Chapter 79 Far Lateral Approach and Transcondylar and Supracondylar Extensions for Aneurysms of the Vertebrobasilar Junction
Lesions of the anterior and anterolateral brain stem present special challenges to the neurologic surgeon. Unlike the posterior surface of the brain stem, the anterior surface is buried deep within several vital structures precluding easy anterior access. For this reason, lateral approaches have been proposed to access the anterolateral surface of the lower brain stem from a posterior incision. Heros1 first described extensive removal of the lateral foramen magnum up to the condyle to approach these lesions. Later authors advocated progressive drilling of bony structures lateral to the foramen magnum such as the occipital condyle, jugular tubercle, atlanto-occipital joint, and mastoid. As each lateral structure is removed, the angle of approach to the anterolateral surface of the brain stem is increased and the surgical corridor widened. However, morbidity from damage to the vertebral artery (VA) and cranial nerves as well as frank instability of the craniocervical junction is also increased with each structure removed.
Anatomy
Muscular Anatomy
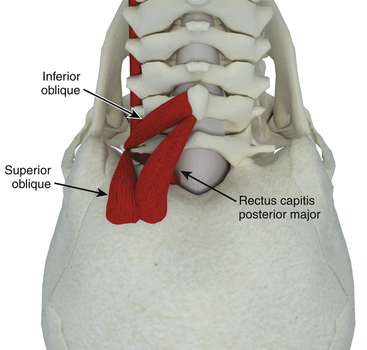
Despite our belief that separation of each individual muscle layer is unnecessary for the far lateral approach, an understanding of the upper cervical muscles and their attachments is an important aspect of performing the far lateral approach safely. The key to the exposure of the far lateral approach lies in the identification and preservation of the extradural vertebral artery, which lies within a triangle of muscles referred to as the suboccipital triangle (Fig. 79-1).
Extradural Anatomy
Three specific points regarding the extradural VA deserve mention. First, as it courses medially in the sulcus arteriosus, it may loop cranially near the occipital bone. This must be kept in mind during the muscular stage of the exposure—it is surprisingly easy to inadvertently bovie into the artery when attempting to separate the last bit of cervical musculature off the suboccipital region. Second, while the posterior inferior cerebellar artery (PICA) usually arises from the VA intradurally, in approximately 5% to 20%2 of specimens it arises extradurally and can be confused with a muscular branch off the VA. Third, the VA sits in a venous plexus as it courses in the sulcus arteriosus, which often leads to troublesome bleeding if one chooses to expose it.
An interesting anatomic study quantified the benefit of removing these two structures in terms of visualization and surgical freedom.3 The authors found that removing the occipital condyle up to the hypoglossal canal resulted in a mild improvement (21% to 28%) in visualization but a much larger improvement (18% to 40%) in surgical freedom (ability to manipulate surgical instruments within that space). Resection of the jugular tubercle on the other hand, had the opposite effect with a dramatic increase (28% to 71%) in visualization but only a modest (40% to 52%) increase in surgical freedom. This emphasizes the role the occipital condyle plays in narrowing the surgical spatial cone through which instruments are manipulated.
Surgical Technique
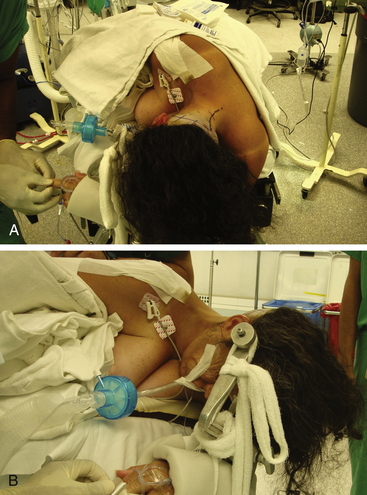
Various positions can be used including supine with the head rotated, lateral or half-lateral decubitus, and a three-quarter prone or park-bench position. At our institution we prefer a straight lateral position. The patient is placed on the operating table with the side of the lesion placed upward. The dependant arm hangs off the bed and is cradled in a padded sling between the table edge and the Mayfield head holder. The head is then secured in a three-pin Mayfield head clamp. Pin placement is crucial if an occipital artery bypass is contemplated as it may hinder the procedure if placed improperly. The pins are placed so that the single pin is 2 cm superior and anterior to the ear pinna ipsilateral to the lesion. The paired pins are positioned so that the posterior pin is 2 cm above the contralateral ear pinna. The head is positioned with three or four movements:
1. Flexion in the anteroposterior plane with slight distraction until the chin is two finger breadths from the clavicle uncovers the suboccipital region.
