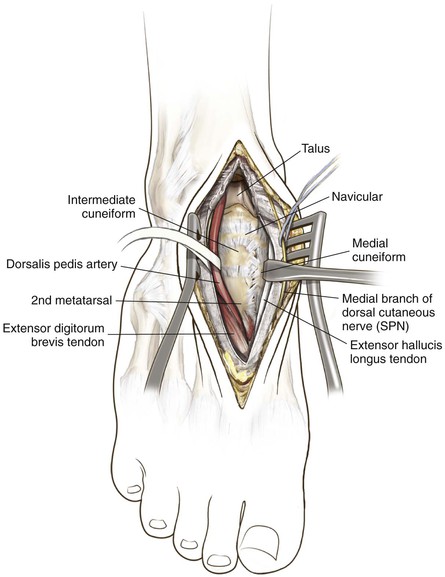
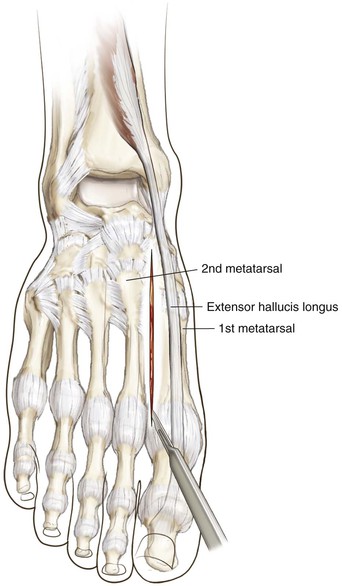
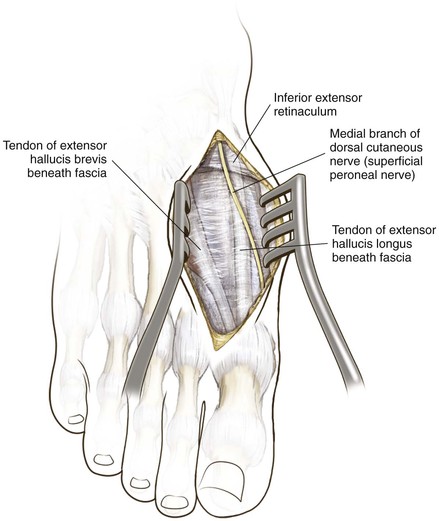
Superficial Dissection (TA/EHL Interval)
Superficial Dissection (Alternative—EHL/EDL Interval)
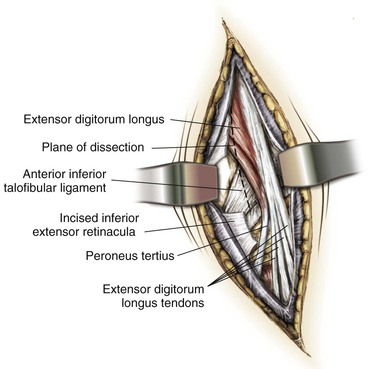
Incise the deep fascia of the leg in line with the skin incision
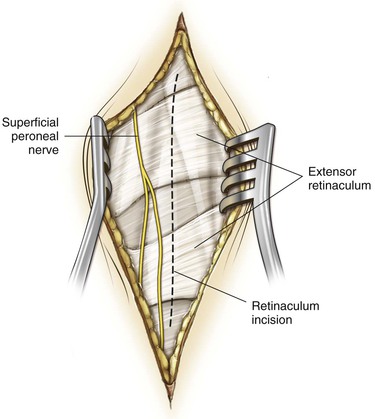
Incise the extensor retinaculum
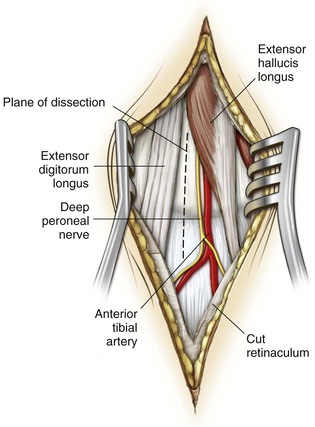
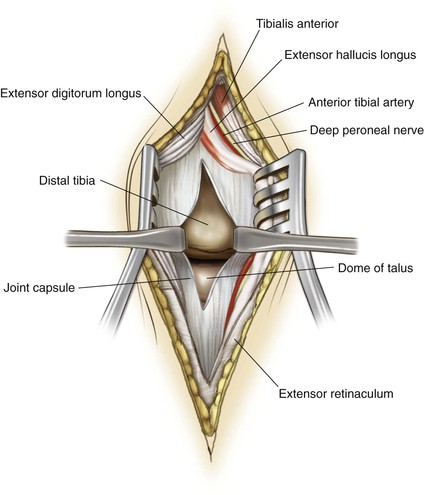
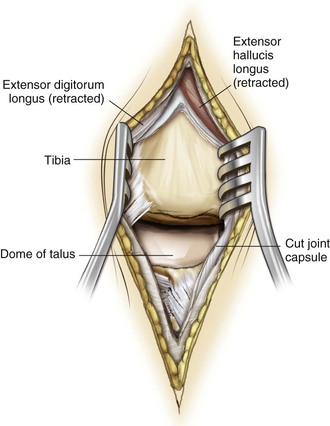
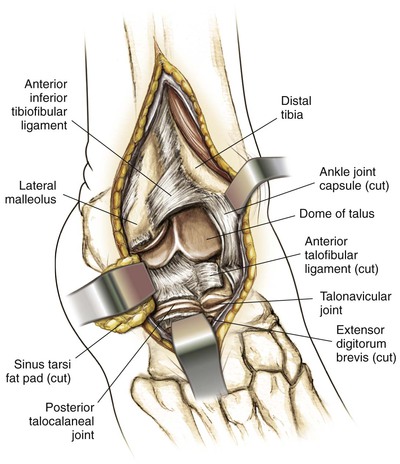
Find the plane between the EHL and EDL a few centimeters above the joint (Fig. 8-40)
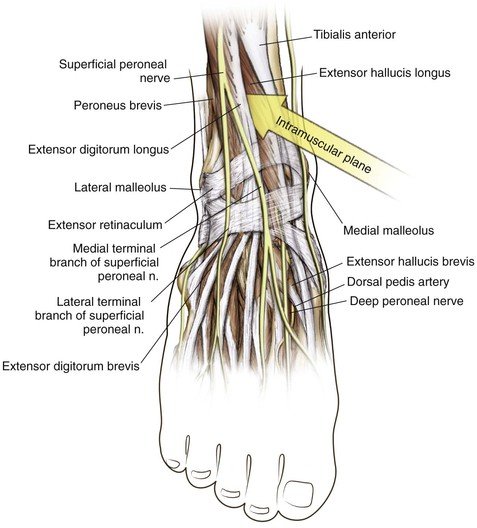
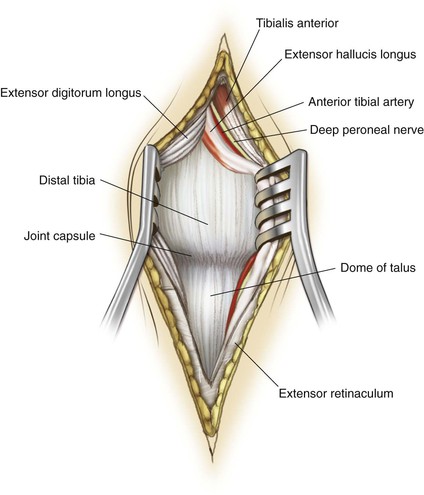
Identify and mobilize the anterior tibial artery and deep peroneal nerve
Retract the EHL and neurovascular bundle medially and the EDL laterally
This approach allows for distal extension to approach the dorsal mid foot (Fig. 8-41)
Anteromedial Approach to the Ankle (Video 8-2)
Indications
Ankle Arthrodesis
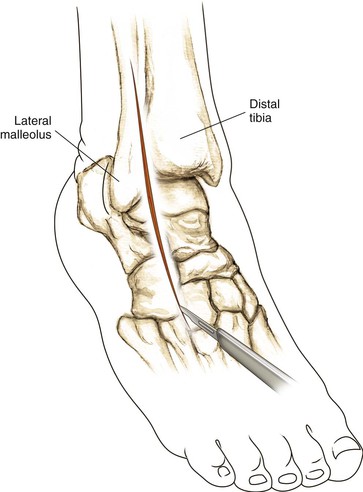
Anterolateral Approach to the Ankle
Indications
Superficial Dissection
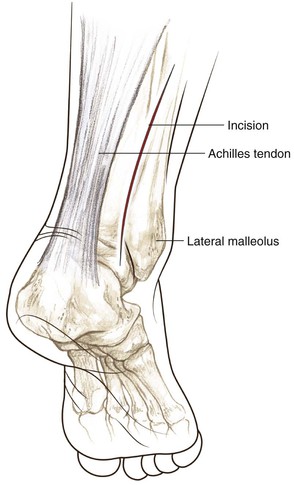
Direct Posterior Approach to the Achilles Tendon
Indications
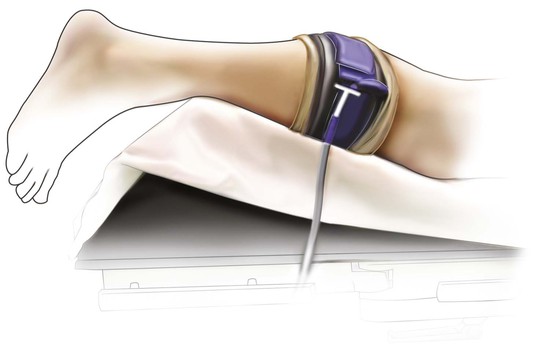
Position (Fig. 8-50)
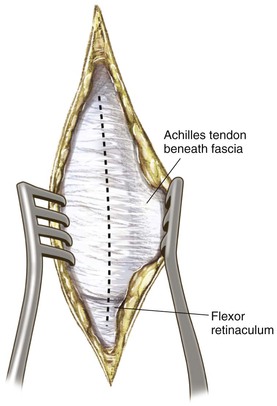
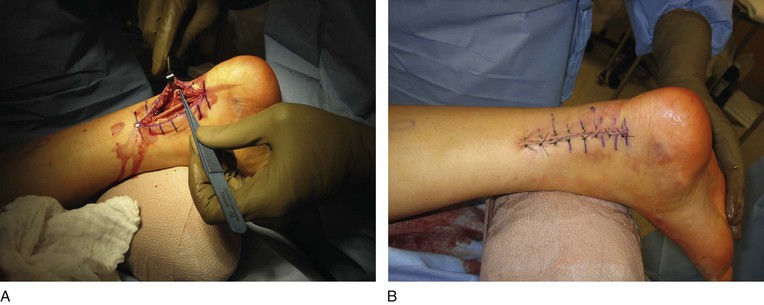
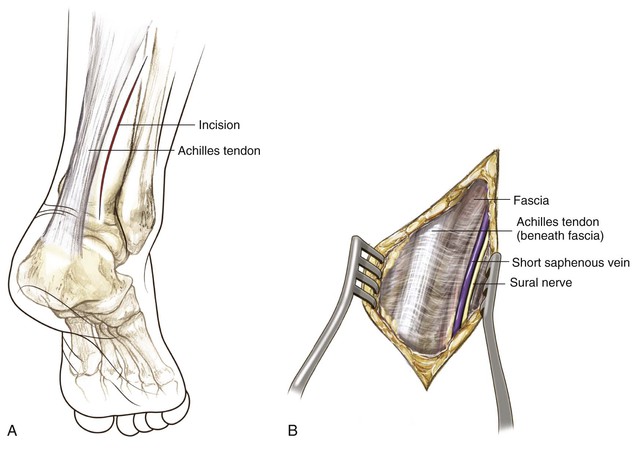
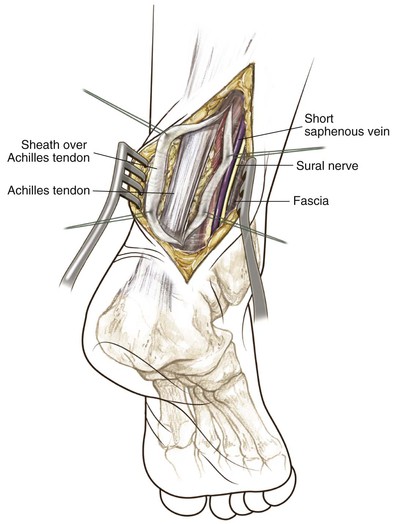
Surgical Exposure (Figs. 8-51 and 8-52)
For acute Achilles tendon ruptures
• A longitudinal incision is made 1 cm medial to the Achilles tendon to improve soft tissue coverage over the tendon after repair (Fig. 8-51); the deep fascia over the Achilles tendon is incised medial to the tendon
In an alternative approach an incision is made just lateral to the Achilles tendon (Fig. 8-52)
In patients with chronic tendinopathy, a midline posterior incision over the tendon is typically used to allow access to the calcaneus (Fig. 8-53)
