CHAPTER 73 EXTREMITY REPLANTATION: INDICATIONS AND TIMING
The years since the first successful replantation of an arm in a 12-year-old boy by Malt and McKhann1 in 1964 were marked by evident progress in the reconstructive surgery of limbs. That first revolutionary report was followed by the reports of revascularization of incompletely amputated fingers by Kleinert and colleagues in 19652 and the first successful thumb replantation by Komatsu and Tamai in 1968.3,4 The evolution of microsurgical techniques and an accumulation of experience worldwide, along with the organization of specialized centers, has made replantation of completely or partially amputated extremities a generally accepted treatment of choice.
CLASSIFICATION
All traumatic amputations of extremities are classified based on:
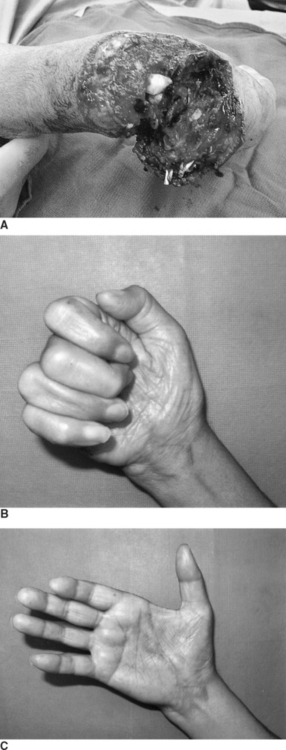
Types of amputations are classified by anatomic criteria. The complete type is clearly defined by its term, that is, an amputation without any tissue connection between amputated and proximal parts of the extremity. An incomplete, or partial amputation is where most of vital anatomic structures are disrupted, and blood circulation in the amputated part of the extremity is absent; without replantation the amputated segment will neither survive nor be functional (Figure 1).
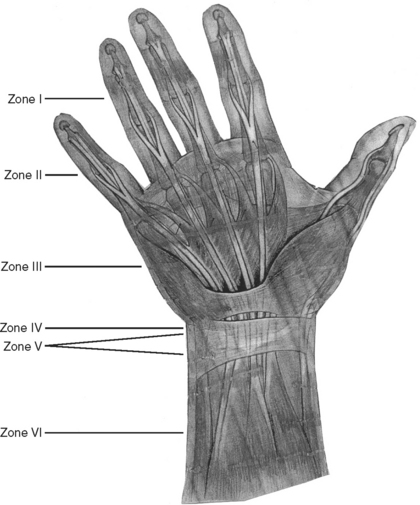
More precise classification of upper extremity amputations and replantations is based on the “zonal” principle, where the upper extremity is divided into six anatomic zones (Figure 2):
INDICATIONS
It appears from the review of the literature and our own experience that the indications for replantation have changed over the years.5 Increasing experience has brought a clear understanding that, in evaluating the results of replantation, the only common denominator is functional outcome. We agree with Pederson that the indications for replantation should not be “based solely on potential viability but are predicated on the potential for long-term function.”6
When considering replantation, one should take into account the status of the amputated part and the patient’s general condition. In general, while any patient with complete or partial amputation can be considered as a candidate for replantation, an ideal candidate should have had not only a relatively benign local status, e.g., an amputation with minimal contamination and/or contusion but also, and maybe more importantly, a real determination for the continuous hard work later to attain and maintain the function of the replanted extremity or its part.