2. Contralateral bending (approximately 30 degrees) increases the surgical space between the ipsilateral shoulder and the suboccipital region.
3. Upward translation partially and subtly subluxes the ipsilateral atlanto-occipital joint and facilitates possible condylar drilling.
4. Contralateral head rotation in order to bring the ipsilateral side uppermost in the surgical field. Although some authors have advocated this manuever,4 the senior author (RCH) believes that this maneuver is not advisable as it results in rotation of the ventral surface of the brain stem and thus the vertebrobasilar junction away from the surgeon. In fact, upon completion of the bony drilling and opening of the dura, we routinely rotate the operating table toward the surgeon to allow a tangential view of the ventral brain stem. The operating table is placed in slight reverse Trendelenberg so as to position the patient’s head above the level of the heart to reduce cerebral venous congestion. The patient’s superior shoulder is retracted towards the patient’s feet using adhesive tape to keep the cervical-suboccipital angle open (Fig. 79-2).
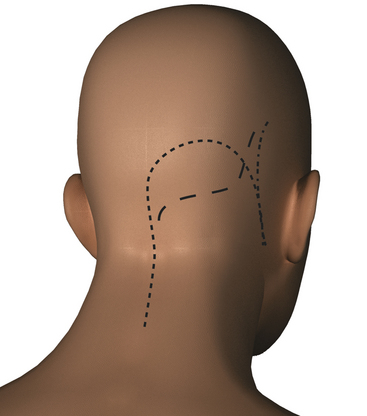
The surgical site is shaved. If the occipital artery is to be harvested, a portable Doppler probe is used to identify the course of the artery over the scalp from the mastoid to approximately 4 cm above the superior nuchal line. In such cases scalp infiltration solutions containing vasoconstrictive agents should not be used. The scalp is then prepped and draped in a standard fashion. Several skin incisions may be used including a linear or curvilinear retromastoid, S-shaped, or hockey-stick incision (Fig. 79-3). The linear or curvilinear retromastoid incision starts at about the level of the top of the ear approximately three finger-breadths medial to the mastoid process and extends straight down or a as a gentle curve to just below the mastoid tip. The S-shaped incision starts from the same point described above; however after an initial extension of the incision straight down toward the mastoid, the incision is curved sharply medially to the midline, and then straight downward to the spinous process of C3.
The hockey-stick incision, which is currently preferred at our institution, is carried through the midline aponeurosis with minimal injury to the muscle mass and allows early identification of the spinous processes and lamina of C1 minimizing the risk of injury to vertebral artery. Superolaterally the muscle mass is cut along its attachment to the superior nuchal line leaving a small cuff of muscle and fascia for better anatomic closure. The main disadvantage to this incision is that the bulk of the musculature is retracted laterally. Since the angle of attack is lateral to medial, this can hinder access to the atlanto-occipital joint or obstruct the surgical view from an inferior direction under the cerebellar tonsil if not adequately retracted. The hockey-stick incision starts approximately at the level of the spinous process of C3 and extends superiorly in the avascular midline plane to approximately 2 cm above the superior nuchal line. The incision is then turned laterally parallel to the superior nuchal line. If the occipital artery is to be harvested, a curved hemostat is used to dissect over and protect the artery. The incision is then continued over the occipital artery to a point immediately superior to the mastoid process. Finally, the incision is curved inferiorly to end just inferior to the mastoid tip (Fig. 79-4).

FIGURE 79-4 The skin incision is shaped like a hockey stick spanning the midline and extending to the mastoid tip.
