CHAPTER 8 External Fixation of Distal Radius Fractures
External fixation has been used for the treatment of distal radius fractures for more than 50 years. Although the fixator configurations have undergone considerable modification over time, the type of fixator itself is not as important as the underlying principles that provide the foundation for external fixation. Although volar plate fixation is currently popular, the indications for external fixation remain largely unchanged. Newer fixator designs also have expanded the traditional usage to include nonbridging applications, which allow early wrist motion. This chapter focuses on the myriad uses for external fixation and the shortcomings and potential pitfalls.
Anatomy
There are some important anatomical points one must bear in mind when considering external fixation of the distal radius. The articular surface of the radius is triangular with the apex of the triangle at the radial styloid. It slopes in a volar and ulnar direction with a radial inclination of 23 degrees (range 13 to 30 degrees), a radial length of 12 mm (range 8 to 18 mm), and an average volar tilt of 12 degrees (range 1 to 21 degrees).1 The dorsal surface of the distal radius is convex and irregular, and it is covered by the six dorsal extensor compartments. The dorsal cortex is thin, which often results in comminution that may lead to an abnormal dorsal tilt. Lister’s tubercle acts as a fulcrum for the extensor pollicis longus (EPL) tendon, which lies in a groove on the ulnar side of the tubercle. The volar side of the distal radius, which is covered by the pronator quadratus, is flat and makes a smooth curve that is concave from proximal to distal. When inserting the dorsal pins, it is important to engage the volar ulnar lip of the distal radius where the bone density is highest, especially in osteopenic bone.2
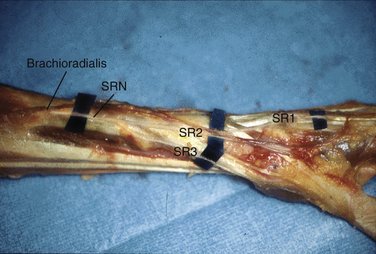
The dorsum of the radius is cloaked by the arborizations of the superficial radial nerve (SRN) and the dorsal cutaneous branch of the ulnar nerve. The SRN exits from under the brachioradialis approximately 5 cm proximal to the radial styloid and bifurcates into a major volar and a major dorsal branch at a mean distance of 4.2 cm proximal to the radial styloid (Fig. 8-1). Either partial or complete overlap of the lateral antebrachial cutaneous nerve with the SRN occurs up to 75% of the time.3 The dorsal cutaneous branch of the ulnar nerve arises from the ulnar nerve 6 cm proximal to the ulnar head and becomes subcutaneous 5 cm proximal to the pisiform. It crosses the ulnar snuffbox and gives off three to nine branches that supply the dorsoulnar aspect of the carpus, small finger, and ulnar ring finger. Open pin insertion allows identification and protection of these branches.
The proximal pins are placed at the junction of the proximal and middle thirds of the radius. At this level, the radius is covered by the tendons of the extensor carpi radialis longus, extensor carpi radialis brevis, and extensor digitorum communis. The proximal pins can be inserted in the standard mid lateral position by retracting the brachioradialis tendon and the SRN, in the dorsoradial position between the extensor carpi radialis longus and extensor carpi radialis brevis, or dorsally between the extensor carpi radialis brevis and extensor digitorum communis, which carries less risk of injury to the SRN.4
Ligamentotaxis
Limitations of Ligamentotaxis
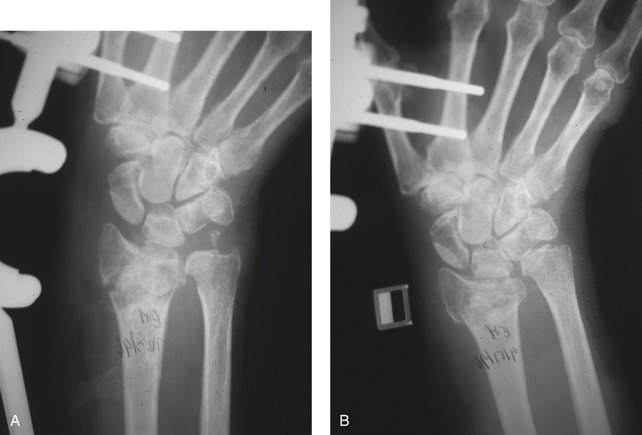
Ligamentotaxis has many shortcomings when applied to the treatment of displaced intra-articular fractures of the distal radius. First, because ligaments exhibit viscoelastic behavior,5 there is a gradual loss of the initial distraction force applied to the fracture site through stress relaxation.6 The immediate improvements in radial height, inclination, and volar tilt are significantly decreased by the time of fixator removal (Fig. 8-2).7
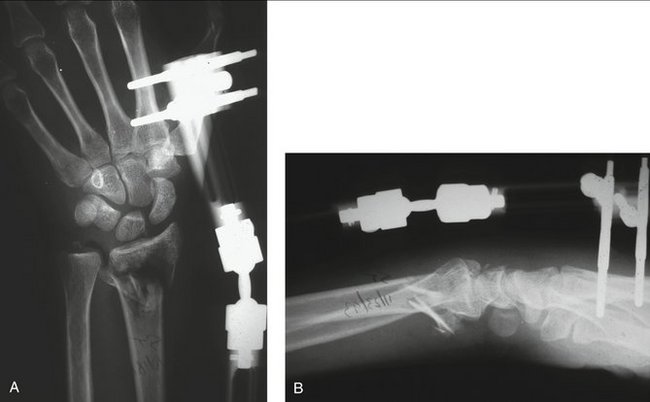
FIGURE 8-2 Limitations of Ligamentotaxis. A, Initial overdistraction restores radial length. B, Note the persistent dorsal tilt of the articular surface even with maximum distraction.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
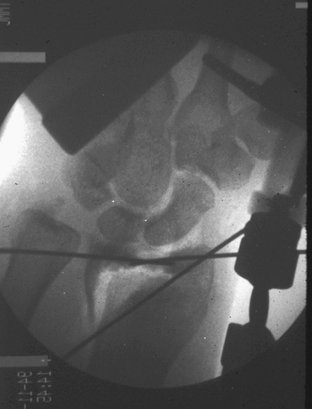
Traction does not correct the dorsal tilt of the distal fracture fragment because the stout volar radiocarpal ligaments are shorter, and they pull out to length before the thinner dorsal radiocarpal ligaments exert any traction.8 Excessive traction may increase the dorsal tilt (Fig. 8-3).9 A dorsally directed vector is still necessary to restore the normal volar angulation. This vector is usually accomplished by applying manual thumb pressure over the dorsum of the distal fragment. With intra-articular fractures, ligamentotaxis reduces the radial styloid fragment, but for the aforementioned reasons, it does not reduce a depressed lunate fragment.10 When there is a sagittal split of the medial fragment, traction causes the volar medial fragment to rotate, which often necessitates an open reduction. External fixation cannot control radial translation and cannot be used with an unstable distal radioulnar joint (Fig. 8-4).
