CHAPTER 6 Facelift anatomy, SMAS, retaining ligaments and facial spaces
Anatomically correct facial rejuvenation surgery is the basis for obtaining natural appearing and lasting results. The complexity of the anatomy of the face, and especially that of the midcheek, accounts for the formidable reputation of facial surgery. This is to the extent that many surgeons design their rejuvenation procedures around an avoidance of anatomical structures, and thereby limit the intent to camouflaging of the aging changes.
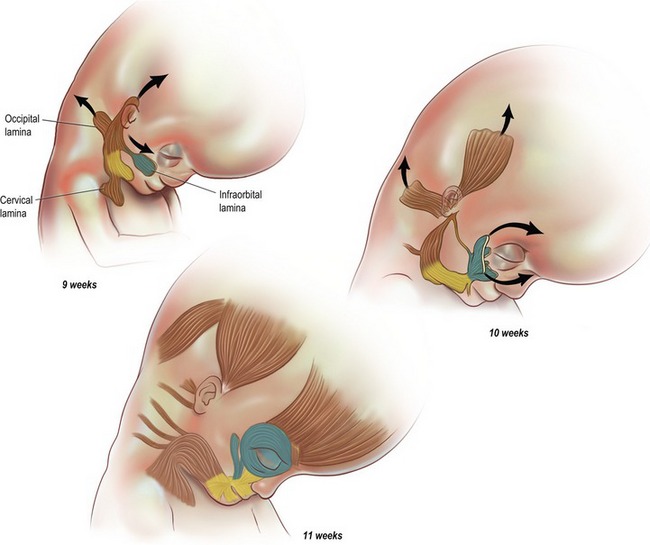
Functional evolution of the face
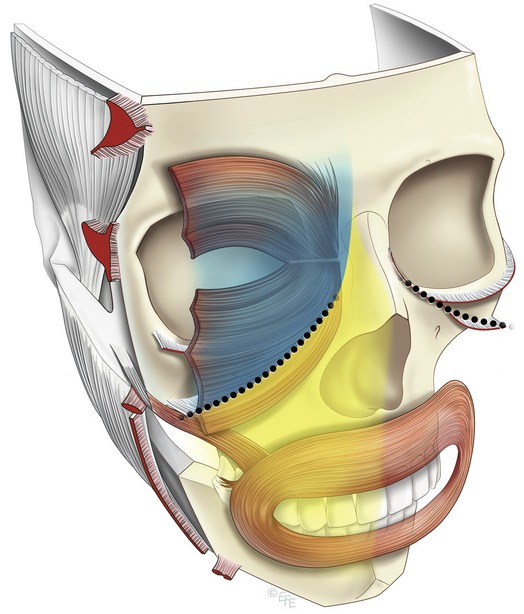
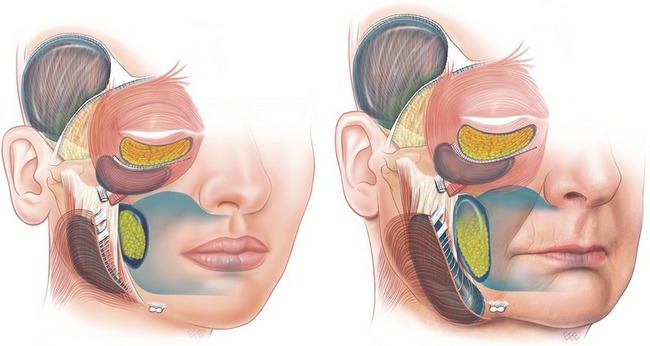
The anatomy of the face is more readily understood when considered from the perspective of its evolution and the function of its components (Fig. 6.1). Located at the front of the head, the face provides the mouth and masticatory apparatus at the entrance to the embryonic foregut, as well as being the location for the receptor organs of the special senses: eyes, nose and ears. The skeleton of the face incorporates a bony cavity for each of these four structures. Those for the special senses have a well-defined bony rim, in contrast to the articulated broad opening of the jaws covered by the oral cavity. The soft tissues of the face, integral to facial beauty and attraction, are in reality, dedicated entirely to their functions.
Regions of the face
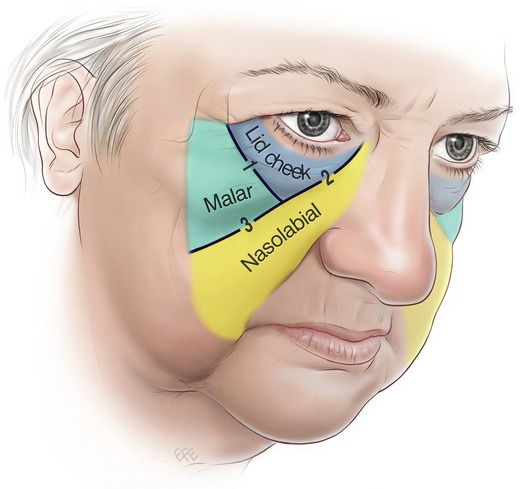
The traditional approach to the face in thirds (upper, middle and lower) while useful, limits conceptualization, as it is not based on the evolving structure. The significant muscles of facial expression are all located on the front of the face (anterior aspect) predominantly around the eyes and mouth, where their effect is seen in communication. For these functional reasons the anterior aspect of the face contains the more delicate expressive areas, which are prone to developing aging changes (Fig. 6.2).
