CHAPTER 26 Femoropopliteal Bypass
INDICATIONS FOR FEMOROPOPLITEAL BYPASS
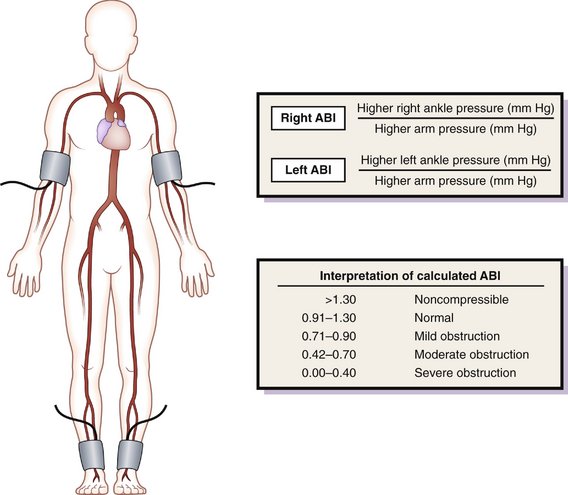
PREOPERATIVE EVALUATION
COMPONENTS OF THE PROCEDURE AND APPLIED ANATOMY
General Operative Principles of Lower Extremity Bypass
Preoperative Considerations
Patient Positioning and Preparation
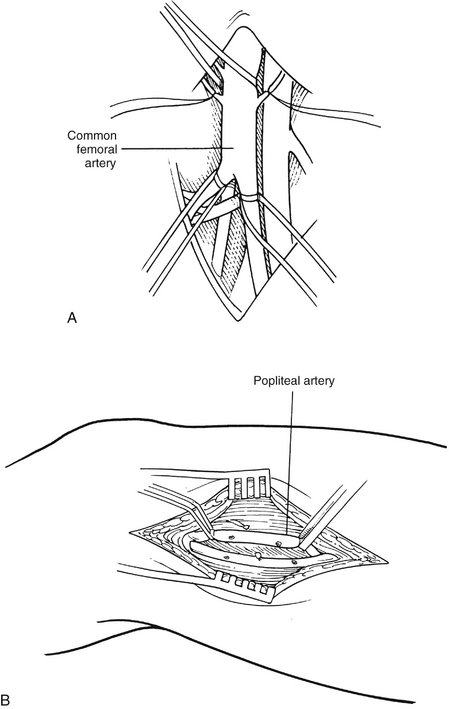
Exposure of the Common Femoral Artery
Exposure of the Popliteal Artery
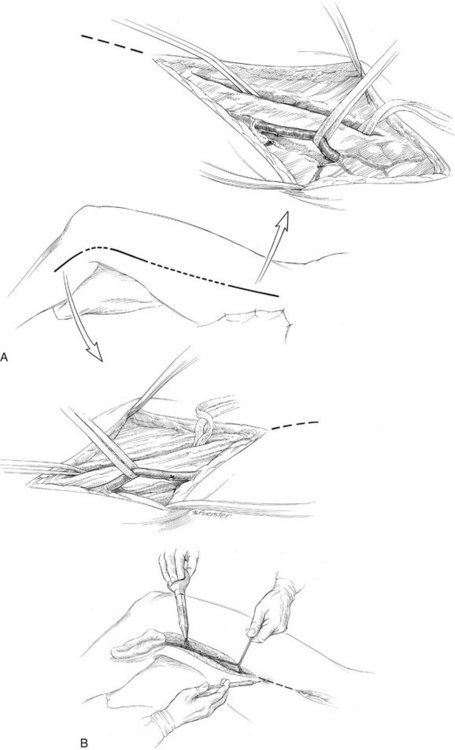
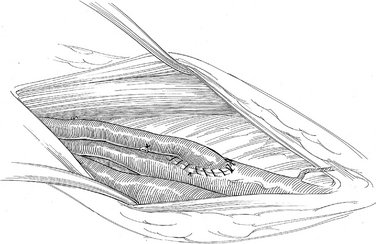
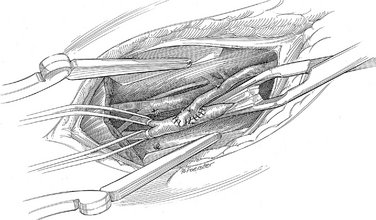
Saphenous Vein Harvest
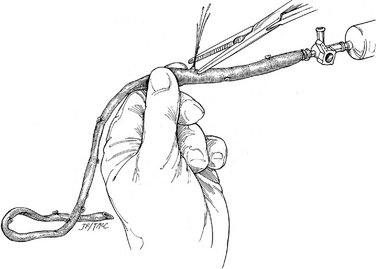
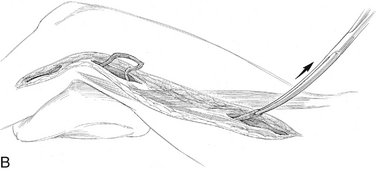
Figure 26-4 Vein graft preparation.
(From Rutherford RB, Ouriel K: Reversed saphenous vein femoropopliteal bypass. In Ouriel K, Rutherford RB: Atlas of Vascular Surgery: Operative Procedures. Philadelphia, Saunders, 1998.)
Construction of the Bypass
POSTOPERATIVE MANAGEMENT
COMPLICATIONS
Freischlag JA, Angle N. Reversed vein bypass [[eds]]. Baker RJ, Fischer JE, editors. Mastery of Surgery, 4th ed. Lippincott Williams & Wilkins, Philadelphia, 2001, 2160-2166.
Ouriel K, Rutherford RB. Reversed saphenous vein femoropopliteal bypass. In: Ouriel K, Rutherford RB, editors. Atlas of Vascular Surgery: Operative Procedures. Philadelphia: Saunders, 1998.
Rosenthal D. Femoropopliteal occlusive disease [[ed]]. Cameron JL, editor. Current Surgical Therapy, 8th ed. Mosby, Philadelphia, 2004, 777-781.