• The paratenon is incised in the midline so that the paratenon can be closed after the reconstruction
Deep Dissection (Fig. 8-54)
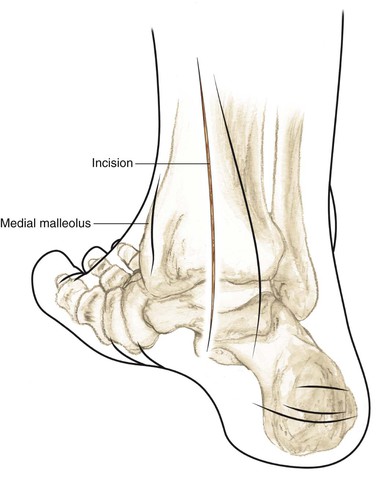
Posteromedial Approach to the Ankle
Indications
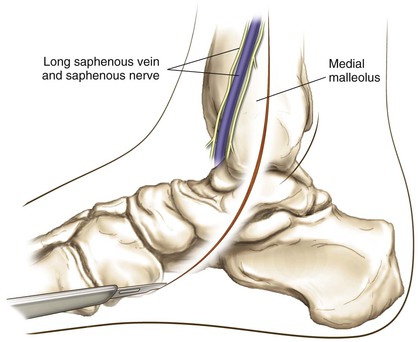
Superficial Dissection
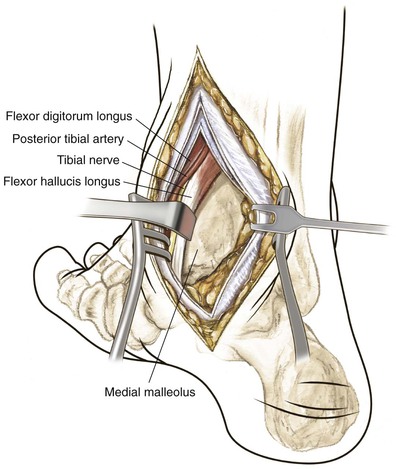
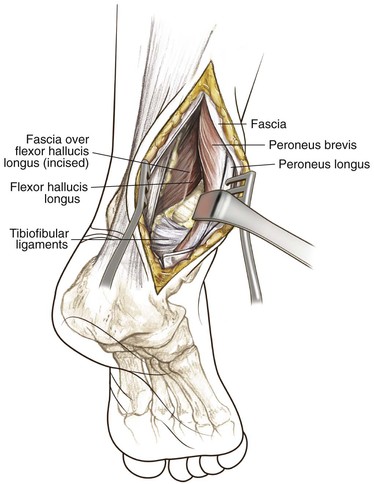
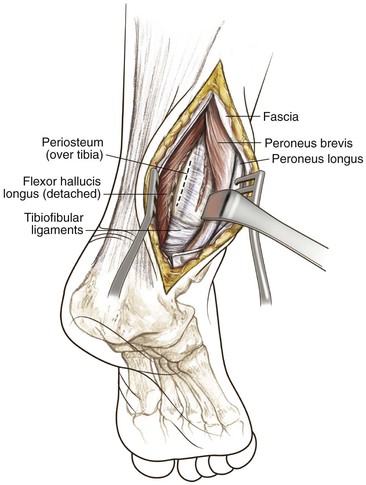
See Figs. 8-56 and 8-57
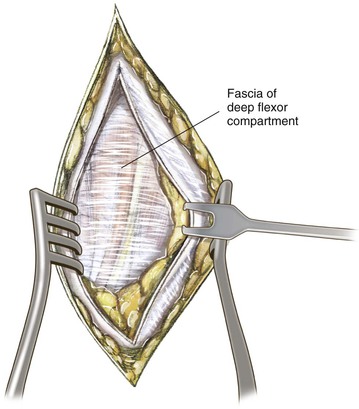
Deep Dissection
Using blunt dissection, identify the fat plane between the Achilles tendon and FHL (Fig. 8-58)
Retract the Achilles tendon and retrotendinous fat laterally, which exposes the fascia of the deeper flexor compartment (Fig. 8-59)
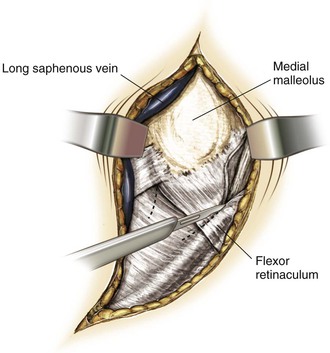
Identify the fascial plane in the anterior flap that covers the tendons of the flexor retinaculum
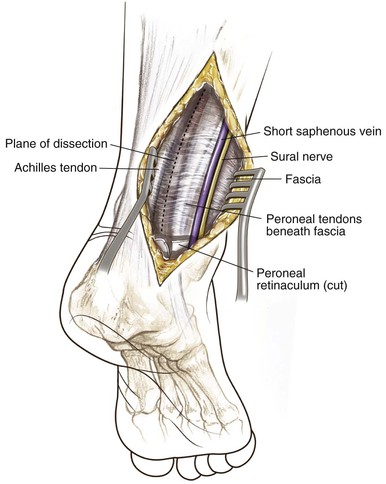
Posterolateral Approach to the Ankle (Video 8-3)
Indications
Transfibular Approach to the Ankle Joint
Indications
Superficial Dissection
The periosteum over the fibula is incised and the fibula is osteotomized obliquely (superolateral to inferomedial), ending approximately 2 cm above the ankle joint (Fig. 8-64); care should be taken not to osteotomize the fibula too proximally, which could disrupt the syndesmotic ligament; the planned location of the osteotomy should be marked provisionally with a Kirschner wire and confirmed on C-arm imaging; a sagittal saw can be used to perform the osteotomy, with cold irrigation to prevent thermal necrosis
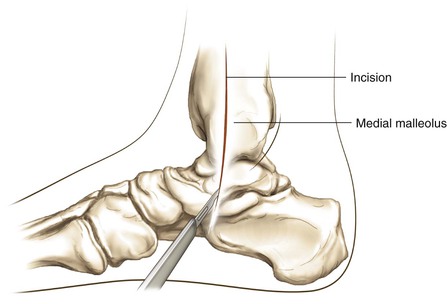
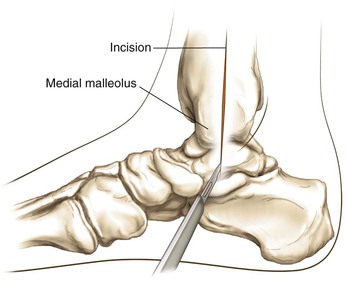
Approach to the Medial Malleolus (Video 8-4)
Indications
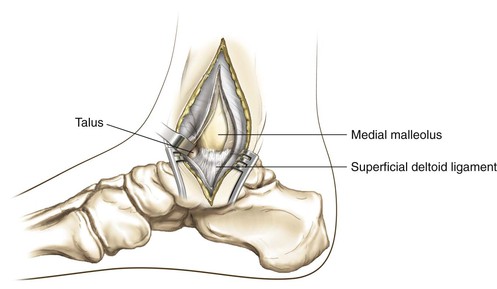
Medial Malleolar Osteotomy Approach to the Medial Talar Dome
Indications
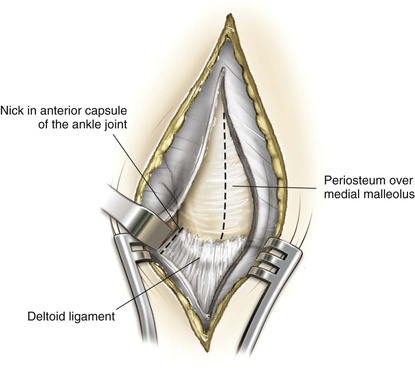
Deep Dissection
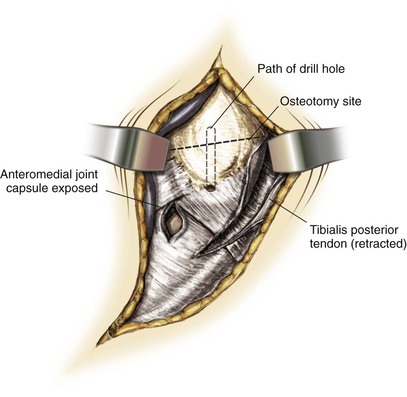
Expose the borders of the medial malleolus (Fig. 8-76)
• Place the retractor behind the medial malleolus to protect the posterior tibial tendon
Leave the attachment of the deltoid ligaments intact