Biomechanical Considerations for External Fixation
Fracture Site Loads
External fixation is considered flexible fixation.11 The biomechanical requirements of external fixation for fractures of the distal radius have not been ascertained because until more recently, the magnitude and direction of the physiological loads on the distal radius were dynamic and unknown. Work by Rikli and colleagues12 has shed new light on this point, however. Using a new capacitive pressure-sensory device, these investigators measured the in vivo dynamic intra-articular pressures under local anesthesia in the radioulnocarpal joint of a healthy volunteer. With the forearm in neutral rotation, the forces ranged from 107N with wrist flexion to 197N with wrist extension. The highest forces of 245N were seen with the wrist in radial deviation and the forearm in supination. Presumably, any implant or external fixator would need to be strong enough to neutralize these loads to permit early active wrist motion. Rikli and colleagues12 also identified two centers of force transmission. The first center was opposite the scaphoid pole, which would represent the radial column. The second center, which would represent the intermediate column of the wrist, took a considerable amount of the load and was opposite the lunate, extending ulnarly over the triangular fibrocartilaginous complex.
Construct Rigidity
Increasing the rigidity of the fixator does not appreciably increase the rigidity of fixation of the individual fracture fragments.13 The stability of the construct can be augmented in many ways, however. After restoration of radial length and alignment by the external fixator, percutaneous pin fixation can lock in the radial styloid buttress and support the lunate fossa fragment.14 A fifth radial styloid pin attached to the frame of a spanning AO external fixator (Synthes, Paoli, PA) prevents a loss of radial length through settling and leads to improved wrist range of motion compared with a four-pin external fixator.15 The addition of a dorsal pin attached to a sidebar easily corrects the dorsal tilt found in many distal radius fractures.16,17
Kirschner wire (K-wire) fixation enhances the stability of external fixation. The combination of an external fixator augmented with 0.62-inch K-wires approaches the strength of a 3.5-mm dorsal AO plate (Synthes, Paoli, PA).18 Supplemental K-wire fixation is more crucial to the fracture fixation than the mechanical rigidity of the external fixator itself.13 Stabilizing a fracture fragment with a nontransfixing K-wire that is attached to an outrigger is just as effective as a K-wire that transfixes the fracture fragments.19
Bridging External Fixation
Temporary External Fixation: Indications
Compared with conventional plate fixation, bridging external fixation may be used in a temporary manner, or it may be used for definitive management of the distal radius fracture. Bindra20 listed the following indications for this technique:

FIGURE 8-5 A, Open distal radius fracture. B, Temporary stabilization with a bridging external fixator.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Rikli and colleagues21 use temporary bridging external fixation for complex fractures to aid in the provisional fracture reduction and to allow a better computed tomography (CT) evaluation of the fracture characteristics before double-plate fixation.
Definitive External Fixation: Indications
Indications for definitive external fixation include the following:
Complications
Fixator loosening with loss of fracture position can be avoided by periodically checking and tightening the fixator connections. Fixator failure by itself is uncommon, but many commercially available fixators are approved for single use only because of the risk of unrecognized material fatigue or failure of any locking ball joints. Pin site complications include infection, loosening, and interference with extensor tendon gliding. The risk of injury to branches of the SRN mandate open pin site insertion. Bad outcomes associated with external fixation are often related to overdistraction. One biomechanical study documented the effect of distraction of the wrist on metacarpophalangeal joint motion. More than 5 mm of wrist distraction increases the load required for the flexor digitorum superficialis to generate metacarpophalangeal joint flexion for the middle, ring, and small fingers. For the index finger, however, 2 mm of wrist distraction significantly increases the load required for flexion at the metacarpophalangeal joint.22 Many cases of intrinsic tightness and finger stiffness that are attributed to reflex sympathetic dystrophy are a consequence of prolonged and excessive traction, which can be prevented by limiting the duration and amount of traction and instituting early dynamic metacarpophalangeal flexion splinting even while in the fixator.
The degree and duration of distraction correlate with the amount of subsequent wrist stiffness.23 Distraction, flexion, and locked ulnar deviation of the external fixator encourage pronation contractures (Fig. 8-6). Distraction also increases the carpal canal pressure,24 which may predispose to acute carpal tunnel syndrome. Metaphyseal defects should be grafted to diminish bending loads and to allow fixator removal after 6 to 7 weeks, which minimizes the fixator-related complications.
Results
Margaliot and associates25 did a meta-analysis of 46 articles with 28 (917 patients) external fixation studies and 18 (603 patients) internal fixation studies. They did not detect a clinically or statistically significant difference in pooled grip strength, wrist range of motion, radiographic alignment, pain, or physician-rated outcomes between the two treatment arms. There were higher rates of infection, hardware failure, and neuritis with external fixation and higher rates of tendon complications and early hardware removal with internal fixation. Considerable heterogeneity was present in all of the studies, which adversely affected the precision of the meta-analysis.
Augmented External Fixation
The use of supplemental K-wire fixation can expand the indications for external fixation. As noted earlier, K-wire fixation not only enhances the reduction of the fracture fragments, but also increases the rigidity of the entire construct. Many authors have stressed the importance of using the external fixator as a neutralization device rather than a traction device. Ligamentotaxis is used to obtain a reduction of the fracture fragments, which is then captured with percutaneous K-wire fixation. The traction on the fixator can be reduced, which allows positioning of the wrist in neutral or slight extension (Fig. 8-7).9 This positioning serves to reduce extensor tendon tightness and facilitates finger motion. In a study of intrafocal pinning, Weil and Trumble26 noted that in patients older than 55 years and younger patients with comminution involving two or more surfaces of the radial metaphysis (or >50% of the metaphyseal diameter), bridging fixation was necessary in addition to percutaneous pin fixation to prevent late fracture collapse. In four-part fractures in which there is a sagittal split of the medial fragment, longitudinal traction accentuates the palmar translation and rotation of the volar medial fragment (Fig. 8-8). Dorsal to volar K-wire placement carries the risk of injury to the volar neurovascular bundles, especially with K-wire migration. For these reasons, any sagittal split of the articular surface typically requires open treatment27 (Fig. 8-9).