In contrast, the lateral face is relatively immobile as it passively overlies the structures to do with mastication, which are all deep to the investing deep fascia. These are the temporalis and masseter on either side of the zygomatic arch, along with the parotid and its duct. The only superficial muscle in the lateral face is the platysma in the lower third, which reaches no higher than the oral commissure. Internally, a distinct boundary separates the mobile anterior face from the lateral face. The vertically oriented line of retaining ligaments attached to the facial skeleton forms this boundary (Fig. 6.2).
From the perspective of priorities in rejuvenation surgery, the midcheek is the most important area of the face, because of its prominent central location between the two facial expression centers, the eyes and the mouth. The periorbital and the perioral parts overlap in the midcheek (Fig. 6.2). The periorbital part overlies the body and orbital process of the zygoma, while the perioral part overlies the maxilla, a bone of dental origin. The functional parts are inherently mobile and meet at the relatively immobile boundary that extends in an oblique line across the midcheek. This is the midcheek groove formed by the dermal extensions of the zygomatic ligaments (Fig. 6.3).1
The facial nerve in relation to regions of the face
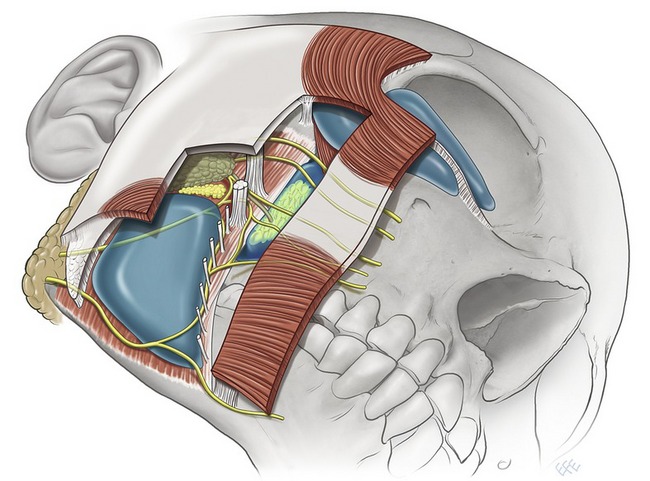
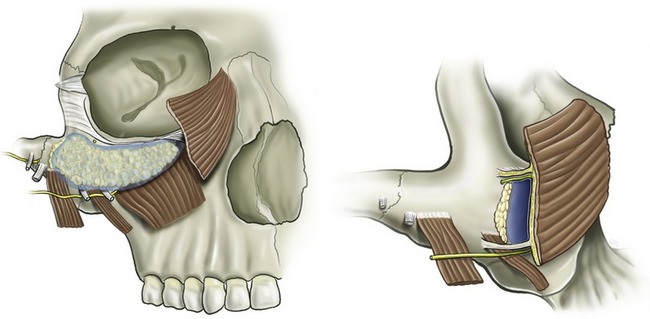
The level in which the facial nerve branches travel relates to the region of the face (Fig. 6.4). In the lateral face below the zygomatic arch the branches remain deep to the investing deep fascia. In the anterior face (and above the lower border of the zygoma) the branches are more superficial in relation to their muscles. The transition in levels occurs at the retaining ligament boundary, which is the last position of stability before the mobile anterior face. The nerves are protected here as they course outward to their final destination
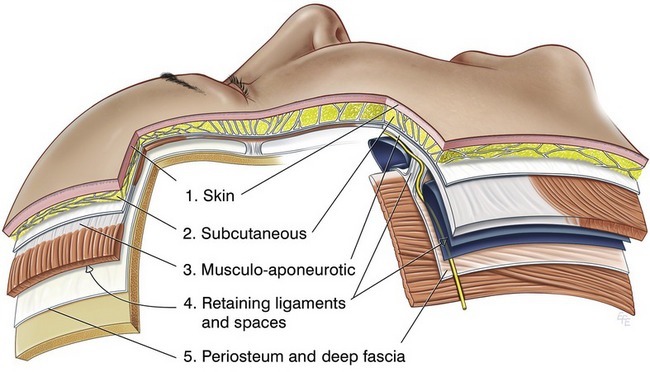
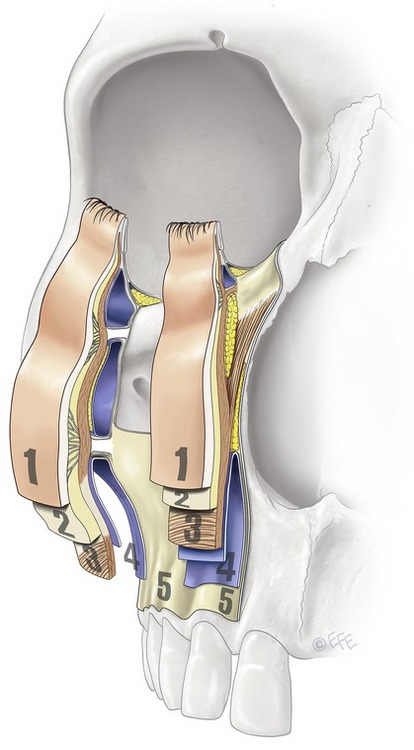
Fig. 6.4 The layers of the face. The five layers of the scalp are a prototype of facial anatomy and the simpler basis for the more complex structure elsewhere on the face. Layer 4 is the most changed layer, consisting of alternating spaces and ligaments. The course of the facial nerve changes level at the ligamentous boundary transition from the lateral to the anterior face. Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek: facial layers, spaces, and the midcheek segments; Clin in Plast Surg 2008;35:395–404.
