CHAPTER 46 Eyelid malpositions
Entropion and ectropion
Introduction
Intact eyelids cover the eye completely while closed and the lid margins stay in direct contact with the globe while opened1. The lid margin’s contact line to the ocular surface is of vital importance to the integrity of the ocular surface. Dysfunction of lid motility and position can lead to symptoms varying from mild discomfort and dry eye to severe corneal ulceration and sight-threatening ocular surface disease. It is therefore most important to address lid malposition with the appropriate surgical therapy2–4. (Further suggested reading).
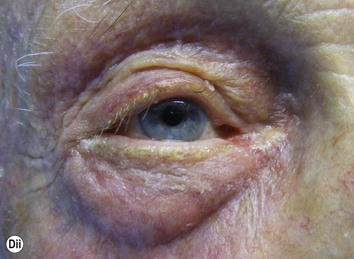
Entropion is a condition in which the lid margin is turned inward onto the ocular surface, while ectropion by definition is the contrary, describing a lid margin that turns outward, leading to exposure of tarsal conjunctiva (Figs 46.1 and 46.2).
Preoperative assessment
Operation techniques
Lower lid ectropion
Tarsoconjunctival excision
If the canthal tendon is tight and ectropion of the medial third of the lid has led to eversion of the lower punctum, an excision of the posterior lamella with or without plication of the lower lid retractors is sufficient to correct the problem5.
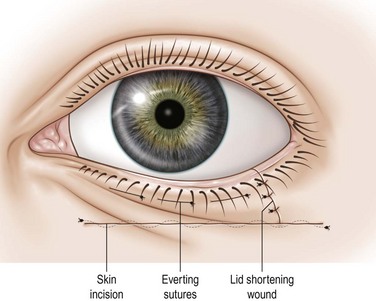
(Tarso)conjunctival excision, inverting sutures, and horizontal lid shortening (lazy T procedure)
If the canthal tendons are tight and the eversion is mainly in the medial third of the lid, inverting the lid margin by excising a part of the conjunctiva and shortening the lid horizontally will correct the malposition. The resulting incision lines after closure forms a T that lies lazily on its side, hence the name6.
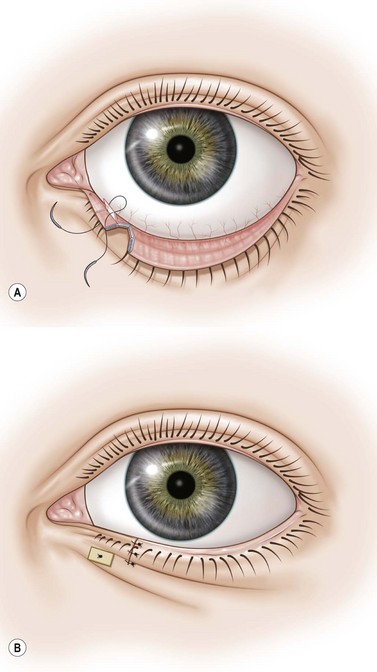
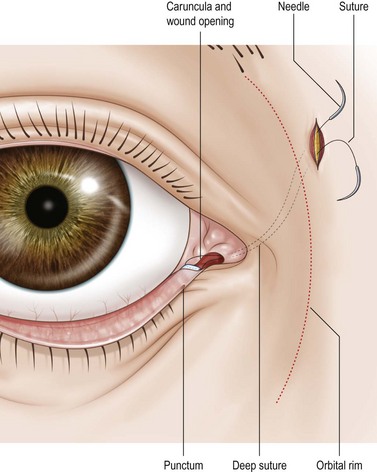
Lateral canthal plication through upper lid crease incision
A lateral canthal tendon laxity can be repaired without shortening the lateral canthal tendon by plicating it with a suture7.