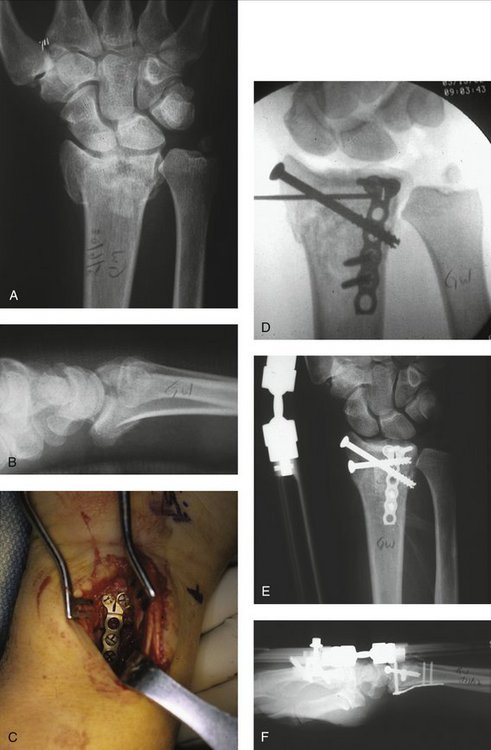
FIGURE 8-9 Limited Internal Fixation. A, Anteroposterior x-ray of a displaced four-part fracture. B, Lateral view shows a sagittal split of the medial fragment. C, Internal fixation of medial fragment through a limited volar ulnar approach. D, Subchondral K-wire inserted to support the joint surface. E, Second K-wire replaced by a percutaneous screw, which stops short of the distal radioulnar joint. F, Lateral view shows restoration of normal tilt and reduction of the sagittal split.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Results
Kreder and associates28 compared the results of open reduction and internal fixation (ORIF) versus external fixation and pinning. The study randomly assigned 179 adult patients with displaced intra-articular fractures of the distal radius to receive indirect percutaneous reduction and external fixation (n = 88) or ORIF (n = 91). There was no statistically significant difference in the radiological restoration of anatomical features or the range of movement between the groups at 2 years. The patients who underwent indirect reduction and percutaneous fixation had a more rapid return of function and a better functional outcome, however, than the patients who underwent ORIF, provided that the intra-articular step and gap deformity were minimized.
Complications
In one study of 70 cases of external fixation and percutaneous pinning, 49% of cases lost more than 5 degrees of volar tilt after reduction at the 6-month follow-up despite the use of pinning. Initial deformity, patient age, use of bone graft, and duration of external fixation were not predictors of loss of reduction. No specific predictor of loss of reduction was noted, although there was a trend toward a loss of reduction in younger patients.29
Nonbridging External Fixation
Extra-articular Fractures
Indications
Nonbridging external fixation is indicated in any extra-articular fracture in which there is a high risk of late collapse, or if there is redisplacement of the fracture after an acceptable closed reduction (Fig. 8-10). When there is significant displacement on the injury films, there is a high likelihood of collapse even if the initial reduction is satisfactory. Trumble and colleagues30 recommend supplemental internal or external fixation in younger patients for fractures with more than 2 mm of radial shortening and more than 15 degrees of dorsal tilt after a closed reduction, especially if there is comminution of two or more cortices.

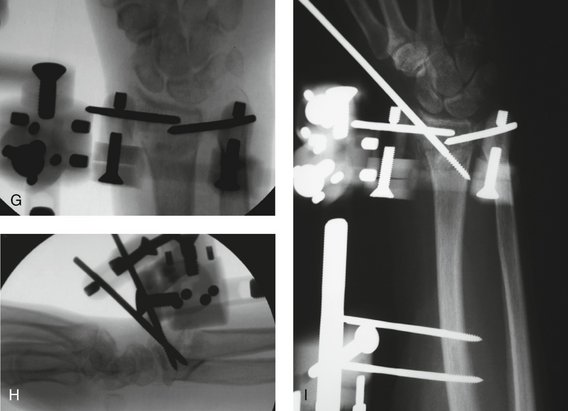
FIGURE 8-10 Nonbridging External Fixation. A, A 55-year-old woman with extra-articular radius fracture. B, Note the marked dorsal comminution. C, Redisplacement at 8 days with loss of radial height. D, Loss of volar tilt. E, Appearance after percutaneous bone grafting. F, Lateral view after bone grafting. G, Insertion of dorsal fixator pins. H, Lateral view with nonbridging external fixator. I, Postoperative x-ray at 1 week with additional radial styloid pin.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Contraindications
Nonbridging external fixation is contraindicated when the distal fragment is too small for pin placement. At least 1 cm of intact volar cortex is required for pin purchase. Dorsal comminution does not preclude a successful result. This technique is not applicable in patients with volar displaced or volar shear fractures or in children with open epiphyses.40
Surgical Technique
The technique is similar to bridging external fixation, with the use of a tourniquet and intraoperative fluoroscopy, but a traction tower is not required. Two dorsal 3-mm pins are inserted in the distal fragment through separate longitudinal incisions. The pins can be placed on either side of Lister’s tubercle or the EPL tendon and between the extensor digitorum communis and the extensor digiti minimi. The starting position of the pin should be approximately halfway between the fracture and the radiocarpal joint. A temporary K-wire can be used to gauge the proper angle. The first pin is inserted through Lister’s tubercle parallel to the joint surface in the lateral plane until it engages the volar cortex. The second dorsal pin is inserted in a similar manner, but on the ulnar side of the EPL or extensor digitorum communis tendons. The dorsal tilt is corrected by levering the pins distally until the normal volar inclination has been restored. The fixator frame is applied and tightened.
Complications
Pin pullout resulting from fracture of the distal fragment can occur if the distal fragment is too small or osteopenic, or if the reduction is too vigorous. If this occurs, the fixator can be converted to a bridging construct. An incomplete reduction also is possible, especially with nascent malunions. Over-reduction of the fracture also can occur, especially when there is volar comminution.31
Results
McQueen31 performed a prospective study of 641 patients with unstable fractures of the distal radius treated with external fixation. Of these cases, 59% were treated with nonbridging external fixation, mostly AO type A3.2 and C2.1 fractures. Patients treated with nonbridging external fixation had statistically significantly better radiological results throughout the period of review. In particular, this technique consistently restored the volar tilt and carpal alignment. Radiological improvement was mirrored by functional improvement. Most functional indices were statistically better at an early stage, whereas wrist flexion and grip strength remained significantly better at the final review. Complication rates were similar between the two groups.
Intra-articular Fractures
Early wrist motion after intra-articular fractures provides many possible benefits, including diminished stiffness, stimulation of cartilage repair,32 and decreased osteopenia of the distal fragments.33 To accomplish this with nonbridging external fixation, the construct must be able to withstand the forces generated during active and passive wrist motion.
Biomechanical Considerations
The author undertook a biomechanical study to examine the feasibility of nonbridging external fixation of simulated three-part and four-part intra-articular fractures.34 All of the fractures were stabilized using a single custom nonbridging external fixator that has an integrated dorsal sidearm (Fragment Specific Fixator; South Bay Hand Surgery LLC, Torrance, CA) (see Fig. 8-10).
The study conclusion was that nonbridging external fixation with new fixator designs could be applied to the treatment of intra-articular fractures. Putnam and coworkers35 have shown that for every 10N of grip force, 26N is transmitted through the distal radius metaphysis. They recommended that the rehabilitation grip forces should be kept at less than 140N with external fixation to prevent or minimize fixation failure. This also seems to be a safe limit because it pertains to nonbridging external fixation as well.
Similar to a fixed-angle plate, the biomechanical rationale for the Fragment Specific Fixator is to transfer load from the fixed support of the articular surface to the intact radial shaft, bypassing any metaphyseal comminution (Fig. 8-11). In contrast to a fixed-angle blade plate, the fixator pin angle is freely adjustable so that it can be adapted to the fracture site plane, which may diminish fracture malalignment.