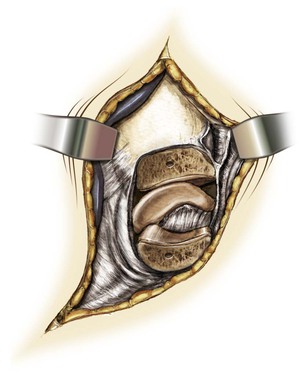
• Osteotomize the medial malleolus (Fig. 8-77)
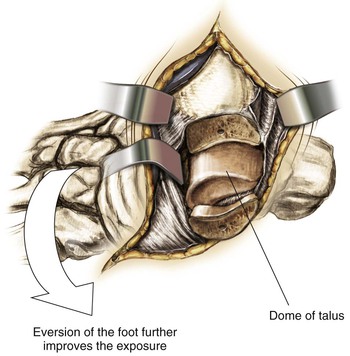
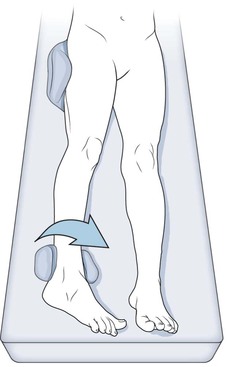
• This procedure exposes the dome of the talus and the articulating surface of the tibia into view (eversion of the foot improves the exposure further; Fig. 8-78)
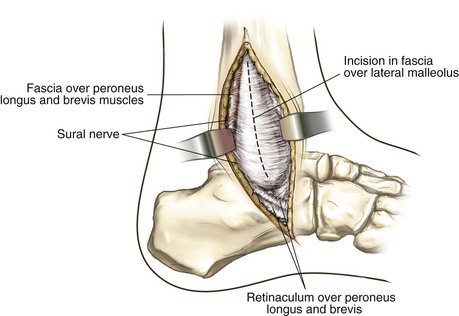
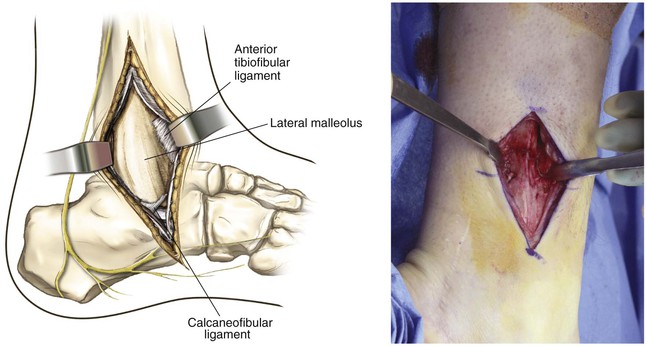
Approach to the Lateral Malleolus (Video 8-5)
Indications
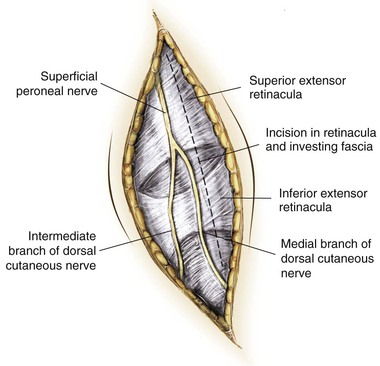
Superficial Dissection
Make a 12- to 15-cm incision along the posterior border of the fibula up to its distal end; the distal end can be either straight or be curved forward (see Fig. 8-80)
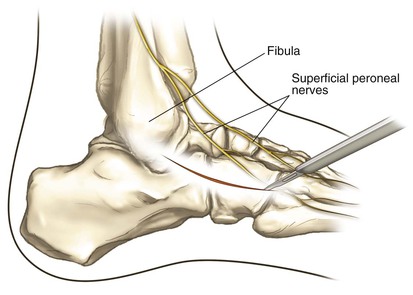
Elevate the anterior and posterior skin flaps, taking care to protect the superficial peroneal nerve and sural nerve and short saphenous vein posterior to the lateral malleolus (Fig. 8-81)
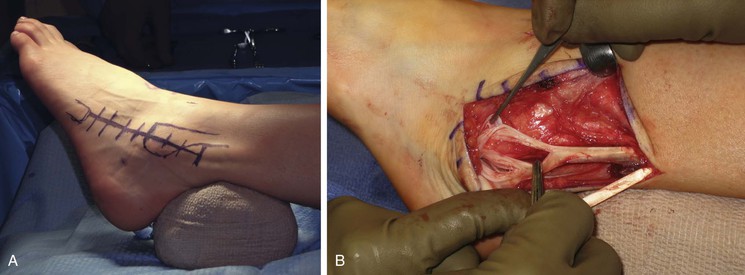
Oblique Lateral Incision—Utility Approach to the Lateral Ankle
Indications
Lateral ligament reconstruction
Peroneal tendon exploration/repair
Incision
An oblique incision is made beginning at the posterior border of the fibula, 7 to 8 cm proximal to the tip, and coursing distally toward the sinus tarsi, crossing the distal fibula between the approximate origins of the calcaneofibular ligament (CFL) and anterior talofibular ligament (ATFL) (Fig. 8-83)
Surgical Approaches to the Hind Foot
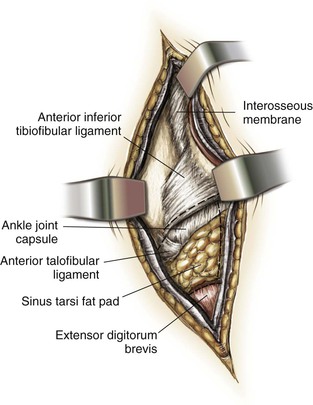
Subtalar Joint Approach—Lateral Approach
Indications
Deep Dissection
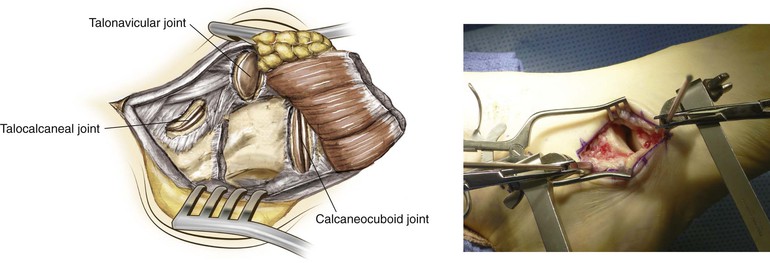
Interosseous ligaments are sharply incised and the subtalar joint is exposed
• A laminar spreader or Hintermann retractor is used to distract the joint for visualization
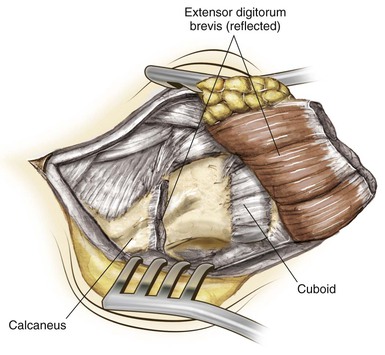
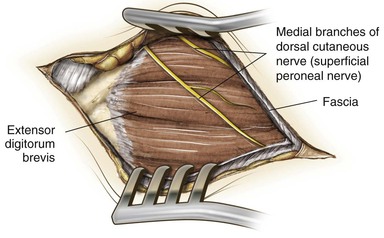
Exposure of the CC joint: the extensor digitorum brevis muscle is identified and further elevated from the calcaneus and the muscle is retracted dorsally to expose the CC joint (Fig. 8-86).