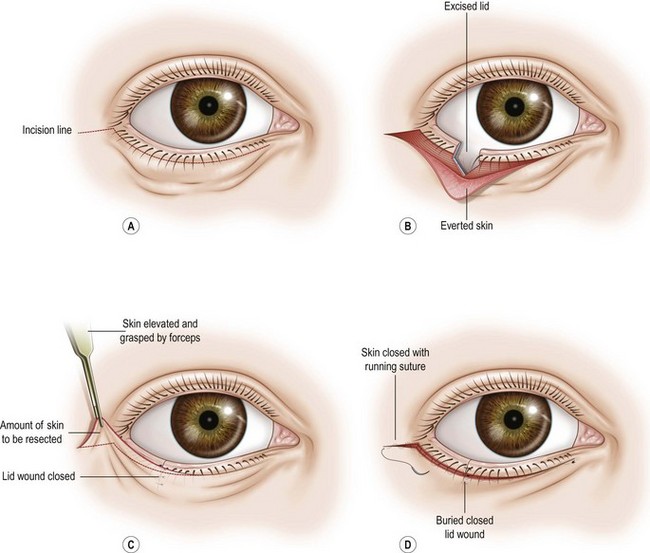
Lateral canthal sling
Laxity of the lateral canthal tendon leads to lower lid ectropion as the orbicularis muscle fibers weaken and become unable to overcome the horizontal tendinous laxity. The ‘snap test’ shows that the lid doesn’t move back to the globe adequately when pulled away. Tightening the inferior limb of the canthal tendon will correct this laxity8.
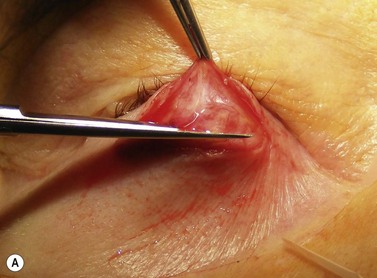
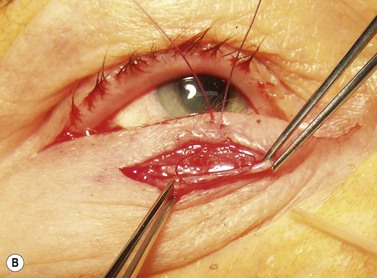
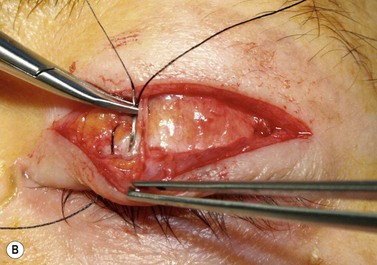
Technique (Fig. 46.5 A–D)
A horizontal subciliary skin incision is made in the lateral third of the lower lid and extended over the lateral canthus. With careful cautery, the incision is deepened to the lateral orbital rim. The lower limb of the lateral canthal tendon is cut and a tarsal strip created9: the lid margin is freed from lash roots, conjunctiva and skin. A double armed 5-0 long-acting absorbable suture is passed through the strip. A slit incision is made through the upper arm of the lateral canthal tendon and each arm of the suture is then passed through the slit, behind the lateral orbital rim, through the periosteum, pulled through anteriorly, tied, and buried under the musculature.
Lower lid entropion
In principle, the decision to correct a lower lid entropion with a certain procedure depends on several key questions10:
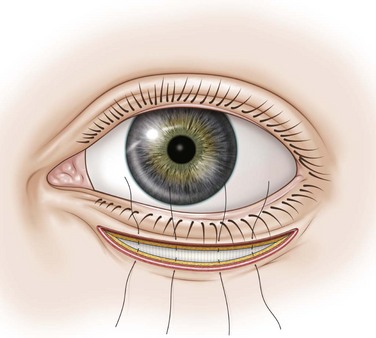
Horizontal (transverse) lid split and everting sutures
This is probably the most commonly used and versatile procedure to correct an involutional entropion with a ‘spastic’ component, where long-term cure is required and no horizontal laxity is present. It can also work satisfactorily, when only mild laxity is present. The technique was first described by Wies11 and produces a transverse fibrous scar to prevent the preseptal orbicularis muscle from moving upward towards the lid margin and pushing it inward. The everting sutures additionally pull the margin outward through the force of the lid retractors.