Surgical Technique Using the Fragment Specific Fixator
Reduction of Dorsal Tilt
The dorsal tilt can be corrected by using a Freer elevator inserted percutaneously in the fracture site after the radial styloid reduction. Alternatively, the tilt can be corrected as described for the extra-articular fractures. In this case, the radial styloid is reduced secondarily. Two dorsal 3-mm pins are inserted in the distal fragment through separate longitudinal incisions as described for the extra-articular fractures. The first 3-mm pin is inserted through Lister’s tubercle parallel to the joint surface in the lateral plane until it engages the volar cortex. The dorsal sidearm is positioned parallel to the joint space. A single-pin clamp attached to the dorsal sidearm is fastened to this pin, then both are locked in place. After the two proximal pins are inserted in the mid radius, the distractor unit is used to lengthen the fixator until the volar tilt of the articular surface has been restored. An additional dorsal pin is inserted on the ulnar side of the EPL or extensor digitorum communis tendons using the second single-pin clamp on the outrigger bar as a drill guide. The radial styloid pins are inserted as described earlier (Fig. 8-12).
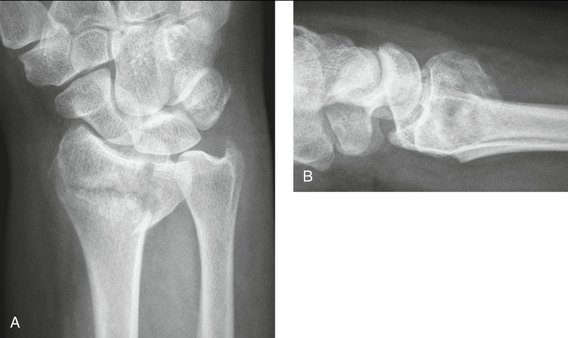
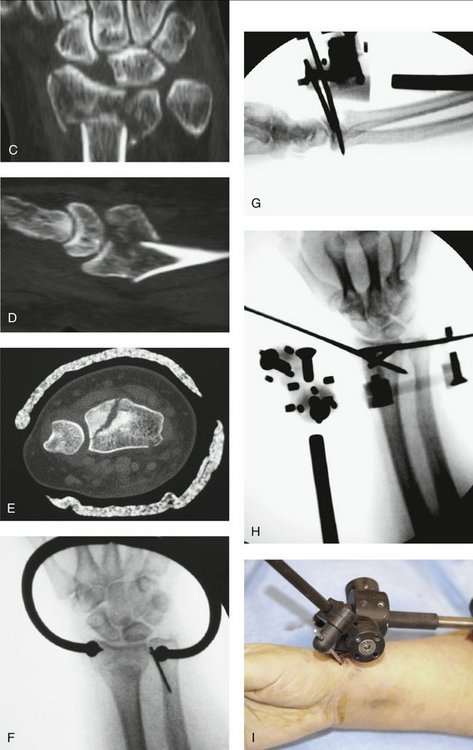
FIGURE 8-12 A, Displaced three-part distal radius fracture. B, Dorsal tilt of the joint surface. C, Anteroposterior CT scan highlights the size of the medial fragment. D, Lateral CT scan shows the sagittal split of the medial fragment. E, Coronal CT scan shows disruption of the sigmoid notch. F, Reduction of coronal split with percutaneous bone forceps. G, Reduction of dorsal tilt and application of nonbridging fixator. H, Insertion of an oblique radial styloid pin. I, Palmar view of the radial styloid pin, which does not interfere with thumb motion.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Caveats
Nonbridging external fixation of intra-articular distal radius fractures should be reserved for manually active patients with good bone quality without evidence of prior wrist arthritis. The lunate fragment must be sufficiently large to support two 3-mm pins. A CT scan with anteroposterior, lateral, and coronal views is helpful to assess the fracture line patterns to aid pin insertion (Fig. 8-13).
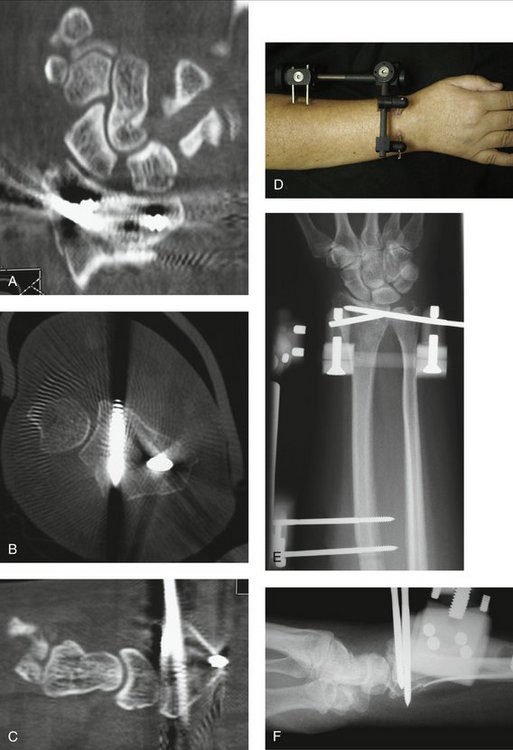

FIGURE 8-13 A, Anteroposterior CT scan shows the anatomical reconstruction of the joint space. B, Coronal CT scan shows fixation of the dorsomedial fragment with the fixator pin. C, Correction of dorsal tilt seen on lateral CT scan. D, Appearance at 4 weeks after removal of radial styloid pin. E, Anteroposterior view. F, Lateral view. G, Wrist flexion in fixator at 4 weeks. H, Anteroposterior view at 4 months. I, Lateral view at 4 months.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Complications
Immediate complications consist of injury to branches of the SRN or dorsal cutaneous branches of the ulnar nerve. Loss of fixation because of poor pin placement or interference with extensor tendon gliding can be minimized by careful technique and open rather than percutaneous pin insertion. The use of many standard external fixator frames applied in a nonbridging manner can result in articular incongruity. Late collapse after fixator removal can occur in osteopenic bone, which often requires subchondral support beyond the 6 weeks of fixator application. Because of the risk of late collapse, adjuvant internal fixation with locking plates is advised in elderly and osteopenic patients, as fracture site settling may occur for up to 6 months.29
Results
Reports of nonbridging external fixation (or radioradial external fixation) for the treatment of intra-articular fractures are sparse and mostly restricted to the European literature. Krishnan and colleagues36 reported a clinical trial of 30 patients with Frykman type 7 and 8 fractures who were treated with the Delta frame nonbridging external fixator (Mathys Medical Ltd., Bettlach, Switzerland). Although favorable wrist motion was reported, the median intra-articular step was 2.8 mm (range 0 to 9.1 mm) with a median intra-articular gap of 1.8 mm (range 0 to 13.4 mm).33
Gradl and coworkers37 examined 25 consecutive patients with fractures of the distal radius who were treated with nonbridging external fixation for 6 weeks. The stepwise surgical technique comprised a preliminary joint-bridging construction for reduction purposes, the subsequent insertion of three to four K-wires in the distal fragment, the assembling of the K-wires to a dorsal outrigger bar that was nearly parallel to the fracture line, and lastly the removal of the joint-bridging part. Clinical and radiological evaluation was performed on the first and seventh days, at 6 weeks, and 2 years after surgery. All fractures united with a palmar tilt (≥0) and articular step-off (<2 mm). A loss of radial length occurred in four patients in whom only three K-wires were inserted in the distal fragment. No radial shortening was seen in fractures with four K-wires inserted in the distal fragment. The functional results at 2 years after surgery showed an average extension of 55 degrees and flexion of 64 degrees without significant differences between extra-articular and intra-articular fractures. There were no instances of extensor tendinitis or pin loosening in the distal fragment; however, there were three cases of proximal pin tract infections.37
Arthroscopic-Assisted Reduction and Nonbridging External Fixation
Surgical Technique
Intraoperative fluoroscopy is used frequently throughout the case, with the C-arm positioned horizontal to the floor. It is preferable to wait 3 to 10 days to allow the initial intra-articular bleeding to stop. I have found it useful to perform much of the procedure without fluid irrigation using the dry technique of del Pinal and colleagues,38 which eliminates the worry of fluid extravasation. If fluid irrigation is used, inflow is through a large-bore cannula in the 4U, 5U, or 6U portal with the outflow through the arthroscope cannula. The working portals include the volar radial (VR) and 6R portal for fracture visualization and the 3/4 portal for instrumentation, but all of the portals are used interchangeably. Lactated Ringer’s solution is preferred over saline solution, and the forearm is wrapped with Coban to limit extravasation.