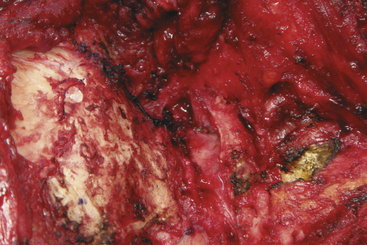
The suboccipital muscles are cut leaving a cuff as stated above. This facilitates tight muscle closure at the end of the procedure and minimizes postoperative cerebrospinal fluid leaks. This is particularly important if an occipital artery bypass is to be performed as a watertight dural closure is not possible because of the necessity of creating an opening for passage of the occipital artery. The suboccipital musculature is then swept laterally in a subperiosteal fashion to expose the occiput as far laterally as the mastoid process as well as the arch of C1. The skin and muscle flap are retracted inferolaterally and held in position by fishhooks (Fig. 79-5). Adequate retraction of the cervical musculature is important (particularly if a hockey-stick incision is used) to avoid negating the advantage of a more lateral angle of vision achieved with the far lateral approach. An alternative method of layer-by-layer muscle dissection from lateral to medial has been described to avoid this problem.5 The technique consists of cutting the muscles in layers leaving small cuffs of the sternomastoid, splenius capitis, and semispinalis muscle attached to the bone for later reattachment. The muscle mass is then elevated medially.
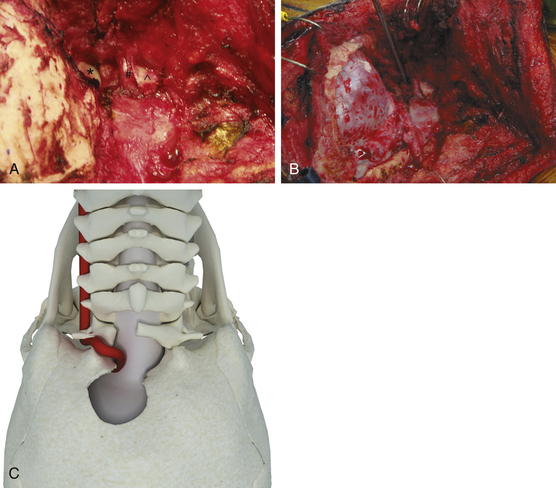
Basic Far Lateral Approach
The basic far lateral approach consists of a suboccipital craniotomy and lateral removal of the bony rim of the foramen magnum up to the occipital condyle, which is left intact. The suboccipital craniotomy is performed extending from the junction of the transverse and sigmoid sinuses superiorlaterally to just beyond the midline through the foramen magnum in a teardrop fashion. After the suboccipital craniotomy has been accomplished, the arch of C-1 is removed from just beyond the midline on the opposite side to the sulcus arteriosus underlying the vertebral artery (Fig. 79-6).
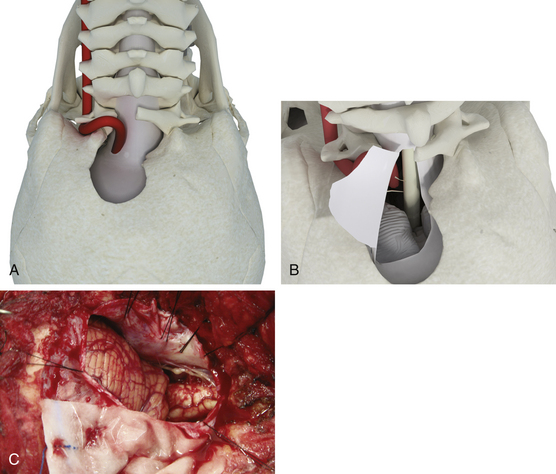
Transcondylar Extension
The basic far lateral approach may be extended more laterally by resection of posterior aspect of the occipital condyle. This transcondylar approach allows a more lateral direction of view than that offered by the basic far lateral approach, thus providing improved exposure of the lower clivus and anterolateral medulla (Fig. 79-7).