Layers of the face
The principles of facial structure can be summarized quite simply:
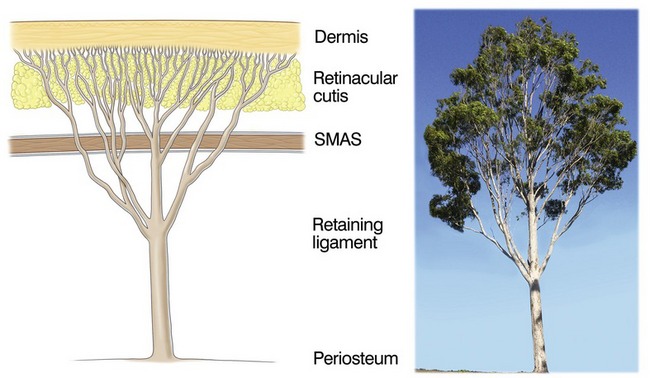
1. The scalp is the basic prototype for understanding facial anatomy, as it is the least differentiated part of the face (Fig. 6.4).
2. The face is constructed of concentric soft tissue layers over the bony skeleton.
3. The five layers of the scalp are: (i) skin; (ii) subcutaneous; (iii) musculo-aponeurotic; (iv) areola tissue; (v) deep fascia.
4. The layers are not homogenous over the face proper, as they are modified in areas of function.
5. The key areas of function overlie the bony cavities, especially the eyelids and the cheeks and mouth.
6. A multilinked fibrous support system supports the dermis to the skeleton (Fig. 6.5). The components of the system pass through all layers.2
7. At the transition between that over the skeleton to that overlying the cavities (eyelids and mouth) there is a modification of the anatomy.
8. The complexity of the facial structure results from the balance required between mobility and stability (ligamentous support).
Details of the layers
Layer one – skin
The structural collagen of the dermis is the outermost part of the fibrous support system and is intrinsically linked, both embryologically and structurally, with the collagenous tissue of the deeper layers. The thickness of the dermal collagen relates to its function, and tends to be in inverse proportion to its mobility. The dermis is thinnest on the eyelids and thickest on the forehead and nasal tip. The thinner, more mobile dermis is susceptible to an increased tendency for aging changes.
Layer two – subcutaneous
Each of the three midcheek segments has a distinctly different thickness of subcutaneous fat. The subcutaneous layer is thinnest in the lid–cheek segment adjacent to the lid proper. In the malar segment the layer is moderately thick and uniform, whereas it is markedly thicker in the nasolabial segment, which has the thickest layer of subcutaneous fat of the face. Where the subcutaneous fat is thicker, the retinaculum fibers are lengthened and more prone to weakness and distension. The thick subcutaneous fat in the nasolabial segment is named the malar fat pad, which is confusing terminology given that its position is predominately medial to the prominence of the zygoma in the perioral part of the midcheek3,4 (Fig. 6.2).
Within the subcutaneous layer, the attachment to the overlying dermis is stronger than on its deep surface, due to the tree-like arrangement of the retinacular cutis fibers (Fig. 6.5). In superficial, i.e. subdermal, dissection of the subcutaneous layer, many fine retinacula cutis fibers are encountered. At the interface with the underlying layer 3, there are fewer, though larger fibers and less subcutaneous fat, which appears not to descend fully to the interface where it overlies the superficial muscles, orbicularis oculi and platysma.
The retinacular fibers are not uniform across the face, but vary in their orientation and arrangement according to the region. This variation mirrors the anatomy of the underlying 4th layer. As will be more apparent when the 4th layer is discussed, the line of retaining ligaments continue vertically through the subcutaneous layer to form septae, that form boundaries which compartmentalize between more mobile areas.5 Accordingly, where the subcutaneous layer overlies spaces (in the 4th layer) there are no vertically oriented subcutaneous ligaments extending through. In contrast, the retinacular fibers overlying the spaces have a predominantly horizontal orientation, being in strata-like layers that are less restrictive to underlying movement.
Layer three – musculo-aponeurotic
In the prototype scalp, the third layer demonstrates key principles about the facial muscles. The superficial muscle, occipito-frontalis, moves the overlying soft tissues including the skin of the scalp and forehead. While the muscles have a minimal area of bony origin, which is remote (on the superior nuchal line), they have an extensive area of insertion into the overlying soft tissues.