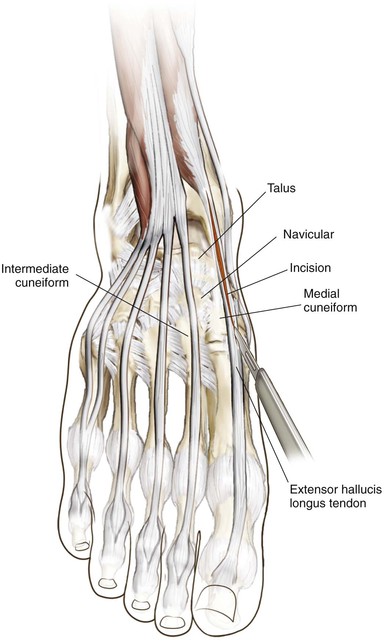
Dorsal Approach to the Talus
Indications
Incision
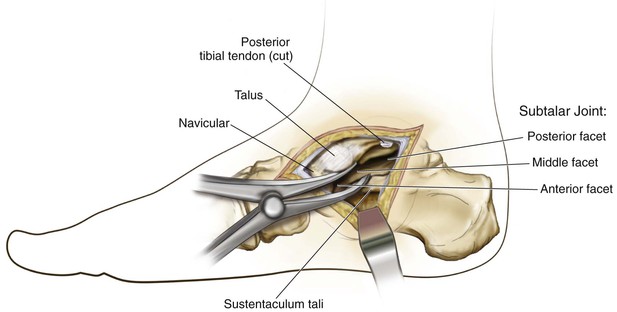
Medial Approach for the Hind Foot
Indications
Deep Dissection
The capsule of the subtalar joint is incised and interosseous ligaments are released
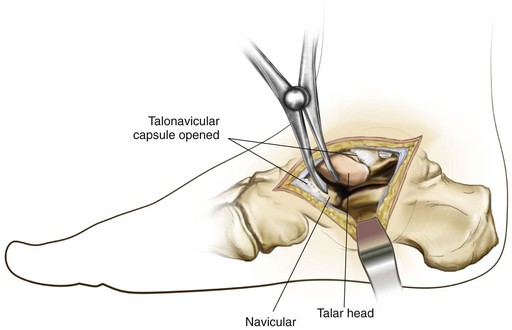
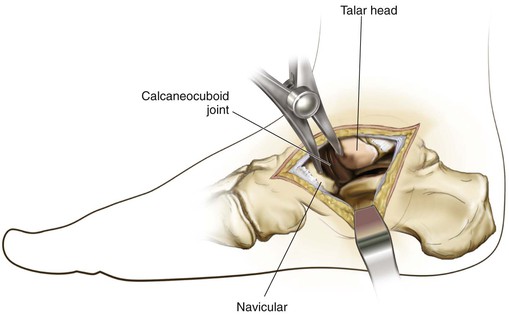
The CC joint can be approached by applying the laminar spreader in between the navicular and the head of the talus (the TN joint capsule is incised and opened); the CC joint lies deep/lateral to the TN articulation (Figs. 8-92 and 8-93)
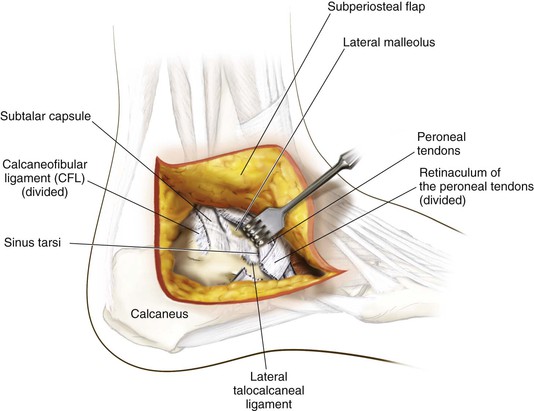
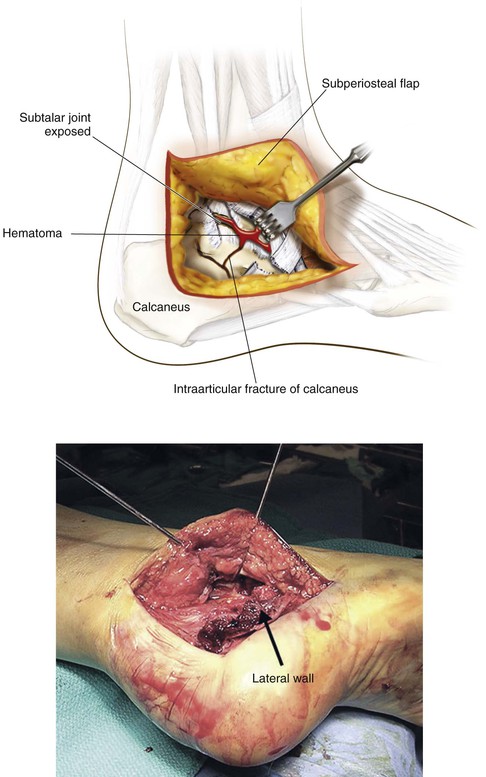
Extensile Lateral Exposure for Calcaneal Fracture Fixation (Video 8-6)
Indications
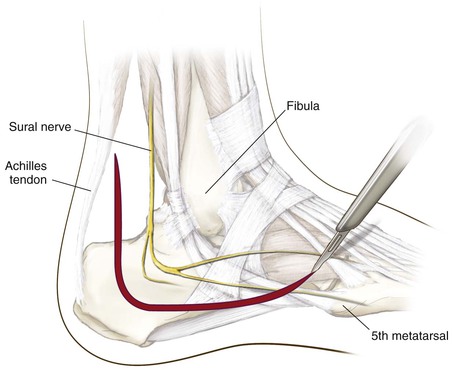
Hazards
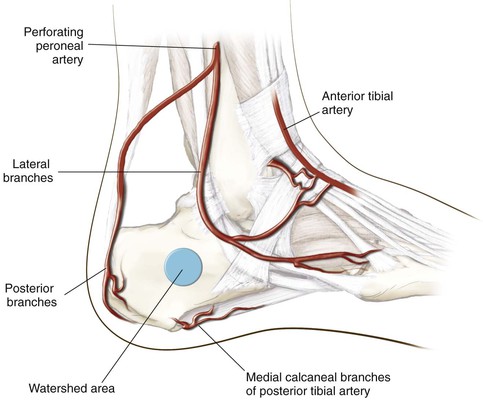
The vascular supply to the planned flap is a “watershed” area; the corner of the soft tissue flap at the juncture of the longitudinal and vertical posterior incisions must be treated with infinite care (Fig. 8-95)
• Sural nerve injury can occur in the proximal and distal aspects of the L-shaped incision
Development of a Flap
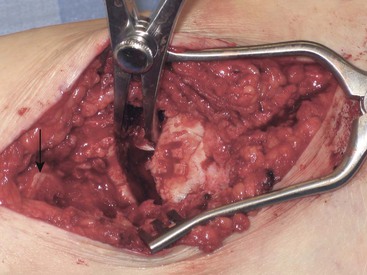
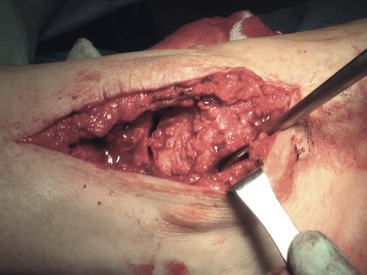
The peroneal tendons and the sural nerve are within the proximal flap and are mobilized from the lateral aspect of the calcaneus; as the flap is developed superiorly, the subtalar joint and the sinus tarsi are exposed (Fig. 8-96)
The lateral wall of the calcaneus and the subtalar joint is exposed to reduce and fix intraarticular fractures of the calcaneus (Fig. 8-97)
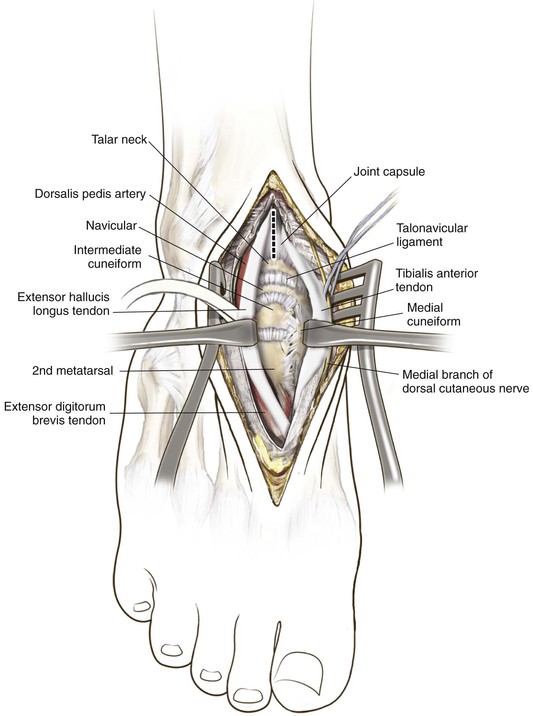
Approaches to the Mid Foot/Metatarsals
Extensile Dorsomedial Exposure to the Mid Foot
Indications
Superficial Dissection
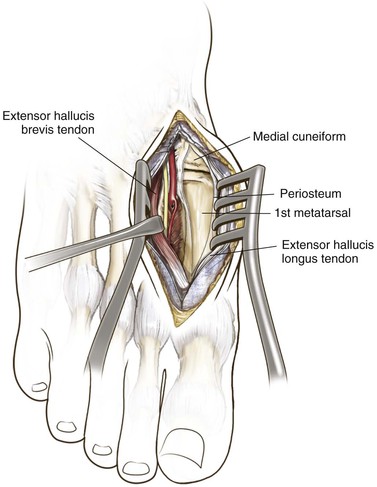
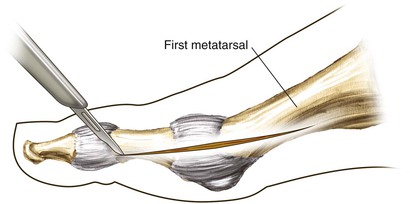