The fracture hematoma and debris are lavaged, and any early granulation tissue is débrided with a resector. Mehta and colleagues39 described a five-level algorithm for reducing the fracture fragments. This algorithm included the “London technique” for comminuted intra-articular fractures in which the K-wires were advanced through the distal ulna into the subchondral distal radius and withdrawn from the radial aspect so that they did not encroach on the distal radioulnar joint (Fig. 8-14).
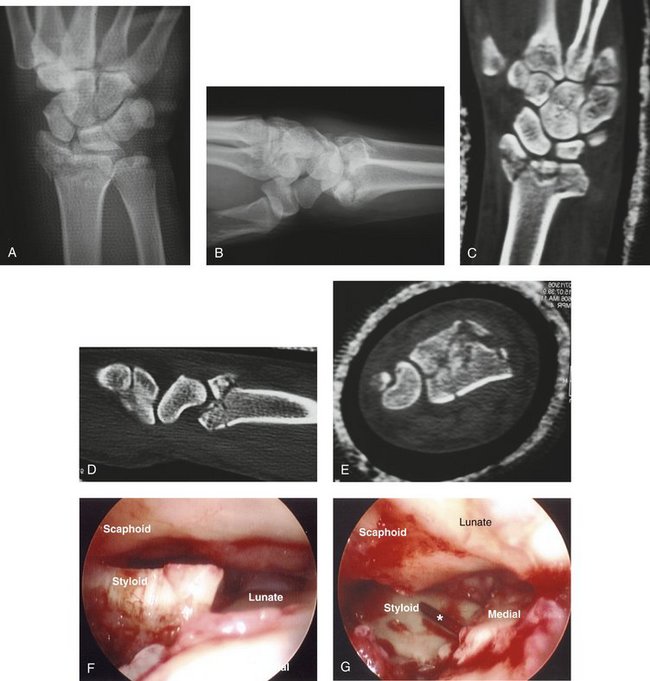

FIGURE 8-14 Arthroscopic-Guided Pinning and Nonbridging External Fixation. A, Comminuted intra-articular distal radius fracture. B, Lateral view. C, Anteroposterior CT scan reveals the extent of the intra-articular fragmentation. D, Lateral CT scan highlights the small dorsal rim fragments. E, Coronal CT scan shows the sigmoid notch disruption. F, Arthroscopic view of joint surface shows the degree of comminution. G, A percutaneous styloid is inserted through the ulna to capture and control the medial fragment. H, Percutaneous reduction of dorsal tilt. I, Fluoroscopic appearance. J, Arthroscopic view after reduction and pinning. K, Fluoroscopic view after arthroscopic reduction. L, Application of nonbridging external fixator. M, Result at 6 months with restored radial height and tilt. N, Congruent joint space with neutral lateral tilt.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
The radial styloid is reduced through ligamentotaxis while the arm is suspended in the traction tower. A Freer elevator also may be placed in the fracture site under fluoroscopic control to facilitate this step. A 1-cm incision is made over the styloid to prevent injury to the SRN, and two 0.62-inch K-wires are inserted for manipulation of the styloid fragment. The fracture site is best assessed by viewing across the wrist with the scope in the 6R portal, to gauge the rotation of the styloid. The K-wires are used as joysticks to manipulate the fragment, then one K-wire is driven forward to capture the reduction. The radial styloid fragment is used as a landmark to which the depressed lunate fragment is reduced. An elevator or large pin is inserted percutaneously to elevate the lunate fragment, which is held reduced with large tenaculum forceps. Forceps with large curved jaws are preferred to prevent crushing the SRN. The tips of the forceps may be placed directly against the ulna to facilitate this step.
Ulnar Styloid Fractures and Distal Radioulnar Joint Instability
Ulnar styloid fractures may or may not be associated with disruption of the deep foveal insertion of the triangular fibrocartilaginous complex and secondary distal radioulnar joint instability. The deep fibers of the distal radioulnar joint can be directly assessed through a volar distal radioulnar joint portal.40 If there is a disruption of the deep fibers of the triangular fibrocartilaginous complex, an open foveal repair can be done.41 If the triangular fibrocartilaginous complex remains well attached to the ulnar styloid fragment, ORIF of the styloid using K-wires and tension band fixation and cannulated screws as bone anchors is performed.
Combined Fixation
Combined fixation can be performed with the fixator applied in either a bridging or a nonbridging mode. In many instances, the Fragment Specific Fixator is applied in a radial uniplanar configuration in conjunction with a combination of a volar or a dorsal plate or both (Fig. 8-15). In these instances, the fixator acts as a “third plate,” which replaces the radial styloid plate. Alternatively, the fixator can be combined with two volar plates when there is marked periarticular dorsal comminution (Fig. 8-16). The fixator can be applied in a bridging fashion with dorsal outrigger support (Fig. 8-17). It also can be applied in a nonbridging fashion after plate fixation (Fig. 8-18).