The fibrous sheath enclosing the frontalis and occipitalis is continuous across the entire scalp, whereas the enclosed muscles are discontinuous. Where the fascia is present without intervening muscle, the superficial and deep layers of the sheath are apposed and fused to form the galea aponeurotica. This is the basis for the aponeurotic part of the 3rd layer. The superficial fascial layer is thin where it overlies the muscle, and in areas such as over the forehead, muscle fibers extend into the subcutaneous layer. In contrast, the deep layer of the fascia is thicker, more supporting and provides a gliding surface at the interface with the underlying 4th layer. The original description of the SMAS (superficial muscloaponeurotic system) in 1976 was essentially a description of this 3rd layer, as is applies to the mid and lower thirds of the face.6 The flat superficial muscle component predominates in some areas of layer 3, while in areas without muscle the aponeurotic element predominates.
The definitive muscles in level 3 have a layered arrangement. The broad flat muscles form the superficial layer that covers the anterior aspect of the face: frontalis overlies the upper third and orbicularis oculi the middle third. The platysma, over the lower third extends onto the lateral face, presumably related to jaw movement, which functionally dominates the lower third. The superficial muscles are more closely related to the overlying subcutaneous layer than they are to the deeper structures. The superficial flat muscles have a minimal direct attachment to the bone. They are indirectly stabilized to the skeleton by a ligament, located at the lateral border of the muscles. The frontalis is fixed by the superior temporal ligament along the superior temporal line, the orbicularis oculi is stabilized by the main zygomatic ligament at its inferolateral border and the platysma is stabilized at its upper border by the upper key masseteric ligament (Fig. 6.15).
Layer four
The following structures are contained within layer 4, but each is distributed in different areas:
1. Retaining ligaments of the face.
2. The deep layer of the intrinsic muscles.
• Overlying the skeleton, layer 4 is essentially composed of a series of ‘spaces’ and non-mobile areas of important anatomy.
• The spaces are mobile functional areas. Each space has a definite boundary and minimal fixation.
• The boundaries tend to be the least mobile part of the soft tissue.
• The retaining ligaments are located within and reinforce the boundaries that separate the different functional areas.
• The intrinsic muscles of the deeper layer attach to the bone within the boundaries.
• Superficially, the muscles insert into the mobile soft tissues in layer 3, in the area of maximum mobility.
• All the deep muscles of clinical significance attach to the bony border of the oral cavity.
• The retaining ligaments and muscle origins share a bony origin at the boundary.
• A line of ligamentous attachment continues around the perimeter of the bony cavities.
1. Spaces provided by the bony cavities; the preseptal and conjunctival spaces of the eyelids within the orbit and the vestibule of the oral cavity beneath the lips and the nasolabial segment of the cheeks.
2. Soft tissue spaces overlying the facial skeleton between the bony cavities. The series of tissue spaces between level 3 and level 5 are voids in the attachment of the mobile soft tissues to the underlying skeleton.
The significance of the spaces is only now becoming appreciated. The spaces are not only essential for function; their presence explains much about the changes that occur with facial aging. The appearance with aging of malar mounds, jowls and labiomandibular folds is due entirely to changes of previously unrecognized facial soft tissue spaces.7
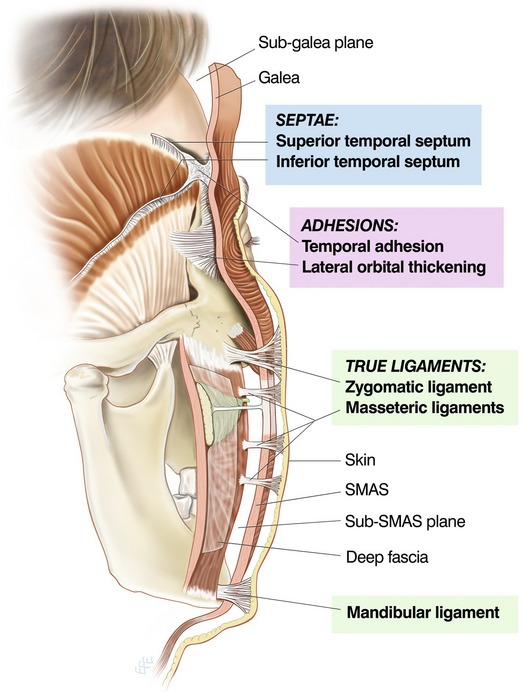
Retaining ligaments of the face
The retaining ligaments of the face are located in specific locations.8,9 These are in between areas of movement (spaces). The trunks of the ligaments pass out through layer 4 as part of the multilinked fibrous support system.2,10 These structures were not originally thought of as being ligaments as they are not part of the musculoskeletal system and do not have the typical appearance of ligaments, such as the cruciate ligament. However, a ligament is, by definition, a fibrous structure that binds or ties adjacent structures. The soft tissue ligaments take varied forms consistent with the functions of the face.
The lateral face immediately in front of the ear is not a mobile area. This zone of no movement extends forward of the ear cartilage for 25 to 30 millimeters due to an important, but little appreciated, area of ligamentous attachment the platysma auricular fascia (PAF).11 The PAF is unique because it is two layers formed into one structure. It consists of a diffuse area of layer 4 ligament that binds the SMAS with the underlying parotid masseteric fascia and parotid capsule. It includes the part of the SMAS (layer 3) between the ear cartilage and posterior border of the platysma. It is both part of the SMAS (layer 3) as well as ligament (layer 4). The retinacular cutis overlying the PAF is ‘dense’ because it does not overlie a space. Forward of the anterior border of the PAF where the platysma is present, the soft tissue layers are mobile.