Dorsal Approach to the First Proximal Metatarsal
Indications
Superficial Dissection
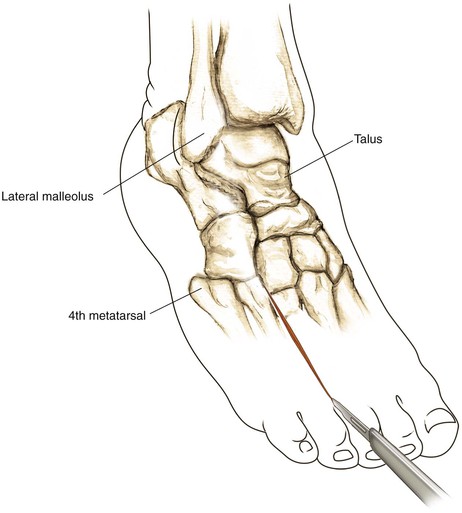
Dorsolateral Approach to the Mid Foot
Indications
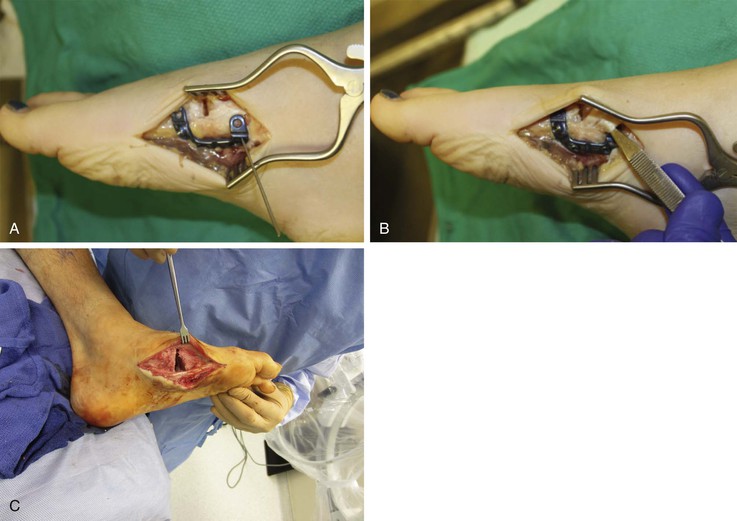
Plantar Plating of the Medial Column
Indications
Incision
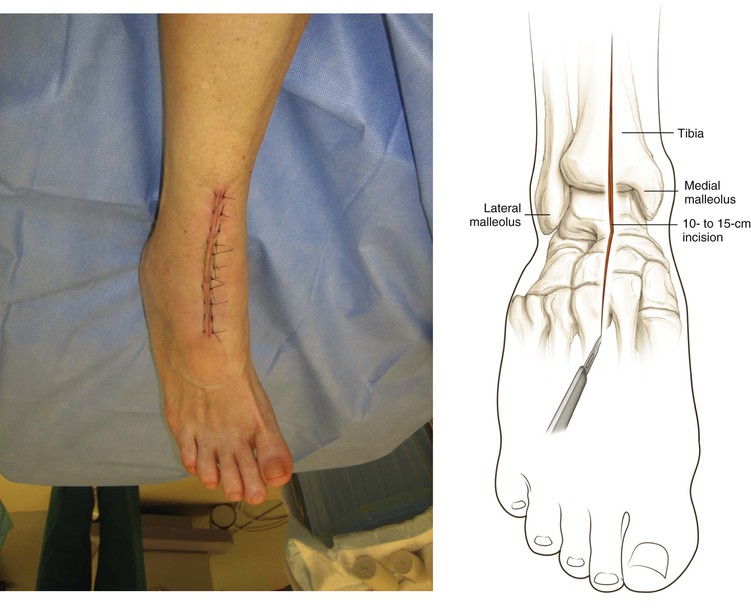
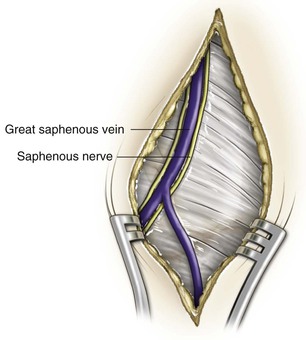
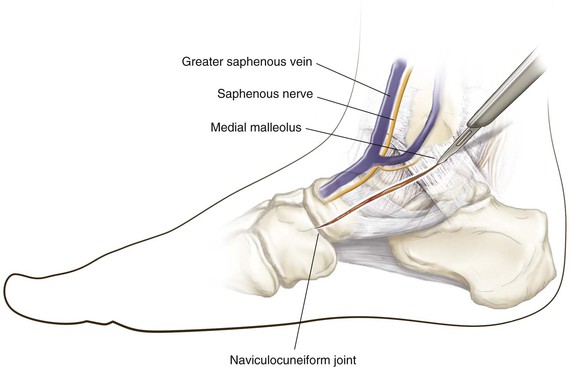
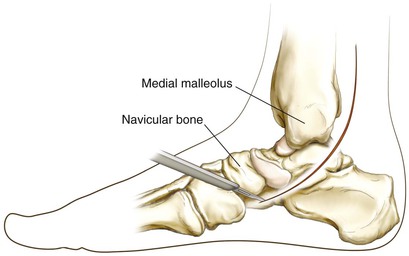
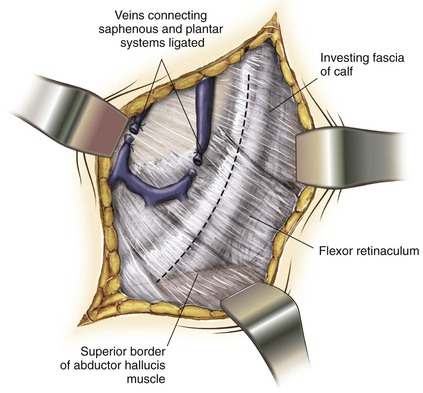
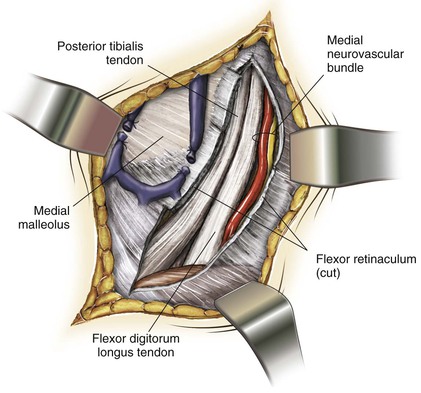
Approach to the Tarsal Tunnel/Posterior Tibial Tendon (Video 8-7)
Indications
Approaches to the Forefoot
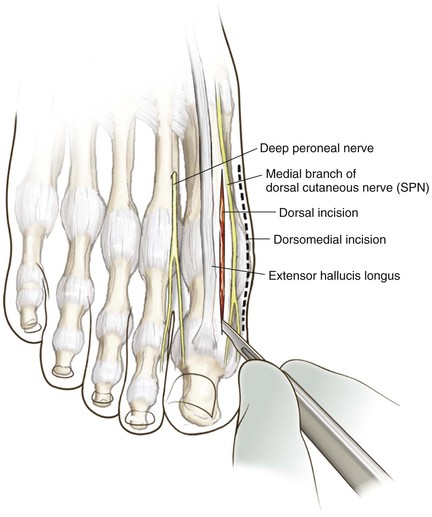
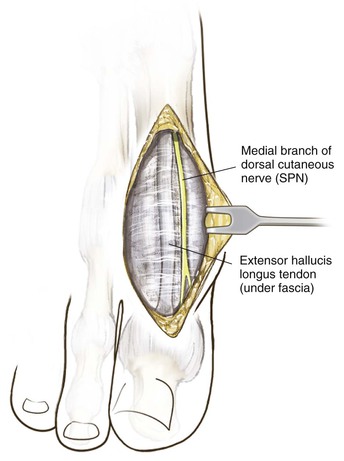
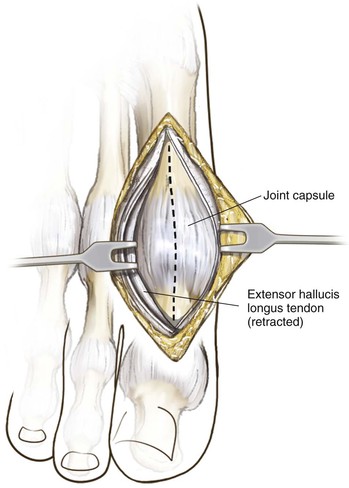
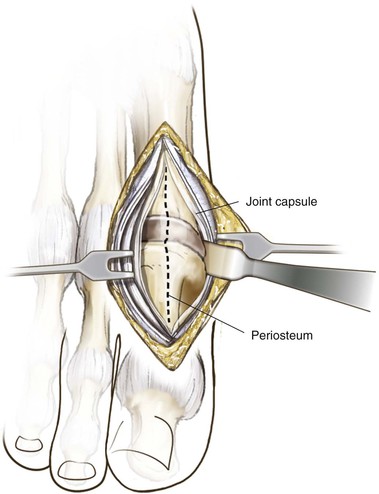
Dorsal Approach to the First MTP Joint (Video 8-8)
Indications
Superficial Dissection
Deep Dissection
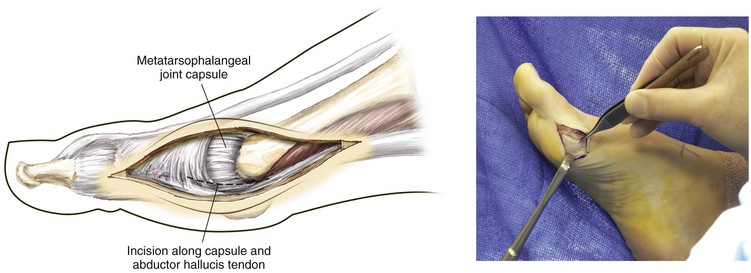
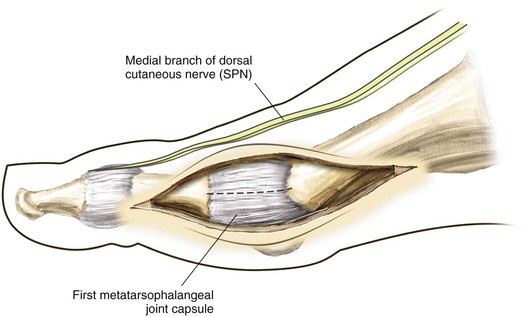
Medial Approach to the First MTP Joint and Medial Sesamoid (Video 8-9)
Indications
Superficial Dissection
Deep Dissection
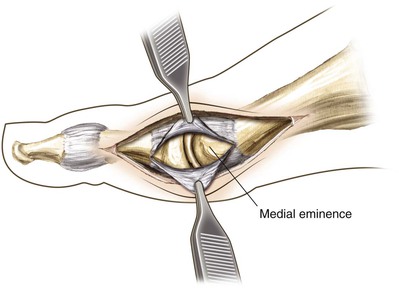
Using sharp dissection, incise the capsule along the length of the incision and reflect the capsule surrounding the exostosis to expose the medial eminence (Fig. 8-116)
Preserve as much of the proximal capsular attachment to the metatarsal neck as possible
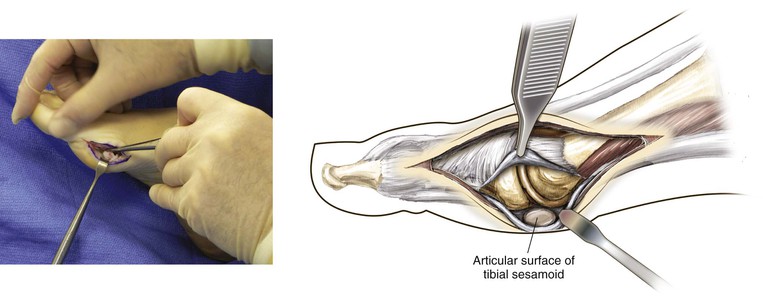
For medial sesamoid excision, the capsular incision is placed plantarly to expose the sesamoid (Figs. 8-117 and 8-118)
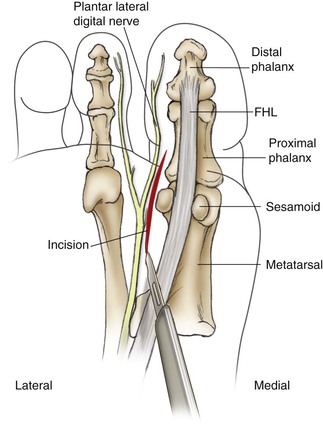
Plantar Approach for the Lateral (Fibular) Sesamoid/Plantar Plate
Indications
Deep Dissection
The distal (sesamoidophalangeal ligament), proximal (flexor hallucis brevis), medial (FHL), and lateral (adductor hallucis) borders should be carefully delineated to avoid potential injury; remember that the FHL runs between the sesamoids and can be injured when incising the intersesamoid ligament (Fig. 8-119)
