Femoral Hernia Repair
Anatomy
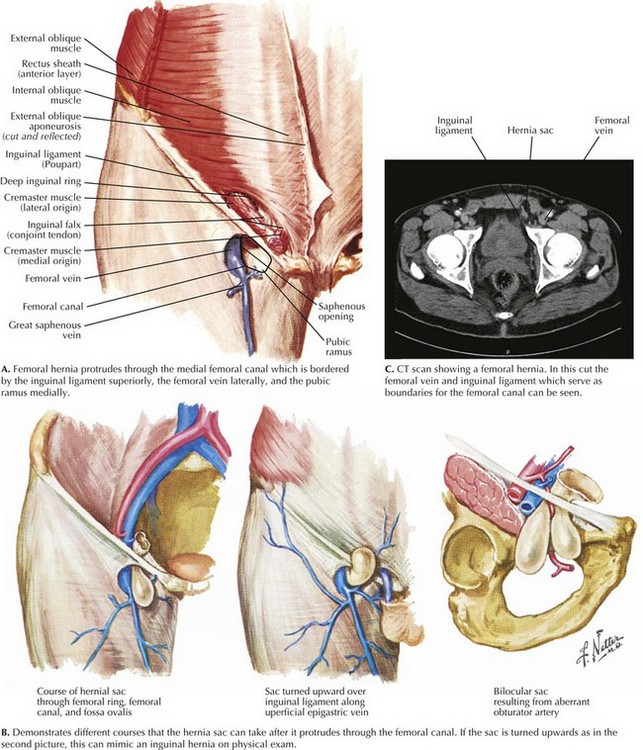
By definition, the femoral hernia protrudes through the femoral canal, bordered by the inguinal ligament superiorly, the femoral vein laterally, and the pubic ramus inferomedially (Fig. 30-1, A). This space is tight and cannot expand, which leads to the high risk of incarceration and strangulation.
Clinical Presentation
The femoral hernia often is seen as an asymptomatic bulge inferior to the inguinal ligament, and as it enlarges, the sac can extend onto the thigh (Fig. 30-1, B). The hernia may or may not be reducible, and patients often report a sensation of fullness. Patients who have incarceration or strangulation often report significant pain, and they may also have evidence of a small bowel obstruction.
Imaging
Additional imaging is not required but can provide useful information, especially when the diagnosis is unclear. Ultrasound or computed tomography (CT) scans can help differentiate between a femoral hernia, inguinal hernia, and inguinal lymphadenopathy (Fig. 30-1, C).
Open Surgical Repair
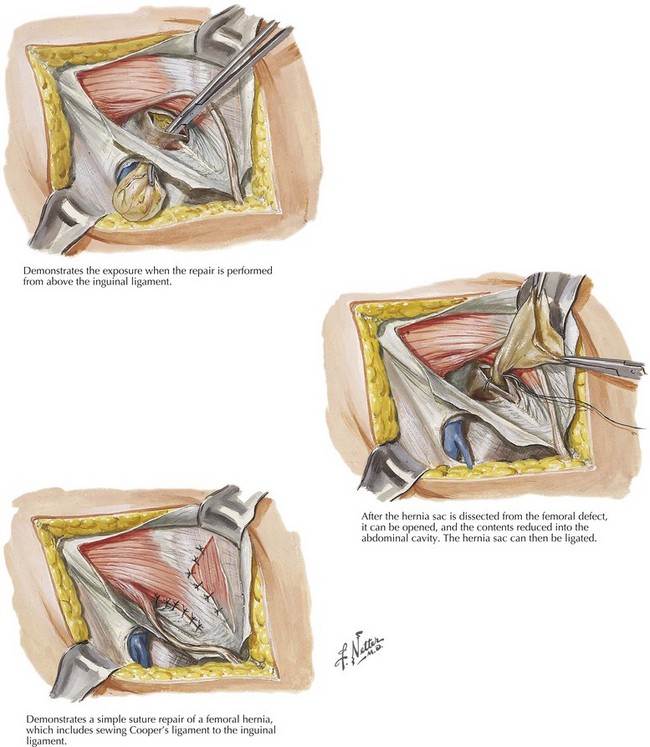
If a patient has signs of incarceration or strangulation, urgent repair is warranted. If the diagnosis of a femoral hernia is confirmed preoperatively, the incision can be placed below the inguinal ligament on the upper thigh. If the etiology of the hernia is uncertain, a standard inguinal hernia incision can be made, with plans to divide the transversalis fascia to expose the femoral space. The dissection can be completed from above the inguinal ligament or below (Fig. 30-2).
Laparoscopic Surgical Repair
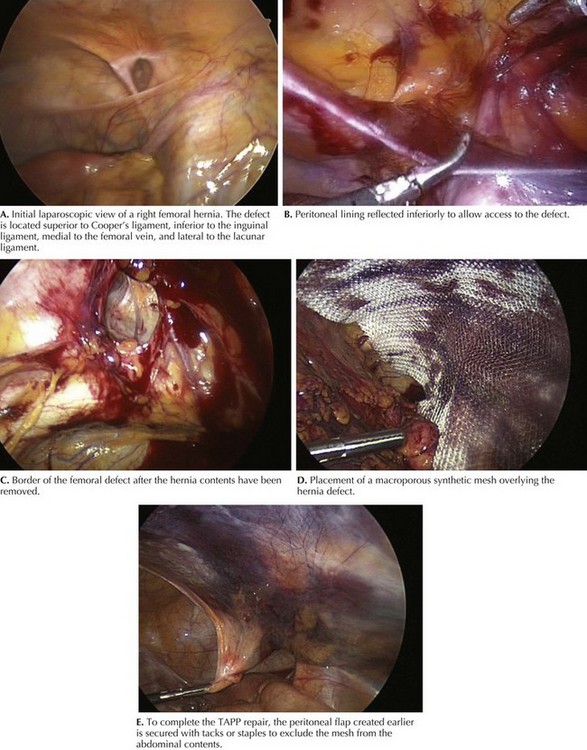
The laparoscopic repair of a femoral hernia is performed in the same manner as that of a standard inguinal hernia (see Chapter 28). Studies have reported both a transabdominal preperitoneal (TAPP) and a total extraperitoneal (TEP) approach for femoral hernia repair. For TAPP repair, traditionally three ports are used. Initial access is obtained at the umbilicus, and the additional working ports are placed to the right and left of midline at the level of the umbilicus. Initial examination reveals the defect near the femoral canal (Fig. 30-3).
Chan, G, Chan, CK. Long-term results of a prospective study of 225 femoral hernia repairs: indications for tissue and mesh repair. J Am Coll Surg. 2008;207(3):360–367.
Dahlstrand, U, Wollert, S, Nordin, P, Sandblom, G, Gunnarsson, U. Emergency femoral hernia repair: a study based on a national register. Ann Surg. 2009;249(4):672–676.
Hernandez-Richter, T, Schardey, HM, Rau, HG, Schildberg, FW, Meyer, G. The femoral hernia: an ideal approach for the transabdominal preperitoneal technique (TAPP). Surg Endosc. 2000;14(8):736–740.
McCormack, K, Scott, NW, Go, PM, Ross, S, Grant, AM. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. (1):2003.