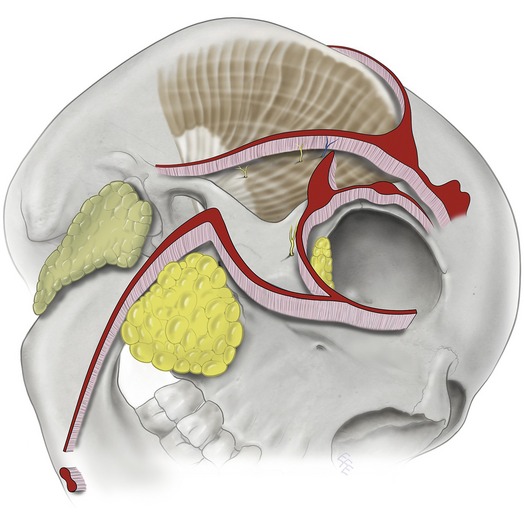
Sub-SMAS facial spaces
The sub-SMAS layer 4 is largely composed of ‘spaces’.7 These intervals have defined boundaries and in the boundaries are located the retaining ligaments. The spaces are by definition safe spaces, because there are no structures within and no structures cross through the spaces. This is important for the surgeon, as all facial nerve branches are outside the spaces. Because spaces allow movement, laxity develops more of the space than occurs in the ligamentous boundaries. This differential laxity accounts for much of the characteristic changes of aging.
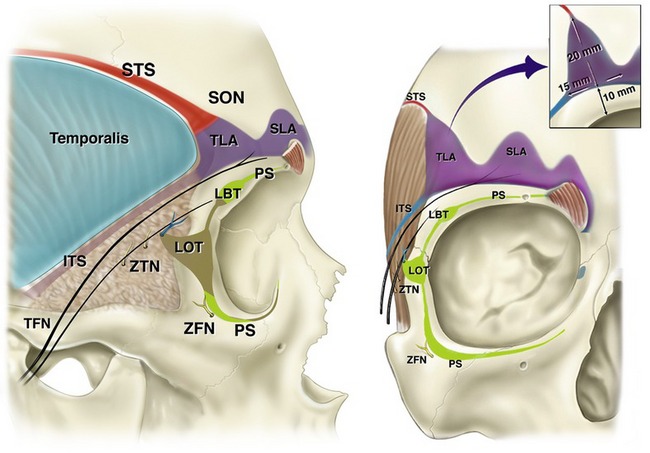
The ligamentous boundary that separates the forehead space from the upper temporal space is the superior temporal septum, which originates along the superior temporal line (the zone of fusion).8 Within the temple a second fibromembranous ligamentous structure, the inferior temporal septum, crosses the outer surface of the deep temporal fascia and separates the upper temporal space from a lower triangular-shaped zone containing detailed temporal anatomy. The superior temporal septum and the inferior temporal septum meet at the respective corners of the triangular-shaped temporal ligament (also called orbital),12 an area of ligamentous adhesion to the underlying periosteum and adjacent deep temporal fascia (Fig. 6.11).13
The prezygomatic space overlies the prominence of the body of the zygoma and allows displacement of the orbicularis oculi, pars orbitale, in its roof (Fig. 6.12).14
The triangular-shaped space correlates with the shape of the bony platform and is bounded above by the orbicularis retaining ligament and inferomedially by the line of zygomatic ligaments. Contraction of the overlying muscle results in visible zygomatic smile lines inferior to the horizontal crows feet lines. With aging laxity of the roof these zygomatic lines become increasingly prominent and may eventually be present at rest. Further laxity may result in a bulge of the roof of the space at rest, the so-called malar mounds, or malar bags (also called malar crescent). The presence of these changes indicates laxity of the orbicularis for which tightening is the treatment. When operating in the prezygomatic space it is logical and inherently safer to use blunt dissection with an appropriate surgical instrument, or finger.15
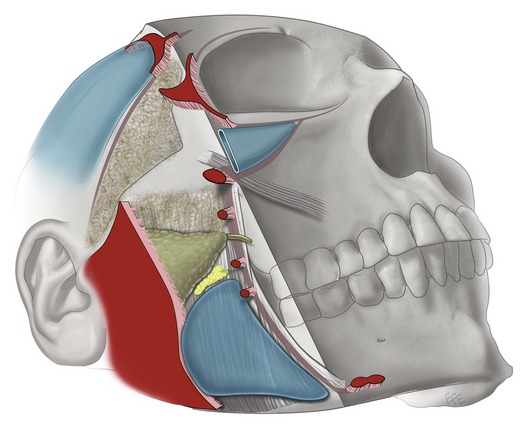
The premasseter space in the lower third of the lateral face is analogous with the temporal space in overlying the deep fascia of a muscle of mastication.10 Opening of the jaw without restriction from the overlying soft tissue requires that movement of the soft tissues be provided by the premasseter space. Eventually, laxity develops in the platysma roof of the space and its attachment along the inferior and anterior boundaries leading to the bulging that forms the jowl and the labiomandibular fold (Fig. 6.13).