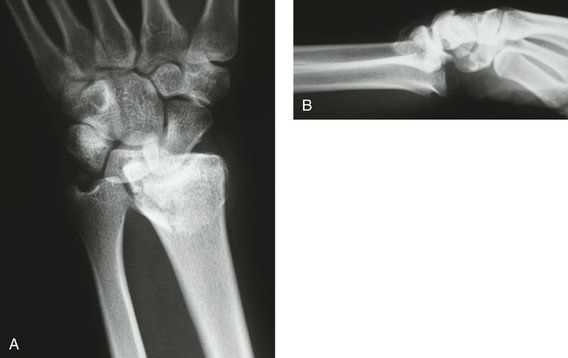
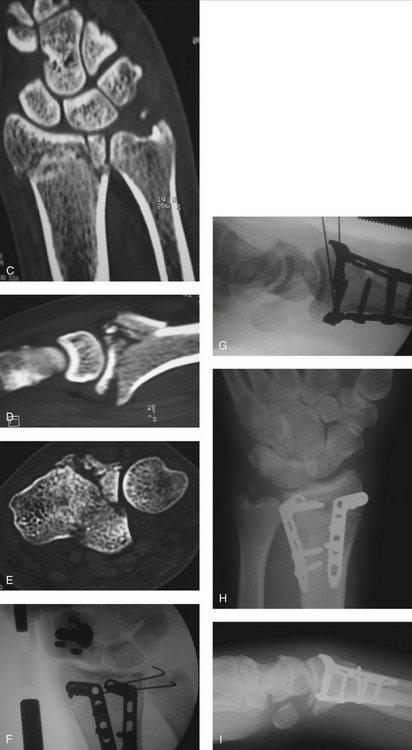
FIGURE 8-15 A 3-Year-Old Boy with Displaced Intra-articular Fracture. A, Anteroposterior view shows marked radial shortening. B, Lateral view shows a small distal fragment and marked dorsal tilt. C, Anteroposterior CT scan reveals the small medial fragment. D, Lateral CT scan highlights the thin volar medial articular fragment. E, Coronal CT scan reveals a small, comminuted dorsomedial wall fragment with sigmoid notch disruption. F, Intraoperative x-ray shows anatomical restoration of the joint surface, but nonrigid pin fixation of the dorsal wall fragments, which necessitates temporary bridging external fixation to unload the joint space. G, Lateral view shows sandwiching of the fracture fragments with volar and dorsal plates with restored volar tilt. H, Posteroanterior view at 4 weeks after fixator removal. I, Lateral view at 4 weeks after fixator removal.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)

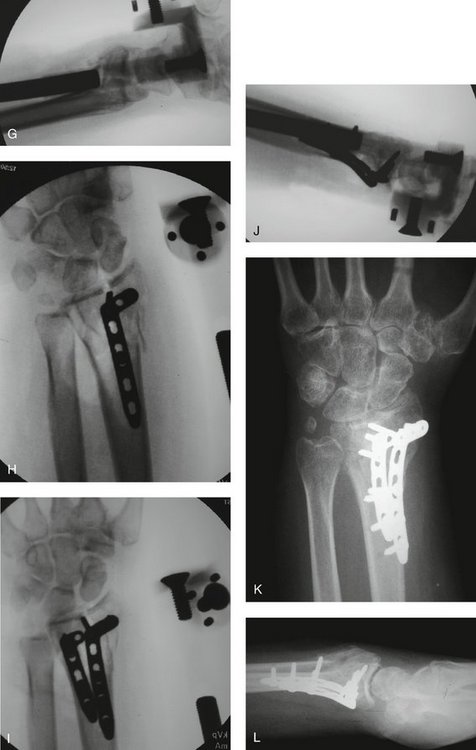
FIGURE 8-16 Volar Shear Fracture with Dorsal Comminution. A, Intra-articular fracture with marked radial shortening. B, Lateral x-ray shows a volar shear pattern with dorsal comminution. C, Anteroposterior CT scan reveals an undisplaced sagittal split of the volar articular fragment. D, Lateral CT scan highlights the marked periarticular dorsal comminution that precludes plate fixation. E, Coronal CT scan shows sigmoid notch disruption. F, Initial joint bridging external fixation clarifies the fracture anatomy. G, Ligamentotaxis alone does not reduce the articular incongruity. H, Volar locking plate applied to the radial column. I, Second volar plate applied to the intermediate column. J, Articular congruity is restored. K, Anteroposterior view at 8 weeks. L, Lateral view at 8 weeks.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
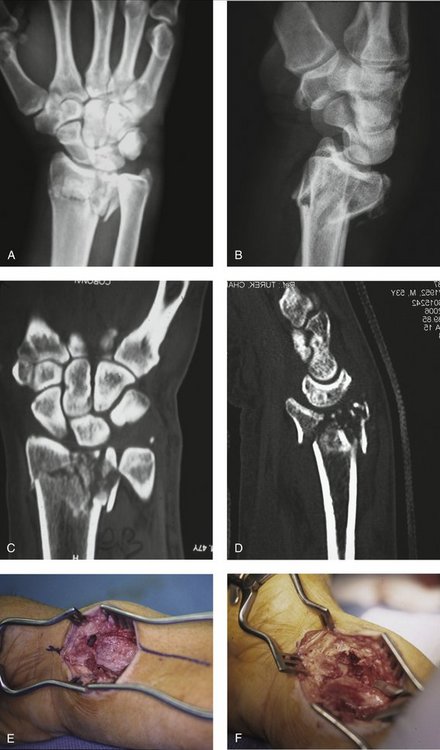
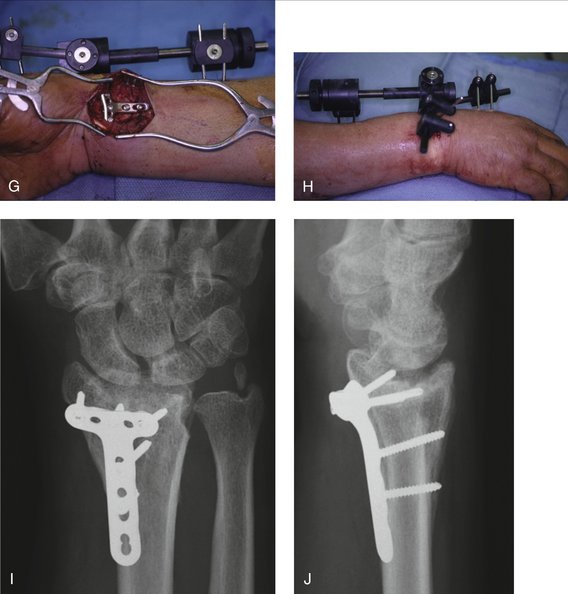
FIGURE 8-17 Joint Bridging External Fixation with Dorsal Outrigger. A, Comminuted intra-articular fracture. B, Marked dorsal tilt. C, Fragmentation of medial fragments. D, Sagittal split with periarticular dorsal comminution. E, Volar approach highlights the cortical comminution. F, Lunate is visible through the sagittal split. G, Volar plate application after bone grafting. H, Result at 6 months with congruous sigmoid notch and restored radial height. I, Anteroposterior view. J, Lateral view. Reasonable joint congruity, but some residual central depression.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)

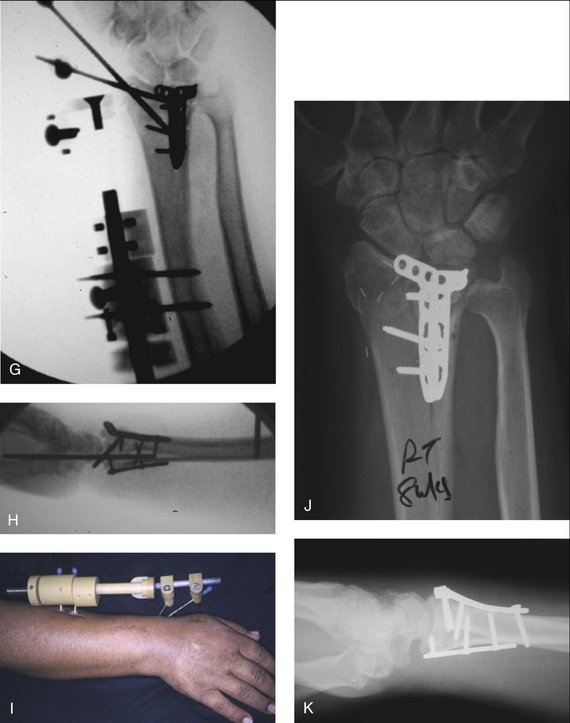
FIGURE 8-18 Volar Plating with Nonbridging External Fixation. A, Intra-articular fracture with metaphyseal extension. B, Depression and dorsal tilt of articular fragments. C, Fixation of palmar medial fragment; note distal screw does not engage the dorsal fragment yet. D, Restoration of sigmoid notch. E, Distraction with temporary joint bridging external fixation facilitates reduction of dorsal fragments. F, Fixator is applied in a nonbridging configuration. G, Anteroposterior view shows restoration of radial height and tilt. H, Lateral view shows reconstitution of joint surface “sandwiched” between volar and dorsal plates. I, Clinical appearance at 4 weeks. J, Anteroposterior view at 8 weeks. K, Maintenance of congruent joint after fixator removal.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
Indications
Despite the plethora of volar plate designs, fixation of a small radial styloid fragment is often tenuous. The Fragment Specific Fixator can be applied in a uniplanar radial application when there is a small radial styloid fragment that cannot be adequately captured with a plate. Any sagittal split of the medial fragment that cannot be successfully reduced with percutaneous or arthroscopic methods is treated with fragment-specific implants. Joint bridging fixation is indicated when there is central comminution to help unload the articular fragments.
