Chapter 413 Extrapulmonary Diseases with Pulmonary Manifestations
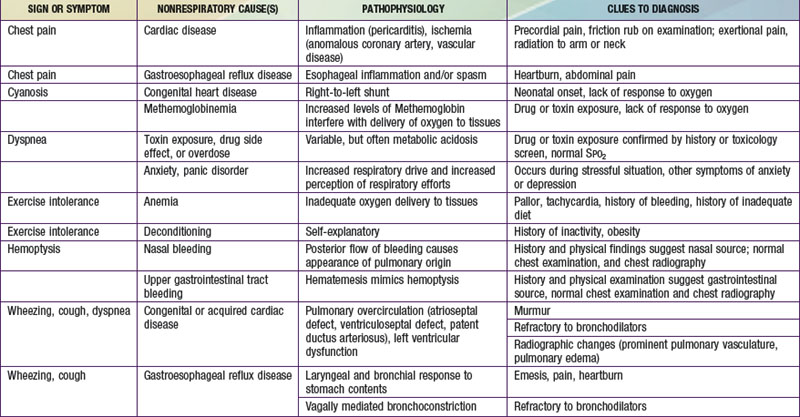
Respiratory symptoms commonly originate from extrapulmonary processes. The respiratory system adapts to metabolic demands and is exquisitely responsive to cortical input; therefore, tachypnea is common in the presence of metabolic stress such as fever, whereas dyspnea may be related to anxiety. Cough most commonly arises from upper or lower respiratory tract disorders, but it can originate from the central nervous system, as with cough tic or psychogenic cough, and it can be a prominent symptom in children with gastroesophageal reflux disease. Chest pain does not commonly arise from pulmonary processes in otherwise healthy children but more often has a neuromuscular or inflammatory etiology. Cyanosis can be caused by cardiac or hematologic disorders, and dyspnea and exercise intolerance can have a number of extrapulmonary causes. These disorders may be suspected on the basis of the history and physical examination, or they may be considered in children in whom diagnostic studies have atypical findings or who show poor response to usual therapy. More common causes of such symptoms are listed in Table 413-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com.
Evaluation
Disorders of other organ systems, and many systemic diseases, can have significant respiratory system involvement. Although it is most common to encounter these complications in patients with known diagnoses, respiratory system disease is sometimes the sole or most prominent symptom at the time of presentation. Acute aspiration during feeding can be the presentation of neuromuscular disease in an infant who initially appears to have normal muscle tone and development. Complications can be life-threatening, particularly in immunocompromised patients. The onset of respiratory findings may be insidious; for example, pulmonary vascular involvement in patients with systemic vasculitis may appear as an abnormality in diffusing capacity of the lung for carbon monoxide (DLCO) before the onset of symptoms. Disorders that commonly have respiratory complications are listed in Table 413-2.
Table 413-2 DISORDERS WITH FREQUENT RESPIRATORY TRACT COMPLICATIONS
| UNDERLYING DISORDER(S) | RESPIRATORY COMPLICATIONS | DIAGNOSTIC TESTS |
|---|---|---|
| Autoimmune disorders | Pulmonary vascular disease, restrictive lung disease, pleural effusion (especially systemic lupus erythematosus), upper airway disease (Wegener granulomatosis) | Spirometry, lung volume determination, oximetry, diffusing capacity of the lung for carbon monoxide (DLCO), chest radiography, upper airway endoscopy, and/or CT |
| Central nervous system disease (static or progressive) | Aspiration of oral or gastric contents | Chest radiography, videofluoroscopic swallowing study, esophageal pH probe, fiberoptic bronchoscopy |
| Immunodeficiency | Infection, bronchiectasis | Chest radiography, fiberoptic bronchoscopy, chest CT |
| Liver disease | Pleural effusion, hepatopulmonary syndrome | Chest radiography, assessment of orthodeoxia |
| Malignancy and its therapies | Infiltration, metastasis, malignant or infectious effusion, parenchymal infection, graft versus host disease (bone marrow transplant) | Chest radiography, chest CT, fiberoptic bronchoscopy, lung biopsy |
| Neuromuscular disease | Hypoventilation, atelectasis, pneumonia | Spirometry, lung volume determination, respiratory muscle force measurements |
| Obesity | Restrictive lung disease, obstructive sleep apnea syndrome, asthma | Spirometry, lung volume determination, nocturnal polysomnography |
Bowman CM. Hemoptysis. In: Loughlin GM, Eigen H, editors. Respiratory disease in children: diagnosis and management. Baltimore: Williams & Wilkins; 1994:201-205.
Loughlin GM. Chest pain. In: Loughlin GM, Eigen H, editors. Respiratory disease in children: diagnosis and management. Baltimore: Williams & Wilkins; 1994:207-214.
Methemoglobinemia, eMedicine Journal http://emedicine.medscape.com/article/956528-overview, 2002.