Assuming technical feasibility, the indications for replantation in traumatic amputations follow:
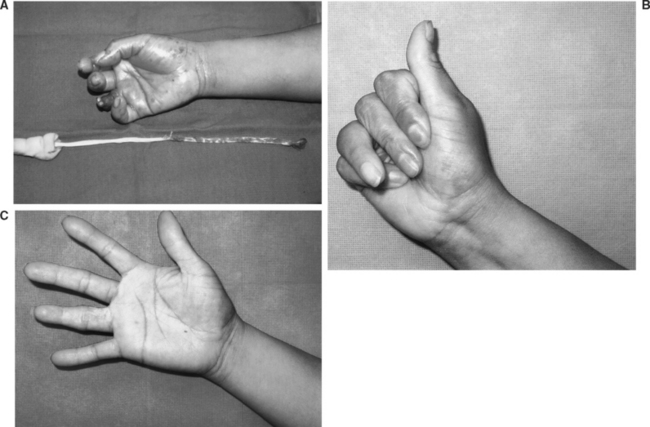
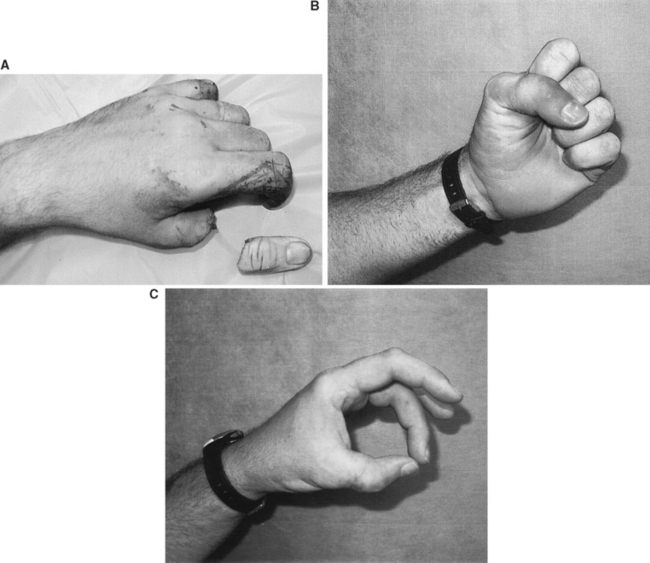
 The thumb provides 40%–50% of the hand’s function. Usually replantation offers the best functional result as compared with other reconstructive options, including toe-to-hand transfer (Figure 4). Even with decreased motion and sensation, the replanted thumb provides such critical tasks of the hand as pinching and grasping. Therefore, all efforts should be made to replant the amputated thumb, unless the functional outcome is dismal.
The thumb provides 40%–50% of the hand’s function. Usually replantation offers the best functional result as compared with other reconstructive options, including toe-to-hand transfer (Figure 4). Even with decreased motion and sensation, the replanted thumb provides such critical tasks of the hand as pinching and grasping. Therefore, all efforts should be made to replant the amputated thumb, unless the functional outcome is dismal. Multiple digital amputations always present a reconstructive puzzle. In general, all feasible replantations should be performed, aiming at the best possible functional result. If not all digits are replantable, the least damaged finger is usually replanted to the most functionally favorable position (heterotopic or transpositional).
Multiple digital amputations always present a reconstructive puzzle. In general, all feasible replantations should be performed, aiming at the best possible functional result. If not all digits are replantable, the least damaged finger is usually replanted to the most functionally favorable position (heterotopic or transpositional). Amputations of a single digit in zone I—despite the recent conservative trend in replantations at the level distal to the flexor superficialis tendon insertion (e.g., Zone I), these usually have favorable functional outcome.
Amputations of a single digit in zone I—despite the recent conservative trend in replantations at the level distal to the flexor superficialis tendon insertion (e.g., Zone I), these usually have favorable functional outcome. All transmetacarpal amputations, or zone III, regardless of the thumb involvement—an absolute indication for replantation.
All transmetacarpal amputations, or zone III, regardless of the thumb involvement—an absolute indication for replantation. Hand amputations at the level of the wrist and above, up to mid-humerus level—the risk of general complications increases with increasing anoxia time and muscle mass.
Hand amputations at the level of the wrist and above, up to mid-humerus level—the risk of general complications increases with increasing anoxia time and muscle mass.1 Malt RA, McKhann CF. Replantation of severed arms. JAMA. 1964;189:716.
2 Kleinert HE, Jablon M, Tsai T. An overview of replantation and results of 348 replants in 245 patients. J Trauma. 1980;20:390.
3 Komatsu S, Tamai S. Successful replantation of completely cut-off thumb. Plast Reconstr Surg. 1968;42:374.
4 Tamai S. Twenty years’ experience of limb replantation: review of 293 upper extremity replants. J Hand Surg. 1982;7:549.
5 Datiashvili RO: Limb Replantation. Moscow, 1991.
6 Pederson WC. Replantation. Plast Reconstr Surg. 2001;107:3.