Surgical Technique
Various authors have reported the use of joint bridging external fixation to facilitate fracture reduction and plate application.21,37 A joint bridging external fixator is applied in a standard fashion as described earlier. The volar medial fragment can be approached in many ways. A 3-cm volar ulnar incision is made along the ulnar border of the flexor tendons, which are retracted radially. The interposed tendons protect the median nerve, and working through the floor of the flexor tendons gains more distance from the ulnar neurovascular bundle. The pronator quadratus is identified and elevated from its ulnar insertion and then reflected radially. Some authors use an extended carpal tunnel approach, which simplifies exposure of the volar ulnar fragment. I prefer to use the standard flexor carpi radialis approach, and then use a broad periosteal elevator to retract the flexor tendons and expose the volar ulnar corner. Alternatively, the flexor carpi radialis approach can be combined with a volar ulnar approach through the same skin incision.
My preferred technique is first to reduce the volar medial fragment to the radial shaft and to the reduced radial styloid fragment. A unicortical locking pin is placed through the distal limb of an L-shaped 2-mm plate to engage the volar ulnar fragment; this allows one to control and reduce the fragment. The traction is released, and the proximal aspect of the plate is fixed to the radial shaft. The wrist is distracted again, and a dorsal approach through the third extensor compartment is performed. The EPL tendon is removed from its compartment and retracted. The fourth extensor compartment is elevated without disrupting the extensor tendons to gain access to the dorsomedial fragment. The dorsal cortex is typically quite comminuted and often can be opened like a book to expose the articular surface. Any tilted or depressed articular fragments are elevated and supported by subchondral structural bone graft. The dorsal cortex is folded back down and held in place with a dorsal 2-mm locking plate. It is not always possible to place more than one distal screw because of the small size of the fragments. Additional bicortical locking screws can now be applied, however, through the more proximal holes to “sandwich” the volar and dorsal medial fragments.
Complications
The complications are similar to those described earlier. There is a greater risk of hardware interference with tendon gliding and cutaneous nerve branches as the number of plates increases. The volar and dorsal exposure also may devascularize small fragments; this can lead to delayed healing or late collapse, which is the rationale for the use of locking plates rather than conventional mini-plates. In elderly patients with osteopenic bone, some fracture site settling cannot be avoided even after bone grafting, external fixation, and locking plates (Fig. 8-19).
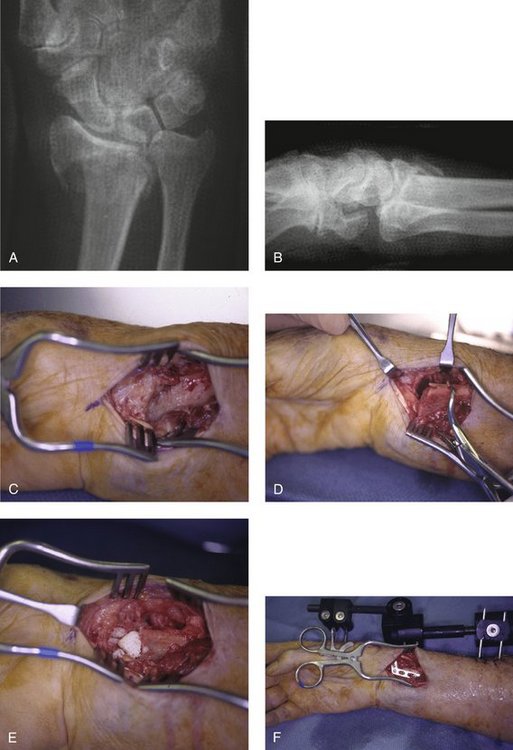
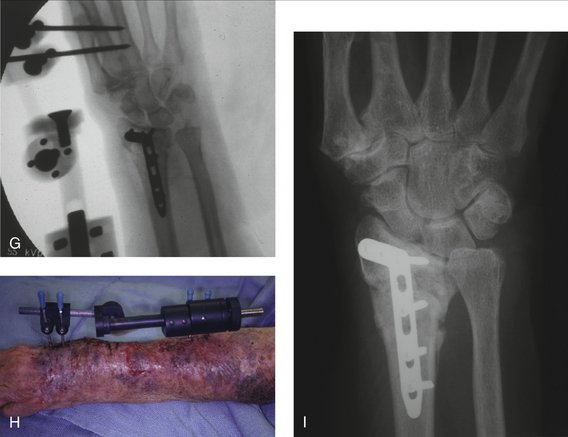
FIGURE 8-19 An 80-Year-Old Woman with Fragile Skin. A, Anteroposterior view of an unstable periarticular fracture with marked radial shortening. B, Lateral view highlights dorsal comminution and dorsal tilt. C, Volar approach to the fracture site. D, Pronation of the proximal radial shaft exposes the fracture. E, Allograft is packed into the metaphyseal defect. F, Neutralization plate is applied. G, External fixation restores 1-mm ulnar variance. H, Note the fragile skin envelope, which precludes a large dorsal dissection. I, Result at 3 months. Note the late settling at the fracture site despite external fixation, plating, and bone grafting, resulting in a 3-mm ulnar-positive variance, but preserved radial tilt.