Supracondylar Extension
The supracondylar extension of the far lateral approach involves removal of the bone above the occipital condyle, specifically the jugular tubercle. This allows further visualization of the anterolateral surface of the brain stem. Extensive drilling of the bone below and above the hypoglossal canal allows transposition of the hypoglossal nerve. The supracondylar approach permits access to the clivus as well as the region medial to the hypoglossal canal. However, the jugular tubercle that lies above and anterior to the hypoglossal canal may obstruct visualization of the basal cisterns and the clivus anterior to the lower cranial nerves. The trans-tubercular variant of the supracondylar approach involves drilling of the jugular tubercle so that the dura covering the prominence can be pushed forward to gain access to the front of the medulla and pontomedullary junction. This is particularly useful for PICA aneurysms in patients in whom the PICA originates from the upper segment of the vertebral artery. Practically speaking, drilling the tubercle extradurally can be challenging because of the distance around the occipital bone one has to reach. One option is to shell out the tubercle extradurally, leaving a rim of cortical bone medially. Upon opening the dura, this shell of tubercle can be cracked laterally into the space created by the drilling. The other option is to drill the tubercle intradurally. This involves cutting the overlying dura and drilling the bone underneath, analogous to intradural anterior clinoid removal. The drilling is directed between the 10th and 11th nerves.
Complications
Extensive removal of the occipital condyle or C1 lateral mass may potentially result in atlanto-occipital instability. In a biomechanical study, it was found that occipito-cervical mobility increased significantly as compared to baseline after removal of half of the occipital condyle.6 A craniocervical fusion should therefore be strongly considered if greater than 50% of the occipital condyle is resected. As mentioned above, this extensive condylar resection is rarely indicated for vascular lesions.
Conclusion
The basic far lateral suboccipital approach that we routinely extend by removing the posteromedial one fourth to one third of the occipital condyle provides an excellent surgical exposure that is adequate for managing almost all aneurysms of the intracranial portion of the vertebral artery, the proximal PICA, and the vertebral basilar junction. This approach, of course, is also excellent for many extra-axial tumors of this region, particularly meningiomas of the anterolateral rim of the foramen magnum. Intra-axial lesions of the anterolateral cervical medullary region can also be approached comfortably with this exposure. More complex exposures such as the transcondylar and supracondylar extensions are rarely required for vascular lesions, but can be quite useful for some complex extra-axial tumors of this region. The main complication specifically related to the cervical approach is injury to the vertebral artery or to the PICA when it has an extradural origin. This can be avoided by detailed knowledge of the anatomy and its variances and careful sharp dissection in the region of the vertebral artery. Intradural complications, which include not only vascular injuries but also injury to the lower cranial nerves, are usually related to the specific pathology, rather than to the surgical approach.
Babu R.P., Sekhar L.N., Wright D.C. Extreme lateral transcondylar approach: technical improvements and lessons learned. J Neurosurg. 1994;81:49-59.
Fine A.D., Cardoso A., Rhoton A.L.Jr. Microsurgical anatomy of the extracranial-extradural origin of the posterior inferior cerebellar artery. J Neurosurg. 1999;91:645-652.
Heros R.C. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559-562.
Lanzino G., Paolini S., Spetzler R.F. Far-lateral approach to the craniocervical junction. Neurosurgery. 2005;57:367-371.
Spektor S., Anderson G.J., McMenomey S.O., et al. Quantitative description of the far-lateral transcondylar transtubercular approach to the foramen magnum and clivus. J Neurosurg. 2000;92:824-831.
Vishteh A.G., Crawford N.R., Melton M.S., et al. Stability of the craniovertebral junction after unilateral occipital condyle resection: a biomechanical study. J Neurosurg. 1999;90:91-98.
1. Heros R.C. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559-562.
2. Fine A.D., Cardoso A., Rhoton A.L.Jr. Microsurgical anatomy of the extracranial-extradural origin of the posterior inferior cerebellar artery. J Neurosurg. 1999;91:645-652.
3. Spektor S., Anderson G.J., McMenomey S.O., et al. Quantitative description of the far-lateral transcondylar transtubercular approach to the foramen magnum and clivus. J Neurosurg. 2000;92:824-831.
4. Lanzino G., Paolini S., Spetzler R.F. Far-lateral approach to the craniocervical junction. Neurosurgery. 2005;57:367-371.
5. Babu R.P., Sekhar L.N., Wright D.C. Extreme lateral transcondylar approach: technical improvements and lessons learned. J Neurosurg. 1994;81:49-59.
6. Vishteh A.G., Crawford N.R., Melton M.S., et al. Stability of the craniovertebral junction after unilateral occipital condyle resection: a biomechanical study. J Neurosurg. 1999;90:91-98.