The masticator space (also called the buccal space because of its content, the buccal fat pad) is different in character being on the anterior face (Figs 6.7, 6.13). It underlies the midcheek medial to the masseter. Similar to the oral cavity, the masticator space facilitates movement of the overlying nasolabial segment of the midcheek. Aging results in weakness of support of the boundaries and roof especially from attrition of the masseteric ligaments. As a result, the platysma becomes less closely bound to the masseter, allowing the masticator space to bulge inferiorly below the level of the oral commissure and into the lower face (Fig 6.15). With major descent, the buccal fat comes to overlie the anterior border of the lower masseter, such that the fullness of the displaced fat increases the prominence of the labiomandibular fold.
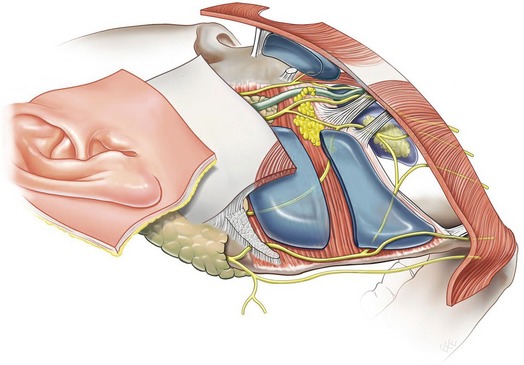
Areas of important anatomy
Over the lateral face, on either side of the zygomatic arch, are two similar areas containing important anatomy (Fig. 6.9). These have not been specifically mentioned in the surgical literature, so for purposes of description they are named here as the lower temporal and upper masseteric areas of important anatomy, as they are neither spaces nor ligaments. By definition they are not spaces, as they contain anatomical structures and are not lined by membrane. They both have soft fat protecting their contents, and can be gently opened, like a space using precise dissection.
The lower temporal area of important anatomy between the upper temporal space and the arch is the passageway from the lateral face into the upper third (Fig. 6.11). The temporal branches of the facial nerve are suspended from the roof in a wafer-like strata of protective fat, immediately inferior to the inferior temporal septum. The contents, which cross the area from deep to superficial, include both zygomatico-temporal nerve branches and the sentinel vein.
Careful dissection in this area may be required to access the lateral zygomatic and upper masseteric ligaments.
Facial nerve branches
Clinical correlation
The facial nerve branches are ‘at greatest risk’ where they transverse layer 4 to access layer 3. The nerves cross this level in predictable locations, in relation to the vertical ligamentous line defining the lateral face/anterior face transition where they are under the protection of the retaining ligaments (Figs 6.4, 6.7).
The temporal and mandibular branches are the most important facial nerve branches in terms of surgical risk. The temporal branches gain the underside of layer 3 immediately on leaving the parotid, inferior to the zygomatic arch. These branches course within a wafer-like layer of fat contained in a fibrous envelope suspended from the underside of the temporal SMAS, as they course over the arch and the lower temporal triangle, where they are immediately inferior to the inferior temporal septum (Fig. 6.11). The temporal branches can be safely avoided by maintaining the plane of dissection directly on the outer surface of the deep temporal fascia and avoiding compression neurapraxia from retractor pressure.
The mandibular branches are at risk where they are fixed by having a close relationship to ligament. Initially, this is within the PAF, and then well anteriorly by the mandibular ligament (Fig. 6.13). Over most of its course, where it is in relation to the premasseter space, the nerve is mobile. The absence of retaining ligaments along the mandible between the PAF and the mandibular ligament allows an inherent mobility of the tissue. For this reason, it is not necessary to dissect in the immediate vicinity of the mandibular branch in order to correct laxity of the platysma overlying the jaw and submandibular triangle.
Layer five
Over the lateral face the muscles of mastication largely conceal the skeleton and here the deep fascia equivalent is the deep temporal and masseteric fascia, which also provide attachment for retaining ligaments. The investing layer of deep cervical fascia is the corresponding layer in the neck. The deep fascia is traditionally taken to be the deep boundary of the territory for aesthetic surgery. However, in recent times this boundary is transgressed for subperiosteal ‘lifting’ and for bone contouring procedures. In the neck it is incised for access to the deeper located submandibular gland.
1. An overcorrection is required to compensate for the ‘lift lag’ phenomenon. This is to compensate for the accumulated aging changes throughout the entire ligamentous support system to the dermis, in order to transmit sufficient effect to obtain the desired changes of shape and tone to the skin.
2. There is inherently more benefit from subperiosteal lifting where the overlying soft tissue layers are more tightly attached. This occurs overlying the skeleton, but is less so over the bony cavities as there is no periosteum in the eyelid or the mobile part of the cheek.
3. Because of the unyielding nature of periosteum, an extensive undermining is needed beyond the immediate area for intended correction. The alternative is to perform a ‘periosteal release’, that is to incise the periosteum at the boundary. This boundary release is commonly performed along the superior orbital rim and less consistently along the boundary with the lateral face.