DIrect lower lid retractor plication (Jones)
The procedure must be combined with a tightening procedure if horizontal laxity is present.
Horizontal lid shortening
If horizontal lid laxity is present, the lid or the canthal tendons have to be shortened. This has to be decided by pulling the lid away from the globe and assessing its spontaneous repositioning (’snap’ test), as well as pulling sideways to assess the position to which either the lacrimal punctum or the lateral canthus can be displaced, respectively. Pulling the lid sideways over the temporal orbital rim will give an estimate of lid laxity and the possible effect of shortening (lateral ‘thumb’ test)12.
Transverse lid split with everting sutures and horizontal lid shortening (Quickert)
Transverse lid split with everting sutures and horizontal lid shortening by lateral tarsal sling
Upper lid ectropion
Inverting suture
Full-thickness skin replacement and horizontal lid shortening
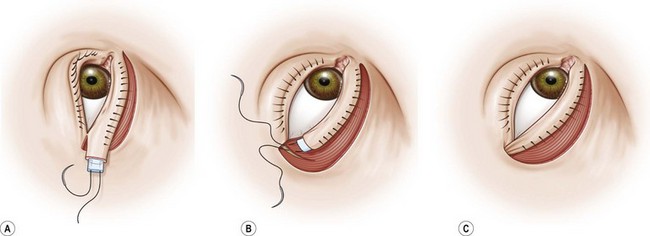
Floppy eyelid repair
The tarsal tissue is soft and the lid foldable and lax. Surgery must aim to correct the horizontal laxity and surplus of tissue and prevent the lid from spontaneous eversion. Shortening the lid can be done by just resecting a full-thickness lateral pentagon, but since this might lead to loss of a large portion of the tarsus it is better to reduce the lid medially, as described below13.
Upper lid entropion
Shortening of the anterior lamella with or without vertical marginal split
Lid split and mucous membrane graft
Summary, suture material, key points, and complications
1 Knop E, Korb DR, Blackie CA, et al. The lid margin is an underestimated structure for preservation of ocular surface health and development of dry eye disease. Dev Ophthalmol. 2010;45:108-122.
2 Collin JRO. A Manual of Systemic Eyelid Surgery, 3rd edn. Oxford: Butterworth Heinemann Elsevier; 2007.
3 McCord CDJr, Codner MA. Eyelid and Periorbital Surgery. St Louis, MS: Quality Medical Publishing; 2008.
4 Tyers AG, Collin JRO. A Colour Atlas of Ophthalmic Plastic Surgery, 3rd edn. Oxford: Butterworth Heinemann Elsevier; 2008.
5 Lee OS. Operation for correction of everted lacrimal puncta. Am J Ophthalmol. 1951;34:575-578.
6 Smith B. The ‘lazy-T’ correction of ectropion of the lower punctum. Arch Ophthalmol. 1976;94:1149-1152.
7 Georgescu D, Anderson RL, McCann JD. Lateral canthal resuspension sine canthotomy. Thesis of the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS). Ophth Plast Rec Surg (in press).
8 Tenzel RR, Buffam FV, Miller GR, et al. The use of the lateral canthal sling in ectropion repair. Can J Ophthalmol. 1977;12:199-202.
9 Anderson RL, Gordy D. The tarsal strip procedure. Arch Ophthalmol. 1979;97:2192-2196.
10 Boboridis L, Bunce C, Rose GE. A comparative study of two procedures for repair of involutional lower lid entropion. Ophthalmology. 2000;107:959-961.
11 Wies FA. Spastic entropion. Trans Am Acad Ophthalmol Otolaryngol. 1955;59:503-506.
12 Danks JJ, Rose GE. Involutional lower lid entropion: to shorten or not to shorten? Ophthalmology. 1998;105:2057-2065.
13 Valenzuela AA, Sullivan TJ. Medial upper eyelid shortening to correct medial eyelid laxity in floppy eyelid syndrome: a new surgical approach. Ophthal Plast Reconstr Surg. 2005;21:259-263.