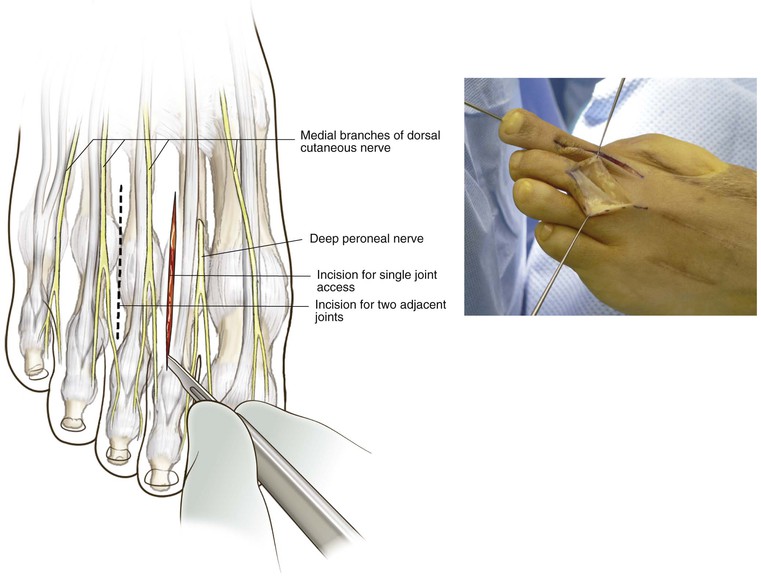
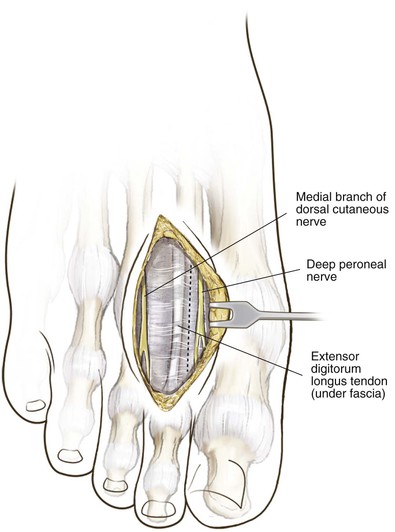
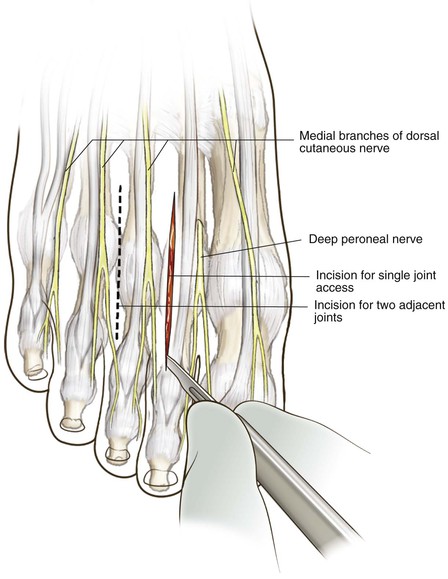
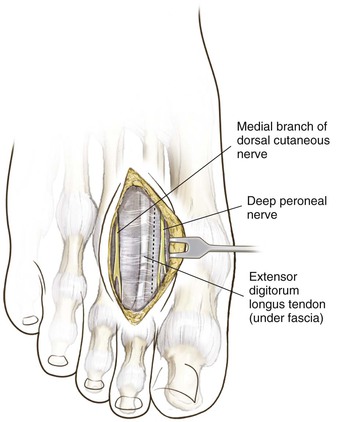
Dorsal Approach for the Lesser MTP Joints
Indications
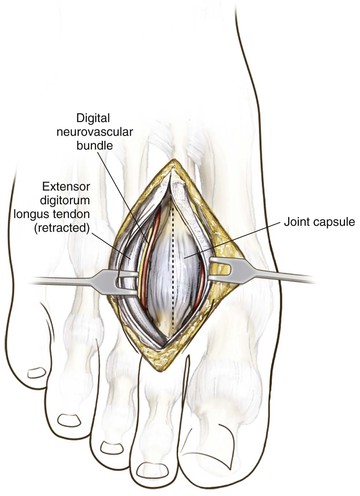
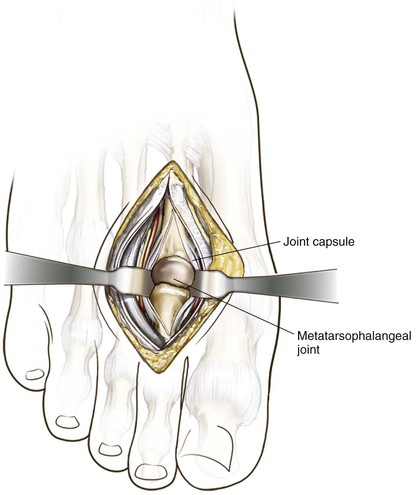
Superficial Dissection
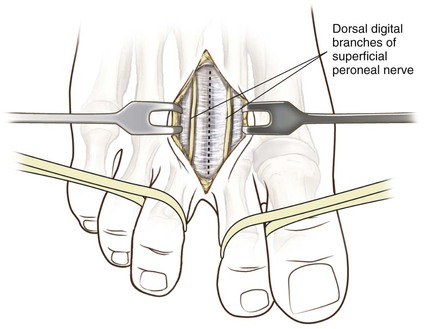
The digital branches of the dorsal cutaneous nerve are carefully retracted
Once the deep fascia is incised, the extensor digitorum longus (EDL) is visualized and the tendon is moved laterally to expose the joint; the extensor digitorum brevis (EDB) is lateral to the longus and is also protected during retraction (Fig. 8-121)
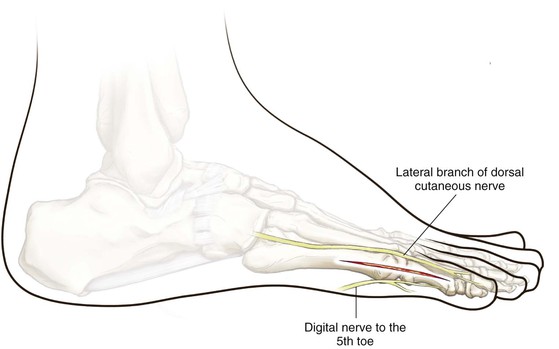
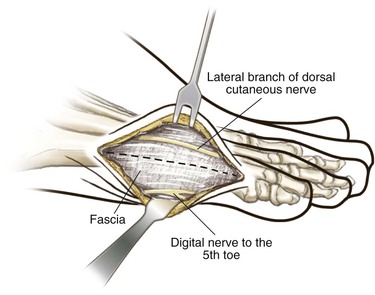
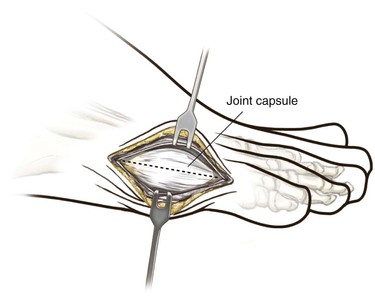
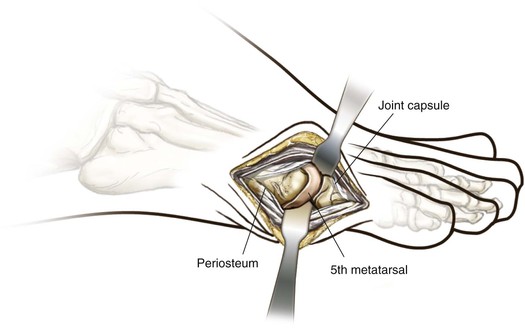
Lateral Approach for the Fifth MTP Joint and the Fifth Metatarsal (Video 8-10)
Indications
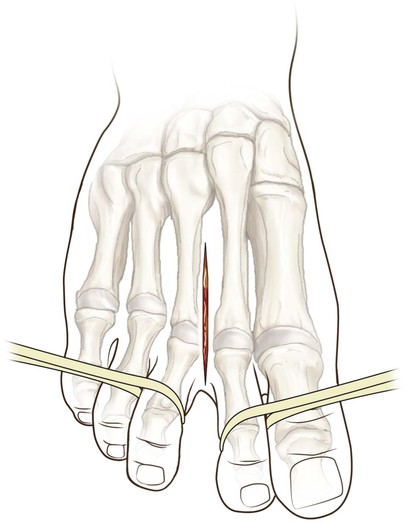
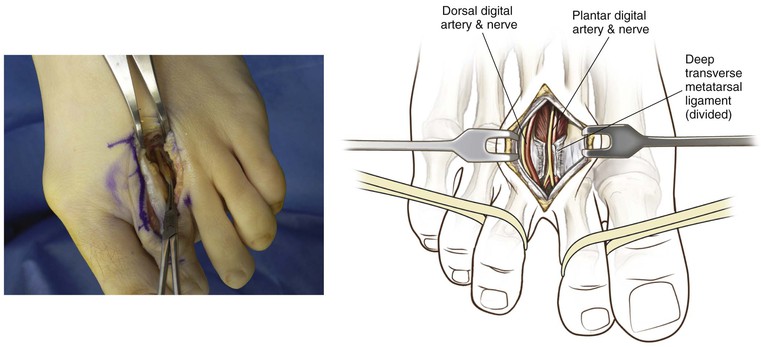
Approach to the Dorsal Web Space
Indications
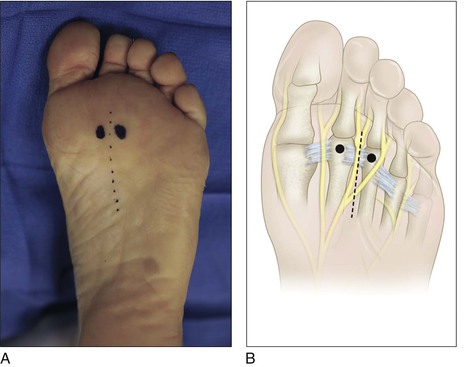
Plantar Approach for Recurrent Interdigital Neuroma
Indications
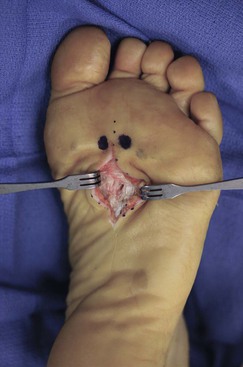
Deep Dissection
The nerve runs directly beneath the fascia
• The transverse metatarsal ligament is then identified
• Often the neuroma is identified plantar to the transverse metatarsal ligament
• The nerve is generally traced proximally from that point and transected at the non–weight-bearing portion of the foot after injection of a local anesthetic (Fig. 8-131)
Excise the distal part of the nerve with the neuroma (Fig. 8-132)
Dorsal Approach to the MTP Joints of the Second Through Fifth Toes with Proximal Interphalangeal Joint Exposure (Videos 8-11 and 8-12)
Indications
Arthroscopic Approaches to the Foot and Ankle