Anatomy over the cavities in the skeleton
The layered anatomy, as described over the lateral aspect of the face, is modified where the orbital and oral cavities are present over the anterior face (Fig. 6.1). The gaps in the bone surface, due to the presence of the cavities, make up about half of the surface area of the skeleton and necessitate modifications to the layered structure.
Most of the movement of the face results from the muscular activity in the soft tissues overlying the spaces, and the surrounding periorbital tissues for the orbits. The movement occurring on the lateral face is essentially passive, secondary to active movement of the muscles on the anterior aspect of the face around the eye and the mouth, and to jaw movement.
Around the bony rims there are anatomical and functional transitions between the relative stability over the fixed area of skeletal attachment and the high mobility of the soft tissue shutters over the bony cavities. This is mainly in layer 4, where there is a concentration of ligaments around the bony rims, at the last available place for soft tissue ligament fixation before the void of the bony cavity (Fig. 6.14).
The generic 5 layer concept also explains the soft tissue anatomy where it overlies the bony cavities. The submuscular space of the lower lids, between the septum orbitale and the overlying preseptal orbicularis, allows mobility of the lids. This space contributes to the pattern of aging changes, particularly the development of lower lid bags. The oral cavity is the largest of the facial spaces and allows movement of most of the midcheek as well as of the lips.
The layers undergo significant adaptations as they leave the bone surface and continue over the orifices. Only the outer three-layer composite superficial fascia forms these soft tissue extensions that are in the form of a composite flap. The SMAS layer within the flap extension has the sphincteric orbicularis muscle around the free edge of the soft tissue aperture of the lids and lips. The facial ligaments in (layer 4) that normally support the composite soft tissue shutters do not exist over the cavities. They are remote where they are condensed along the rim of the bone. This is the basis for the periorbital ligament around the orbital rim, of which the lower lid part is the orbicularis retaining ligament, which stabilizes the overlying orbicularis to the orbital rim periosteum (Fig. 6.11). The orbicularis does not have any attachment to the septum orbitale, (deep fascia) directly beneath, other than the attachments of the orbicularis to the medial and lateral canthal tendons and the nearby orbital rim periosteum.
The extent of the oral cavity has a major impact on the facial structure and on aging of the face. The vestibule of the oral cavity covers a large area of the surface of the maxilla and of the mandible (Fig. 6.14). The part of the skeleton underlying a space is unavailable for ligamentous attachment for support of the soft tissue cover over this large area. Accordingly, the non-attached cheek overlying the oral cavity is the least supported and most mobile part of the face. The indication for a facelift is largely to correct the changes that occur in this poorly supported part of the cheek around the lips.
Anatomy and aging of the face
The youthful face has the appearance of rounded fullness. Laxity gradually develops in the boundaries of the spaces consequent on the repetitive movement that occurs with expression and jaw function. The laxity develops most in the roof of the spaces (level 3). The membranous lining of the spaces undergoes distension in proportion to the degree of laxity developing in the adjacent retaining ligaments, although these are not uniformly affected by laxity. For example, in the lower face the lower masseter ligaments at the anterior boundary of the premasseter space undergo attrition, yet the nearby mandibular ligament remain strong and resist laxity (Fig. 6.15).
As aging changes progress, the bulging over the spaces contrasts with the restriction imposed by the ligaments at the boundaries. These do not bulge as much and form the cutaneous grooves (Fig. 6.3).
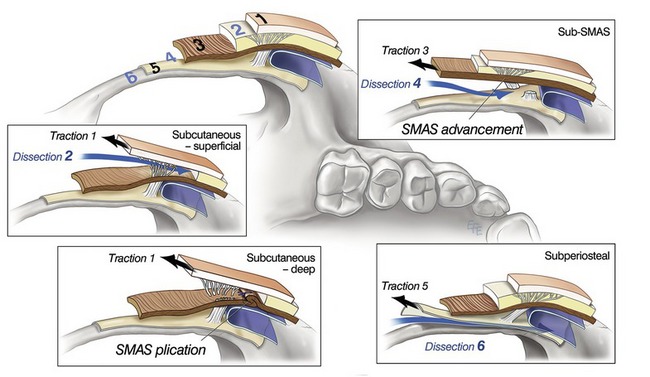
Application of anatomy to surgical technique
Many facelift techniques deliver comparable results. However, the difference on closer analysis is in the extent of harmonious facial shape achieved and the balance between skin tension and shape. Excessive tension flattens natural shape. This is anatomical, and specifically determined by the level in which the dissection has been performed and the layer used for redraping (Fig. 6.16).16
Application to facelift, levels of dissection
Level 4: sub-SMAS
Understanding the anatomy of layer 4 allows sub-SMAS dissection to be utilized in a proactive manner. This provides many advantages based on the fact that the spaces are naturally predissected areas, so the surgical dissection is quick, easy and atraumatic. The surgical approach is commenced with a subcutaneous dissection, which is extended forward until over the posterior part of the roof of the appropriate space. The space is then entered, using traction on the layer 3 roof. Once inside the space, blunt dissection only is used to define the boundaries.
• The transconjunctival (space) approach to access the preseptal space of the lower lid.