(© South Bay Hand Surgery, LLC; 2007. Used by permission.)
1. Feipel V, Rinnen D, Rooze M. Postero-anterior radiography of the wrist: normal database of carpal measurements. Surg Radiol Anat. 1998;20:221-226.
2. Gausepohl T, Worner S, Pennig D, et al. Extraarticular external fixation in distal radius fractures pin placement in osteoporotic bone. Injury. 2001;32(Suppl 4):SD79-SD85.
3. Mackinnon SE, Dellon AL. The overlap pattern of the lateral antebrachial cutaneous nerve and the superficial branch of the radial nerve. J Hand Surg [Am]. 1985;10:522-526.
4. Emami A, Mjoberg B. A safer pin position for external fixation of distal radial fractures. Injury. 2000;31:749-750.
5. Woo SL, Gomez MA, Akeson WH. The time and history-dependent viscoelastic properties of the canine medial collateral ligament. J Biomech Eng. 1981;103:293-298.
6. Winemaker MJ, Chinchalkar S, Richards RS, et al. Load relaxation and forces with activity in Hoffman external fixators: a clinical study in patients with Colles’ fractures. J Hand Surg [Am]. 1998;23:926-932.
7. Sun JS, Chang CH, Wu CC, et al. Extra-articular deformity in distal radial fractures treated by external fixation. Can J Surg. 2001;44:289-294.
8. Bartosh RA, Saldana MJ. Intraarticular fractures of the distal radius: a cadaveric study to determine if ligamentotaxis restores radiopalmar tilt. J Hand Surg [Am]. 1990;15:18-21.
9. Agee JM. Distal radius fractures: multiplanar ligamentotaxis. Hand Clin. 1993;9:577-585.
10. Sanders RA, Keppel FL, Waldrop JI. External fixation of distal radial fractures: results and complications. J Hand Surg [Am]. 1991;16:385-391.
11. Juan JA, Prat J, Vera P, et al. Biomechanical consequences of callus development in Hoffmann, Wagner, Orthofix and Ilizarov external fixators. J Biomech. 1992;25:995-1006.
12. Rikli DA, Honigmann P, Babst R, et al. Intra-articular pressure measurement in the radioulnocarpal joint using a novel sensor: in vitro and in vivo results. J Hand Surg [Am]. 2007;32:67-75.
13. Wolfe SW, Austin G, Lorenze M, et al. A biomechanical comparison of different wrist external fixators with and without K-wire augmentation. J Hand Surg [Am]. 1999;24:516-524.
14. Seitz WHJr, Froimson AI, Leb R, et al. Augmented external fixation of unstable distal radius fractures. J Hand Surg [Am]. 1991;16:1010-1016.
15. Werber KD, Raeder F, Brauer RB, et al. External fixation of distal radial fractures: four compared with five pins: a randomized prospective study. J Bone Joint Surg Am. 2003;85:660-666.
16. Markiewitz AD, Gellman H. Five-pin external fixation and early range of motion for distal radius fractures. Orthop Clin North Am. 2001;32:329-335. ix
17. Braun RM, Gellman H. Dorsal pin placement and external fixation for correction of dorsal tilt in fractures of the distal radius. J Hand Surg [Am]. 1994;19:653-655.
18. Dunning CE, Lindsay CS, Bicknell RT, et al. Supplemental pinning improves the stability of external fixation in distal radius fractures during simulated finger and forearm motion. J Hand Surg [Am]. 1999;24:992-1000.
19. Wolfe SW, Swigart CR, Grauer J, et al. Augmented external fixation of distal radius fractures: a biomechanical analysis. J Hand Surg [Am]. 1998;23:127-134.
20. Bindra RR. Biomechanics and biology of external fixation of distal radius fractures. Hand Clin. 2005;21:363-373.
21. Rikli DA, Businger A, Babst R. Dorsal double-plate fixation of the distal radius. Oper Orthop Traumatol. 2005;17:624-640.
22. Papadonikolakis A, Shen J, Garrett JP, et al. The effect of increasing distraction on digital motion after external fixation of the wrist. J Hand Surg [Am]. 2005;30:773-779.
23. Kaempffe FA, Wheeler DR, Peimer CA, et al. Severe fractures of the distal radius: effect of amount and duration of external fixator distraction on outcome. J Hand Surg [Am]. 1993;18:33-41.
24. Baechler MF, Means KRJr, Parks BG, et al. Carpal canal pressure of the distracted wrist. J Hand Surg [Am]. 2004;29:858-864.
25. Margaliot Z, Haase SC, Kotsis SV, et al. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg [Am]. 2005;30:1185-1199.
26. Weil WM, Trumble TE. Treatment of distal radius fractures with intrafocal (Kapandji) pinning and supplemental skeletal stabilization. Hand Clin. 2005;21:317-328.
27. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg [Am]. 1991;16:375-384.
28. Kreder HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005;87:829-836.
29. Dicpinigaitis P, Wolinsky P, Hiebert R, et al. Can external fixation maintain reduction after distal radius fractures? J Trauma. 2004;57:845-850.
30. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19:325-340.
31. McQueen MM. Non-spanning external fixation of the distal radius. Hand Clin. 2005;21:375-380.
32. Salter RB, Simmonds DF, Malcolm BW, et al. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage: an experimental investigation in the rabbit. J Bone Joint Surg Am. 1980;62:1232-1251.
33. Mehta JA, Slavotinek JP, Krishnan J. Local osteopenia associated with management of intra-articular distal radial fractures by insertion of external fixation pins in the distal fragment: prospective study. J Orthop Surg (Hong Kong). 2002;10:179-184.
34. Slutsky DJ, Dai QG: Fragment specific external fixation of distal radius fractures. Presented at the American Society for Surgery of the Hand, 58th Annual Meeting. Chicago, IL. 2003.
35. Putnam MD, Meyer NJ, Nelson EW, et al. Distal radial metaphyseal forces in an extrinsic grip model: implications for postfracture rehabilitation. J Hand Surg [Am]. 2000;25:469-475.
36. Krishnan J, Chipchase LS, Slavotinek J. Intraarticular fractures of the distal radius treated with metaphyseal external fixation: early clinical results. J Hand Surg [Br]. 1998;23:396-399.
37. Gradl G, Jupiter JB, Gierer P, et al. Fractures of the distal radius treated with a nonbridging external fixation technique using multiplanar K-wires. J Hand Surg [Am]. 2005;30:960-968.
38. del Pinal F, Garcia-Bernal FJ, Pisani D, et al. Dry arthroscopy of the wrist: surgical technique. J Hand Surg [Am]. 2007;32:119-123.
39. Mehta JA, Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular fractures of the distal radius: an arthroscopically-assisted approach. J Bone Joint Surg Br. 2000;82:79-86.
40. Slutsky D. DRUJ arthroscopy and the volar ulnar portal. Tech Hand Up Extrem Surg. 2007;11:1-7.
41. Atzei AL, Carità E, Papini Zorli I, et al. Arthroscopically assisted foveal reinsertion of peripheral avulsions of the TFCC. J Hand Surg [Br]. 2005;30:40.