Anterior Ankle Arthroscopy
Positioning
Supine, with a bump beneath the ipsilateral hip to maintain internal rotation
• A leg holder is placed proximally beneath the operative thigh
If desired, apply a calf tourniquet (apply an Esmarch bandage prior to making the incision)
• A noninvasive ankle distractor is applied (Figs. 8-137 and 8-138)
Portal Placement
• Just medial to the TA tendon at the level of the ankle joint (Fig. 8-139)

• Insufflate the ankle with 10 mL of lidocaine with epinephrine; the joint is localized using a 25-gauge needle (Fig. 8-140)

• A 1.5-cm incision is made, and then a straight hemostat is used to spread down to capsule and to enter through the joint capsule (Fig. 8-141)

• A blunt trocar is then inserted, followed by a 2.7-mm arthroscope (Fig. 8-142)
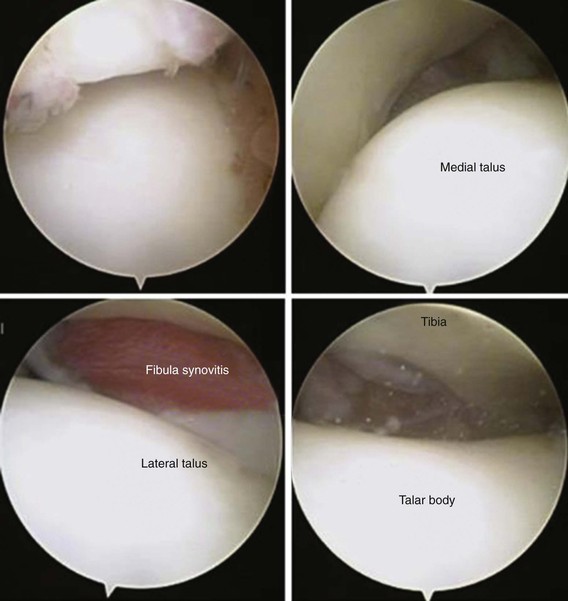
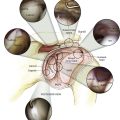
Arthroscopic Examination
Posterior Ankle Arthroscopy
Indications
Bone (os trigonum, loose bodies, ossicles, posttraumatic ossifications, and osteophytes)
Cartilage (posterior talar, tibial, osteochondral defects, and chondromatosis lesions)
Procedure
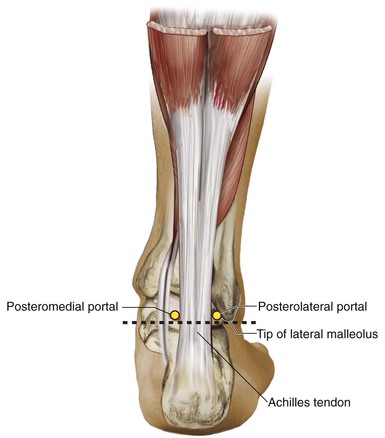
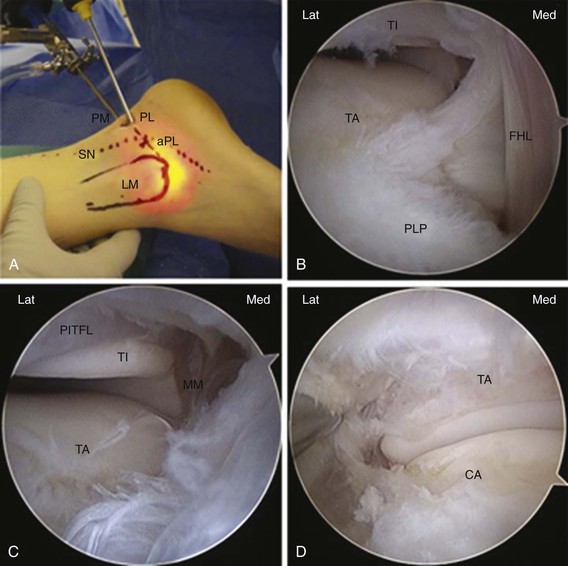
Mark the anatomic landmarks, including the Achilles tendon and the lateral malleolus (Fig. 8-147)
• The posterolateral portal is made just lateral to the Achilles tendon and just proximal to the line drawn from the tip of the lateral malleoli to the Achilles tendon (Fig. 8-147)
• The posteromedial portal is located at the same level on the medial side of the Achilles tendon
A vertical 1.5-cm skin incision for the posterolateral portal is made; dissection of the subcutaneous tissue and deeper layers is performed bluntly with a straight hemostat, which is oriented toward the first interdigital space
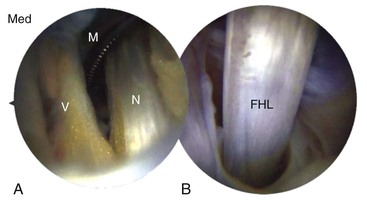