• The deep temporal lift dissection from the upper temporal space, around the lateral orbital rim, into the prezygomatic space.
• The premasseter approach to the masticator space, used to reduce displaced buccal fat and to tighten laxity of the overlying superficial fascia lateral to the oral commissure.
When the ‘deep plane facelift’ was introduced, the term ‘deep’ referred to dissection in level 4, deep to the SMAS.17 Although not clear at that time, the deep dissection was only over the lateral face18 as the level of dissection changed to more superficial (deep subcutaneous level 2) at the transition to the anterior face and over the level 3 muscles, orbicularis and zygomaticus major.3,4 The deep plane procedure evolved into the ‘composite facelift’,18 the difference being that the sub-SMAS plane of dissection was also used in the anterior face. Sub-SMAS dissection over the midcheek can be approached either through the lateral approach (extended SMAS)19 or directly the through anterior face via the lower lid (zygorbicular dissection).18,20
Level 2: subcutaneous
The intended role for the fibrous retinacular cutis in the rejuvenation determines which level within the subcutaneous layer to perform the dissection. If the skin flap is to be used for the redraping, the fibrous retinacular component should be left on the flap by performing a ‘deep’ level of subcutaneous dissection. If external plication of the anterior SMAS is the objective, a deep subcutaneous level of dissection is required to visualize the outer surface of the SMAS.21,22 This level of deep subcutaneous dissection at the interface with level 3 has been given several names: the superficial musculoaponeurotic plane (SMAP)11 and the extended supraplatysma plane (ESP).23
Alternatively, when a ‘separate’ SMAS flap is to be used, it is advantageous to keep most of the retinacular cutis mass attached to the SMAS, as this optimizes the strength of the thin SMAS flap. This is achieved with a superficial level of subcutaneous undermining, the so-called, ‘thin skin flap’.24,25
1. Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek; facial layers, spaces, and the midcheek segments. Clin Plast Surg. 2008;35:395–404.
2. Mendelson BC. Chapter: Extended sub-SMAS dissection and cheek elevation. Clin Plast Surg. 1995;22:325–339.
3. Owsley JQ. Lifting the malar pad for correction of prominent nasolabial folds. Plast Reconstr Surg. 1993;91:463.
4. Owsley JQ, Fiala TG. Update lifting the malar fat pad for correction of prominent nasolabial folds. Plast Reconstr Surg. 1997;100:715.
5. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–2227.
6. Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58:80.
7. Mendelson BC, Advances in understanding the surgical anatomy of the face. Eisenmann-Klein M, Neuhann-Lorenz C. Innovations in plastic and aesthetic surgery, Springer Verlag, New York, 2007;141–145.
8. Furnas DW. The retaining ligaments of the cheek. Plast Reconstr Surg. 1989;83:11.
9. Stuzin JM, Baker TJ, Gordon HL. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89:441.
10. Mendelson BC, Freeman ME, Woffles W, Huggins RJ. Surgical anatomy of the lower face; the premasseter space, the jowl and the labiomandibular fold. Aesth Plast Surg. 2008;32:185.
11. Furnas D. The superficial musculoaponeurotic plane and the retaining ligaments of the face. In: Psillakis JM, ed. Deep face – lifting techniques. New York, NY: Thieme Medical Publishers, 1994.
12. Knize DM, ed. The forehead and temporal fossa. Philadelphia: Lippincott Williams and Wilkins, 2001.
13. Moss CJ, Mendelson BC, Taylor GI. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 2000;105:1475.
14. Mendelson BC, Muzaffar AR, Adams WP, Jr. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002;110:885.
15. Aston SJ. The FAME Procedure. Presented at the Annual Meeting of the American Society of Plastic and Reconstructive Surgeons, Dallas, Texas, November 9–13, 1996.
16. Mendelson BC. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2002;109:824–825.
17. Hamra ST. Deep-plane rhytidectomy. Plast Reconstr Surg. 1990;86:53.
18. Hamra ST. Composite Rhytidectomy. Plast Reconstr Surg. 1992;90:1.
19. Stuzin JM, Baker TJ, Gordan HL, Baker TM. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995;22(2):295–311.
20. Hamra ST. The zygorbicular dissection in composite rhytidectomy: An ideal midface plane. Plast Reconstr Surg. 1998;102:1646.
21. Robbins LB, Brothers DB, Marshall DM. Anterior SMAS plication for the treatment of prominent nasolabial folds and restoration of normal cheek contour. Plast Reconstr Surg. 1995;96:1279.
22. Trepsat F. Cornette de Saint-Cyr B, Delmar H, Goin J.-L, Thion A. Les nouveaux liftings. Ann Chir Plast Esthet. 1994;39:597.
23. Hoefflin S. The extended supraplatysmal plane (ESP) facelift. Plast Reconstr Surg. 1998;101:494.
24. Connell BF, Gaon A. Surgical correction of aesthetic contour problems of the neck. Clin Plast Surg. 1983;10:491.
25. Connell BF. Neck contour deformities. The art, engineering, anatomic diagnosis, architectural planning, and aesthetics of surgical correction. Clin Plast Surg. 1987;14:683.