A scope is placed in the posterolateral portal and the shaver is placed in the posteromedial portal; triangulation is used to locate the shaver, and the capsule/synovitis posterior to the ankle joint is debrided to identify the FHL (Fig. 8-148)
• Passive motion of the great toe will assist in identification of the FHL
Both ankle and subtalar joints can be approached (Fig. 8-149)
• The following structures can be identified from lateral to medial: lateral malleolus, posterior inferior tibiofibular ligament, posterior talofibular ligament, CFL, FHL, posterolateral process of the talus, posterior tibiotalar ligament (part of the deep deltoid), and medial malleolus (Fig. 8-150)
The subtalar joint is clearly visible below the posterior talofibular ligament
Subtalar Arthroscopy
Indications
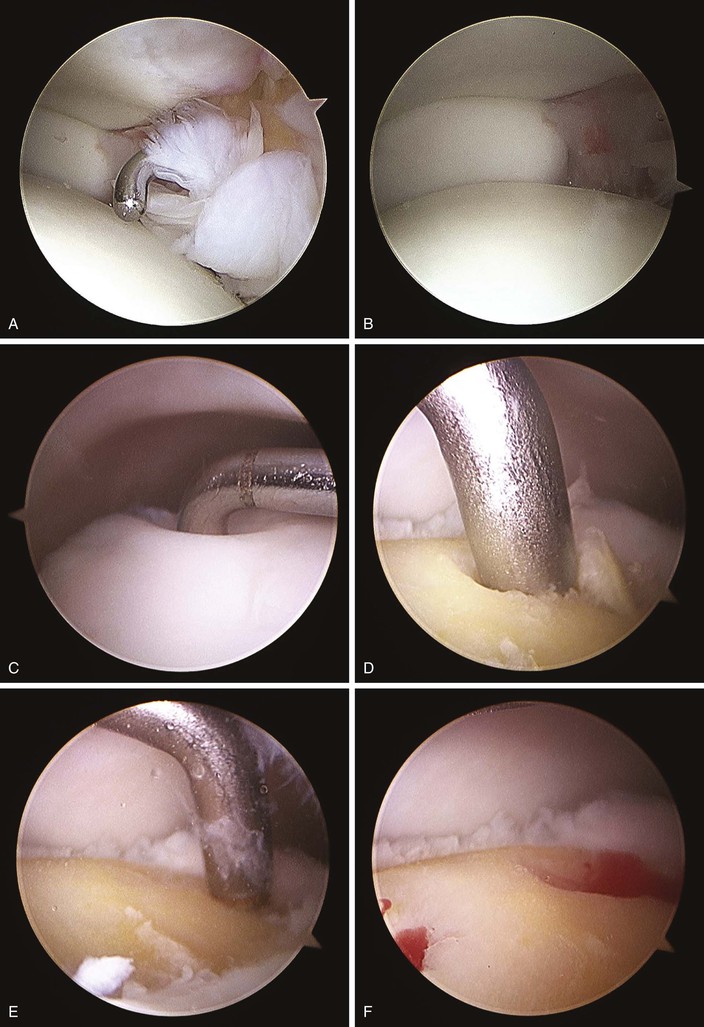
Procedure
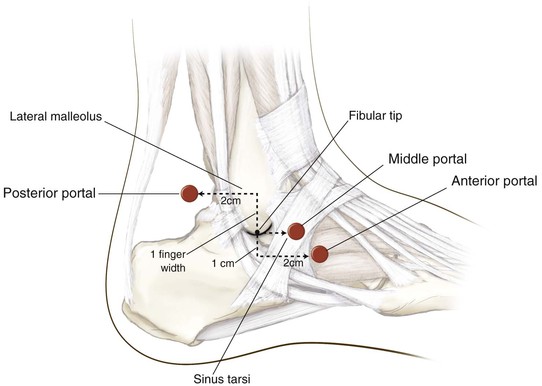
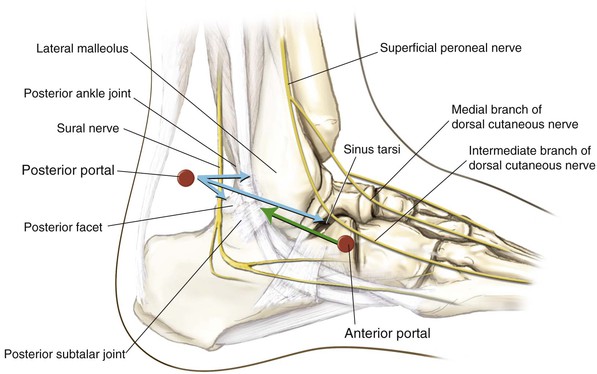
The anterior portal is established approximately 1 cm distal to the fibular tip and 2 cm anterior to it; the middle portal is just anterior to the tip of the fibula, directly over the sinus tarsi; the posterior portal is approximately one finger width proximal to the fibular tip and 2 cm posterior to the lateral malleolus (Figs. 8-151 and 8-152)

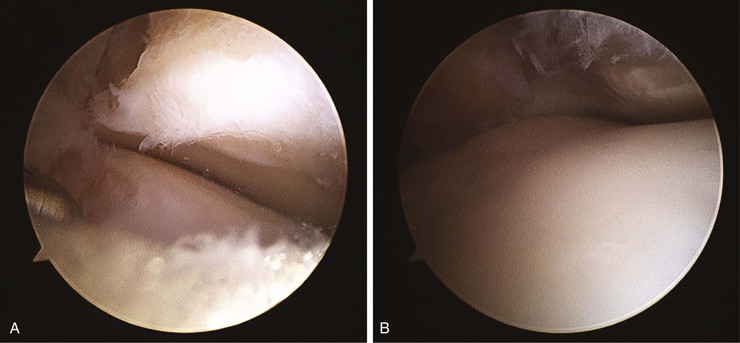
Use of the anterior portal to visualize the posterior subtalar joint, with instrumentation through the posterior portal, allows the best access to the posterior facet, sinus tarsi, and posterior ankle joint (Fig. 8-153)
The arthroscopic lens is rotated in the opposite direction to view the anterior aspect of the posterior talocalcaneal articulation (Fig. 8-154)
The arthroscopic lens may then be rotated medially, and the central articulation between the talus and the calcaneus observed (Fig. 8-155). The posterolateral gutter may be seen from the anterior portal.





 interdigital nerve)
interdigital nerve)