CHAPTER 315 Evaluation and Treatment of Odontoid and Hangman’s Fractures
The estimated annual incidence of spinal cord injury in the United States, not including those who die at the scene, is approximately 12,000 new cases each year.1 The cervical spine is affected in more than 60% of spinal injuries.2 Cervical spine injury occurs in 1.5% of injured children,3 and 53% of these injuries are related to motor vehicles: motor vehicle crashes, 31%; pedestrian versus motor vehicle, 16%; and bicycle versus motor vehicle, 6%.4 The mortality rate for these injuries ranges from 25% to 50%.4,5 In the elderly, falls are the most common cause of cervical spine injury. Since 2000, the incidence of persons older than 60 years at time of injury has increased to 11.5%, as opposed to 4.7% before 1980.1
Approximately 9% to 20% of all cervical fractures are dens fractures,2,6–10 with most (65% to 74%) being type II fractures.2,9,10 C2 fractures are classified as odontoid fractures involving the dens; Hangman’s fractures, a traumatic spondylolisthesis through the pars interarticularis; and miscellaneous fractures, including facet fractures or injury through the foramen transversarium. These injuries may be missed clinically because of the lack of clinical signs except for neck pain. Os odontoideum and fractured calcified pannus may mimic acute C2 fractures.
Anatomy
The anatomy of the axis is unique in that it forms a connection with the mobile upper cervical spine and cranium and the lower cervical spine. This anatomy consists of the axis, atlas, odontoid process, occipital condyles, C2-3 disk, C1-2 facet joints, synovium of the occipital condyles, and the ligaments that attach to C1, C2, and the skull.11 Because the weight of the cranium is transmitted from a relatively lateral and posterior position to a medial and anterior position at C2, the axis is referred to as a transitional vertebra. The atlantoaxial complex is configured to allow much more rotational movement than in any other segment. Approximately 50% of the rotational movement of the entire spine takes place at C1-2; fusion of this segment would cause this motion to be lost. The atlantoaxial joints also allow about 50 degrees of axial rotation and 10 degrees of flexion-extension.
Other noteworthy features of the C1-2 joint include the absence of a true intervertebral disk and relatively loose capsular ligaments,12 evolution of the ligamentum flavum into a weaker atlantoaxial membrane, a rich blood supply from branches of the vertebral and carotid arteries, and an increased spinal canal diameter.13 The odontoid process is held tightly to the anterior portion of the C1 ring by the strong transverse ligament, which prevents subluxation in the sagittal plane. There is also close apposition of the spinal cord to the axis of rotation, which minimizes the torsional forces on the spinal cord that would be present if the cord were located more posteriorly. All these adaptations combine to make a highly mobile yet stable connection between the skull and the spine.
Odontoid Fractures
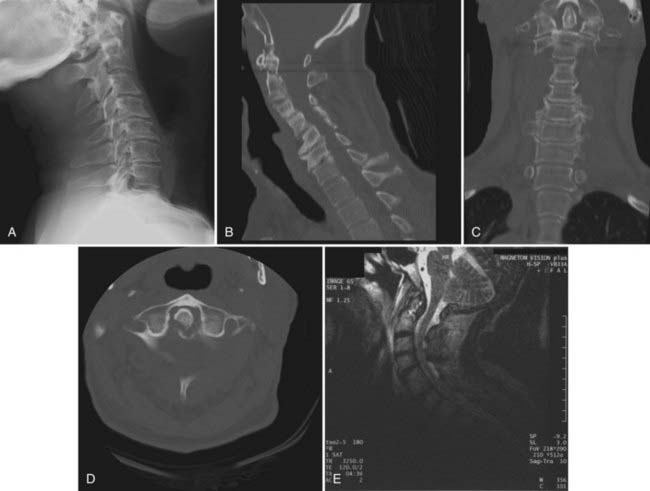
The treatment of odontoid fractures has long been a topic of debate. They are the most common and potentially most devastating of all axis fractures. Many classification schemes for odontoid fractures have been proposed, but the most commonly used is that described by Anderson and D’Alonzo in 1974.9 This scheme classifies odontoid fractures by anatomic location. Type I fractures involve an avulsion fracture of the tip of the odontoid and are thought to occur as a result of rotation and lateral flexion, which causes injury to the alar ligaments. Type II fractures are the most common and potentially the most dangerous and occur as a transverse fracture across the base of the odontoid process, just superior to the body of the axis. About 15% of these patients will have neurological injury; these fractures are unstable and require some type of immobilization. In 1988, a new subtype of odontoid fracture (type IIA) was described that involves comminution at the base of the dens.14 Type III fractures traverse the body of the axis. These fractures usually heal with nonoperative treatment (Fig. 315-1).
Type I Fractures
Type I fractures are rare and traditionally have been thought to be stable and thus managed nonoperatively.15 The mechanism of the injury is considered to be avulsion of one of the alar ligaments.16 The fracture plane is often cephalad to the transverse ligament and therefore does not cause a violation of ligamentous continuity. Several recent reports have noted that this avulsion may lead to atlanto-occipital dislocation and may therefore be unstable (see also Chapter 313).6,17 A thorough examination of this subject is difficult because of the paucity of cases in the literature; analysis of previous reviews indicates that type I fractures account for 0.82% of all odontoid fractures.18 Thin-cut computed tomography (CT) scans with sagittal and coronal reconstruction are the optimal method for radiologic evaluation; magnetic resonance imaging (MRI) or flexion-extension radiographs may be useful if instability is an issue.19 There are reports of ossiculum terminale being mistaken for a type I fracture.20,21 This entity is a congenital nonunion of the tip of the dens held in place by a firm segment of cartilage.
Type II Fractures
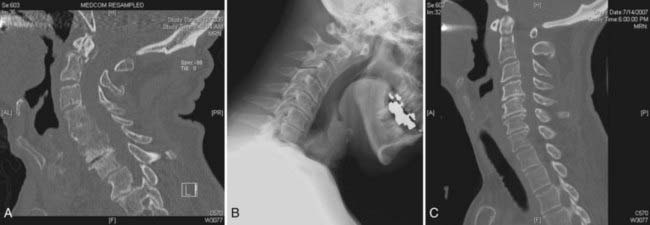
Type II fractures, which occur at the base of the dens, are by far the most common odontoid fractures seen in clinical practice.22 They are generally believed to be unstable; however, controversy exists regarding optimal management of these injuries.19,23 Many articles in the past have documented nonsurgical treatment by external immobilization, with reported nonunion rates ranging from 10% to 88%.2,24–27 There has been much debate whether internal fixation, either by odontoid screw or posterior screw fixation, should be the primary treatment modality or should be reserved for patients who fail external immobilization. Several reports have also described fracture mimicry attributable to os odontoideum28 or fractures of calcified pannus formation. These imposters must be actively searched for because they may result in inappropriate intervention. In addition, one must be sensitive to the loss of structural properties in the aged population secondary to osteoporosis or osteomalacia, which can make fractures difficult to identify (Fig. 315-2). Recently published literature has also brought attention to the increasing number of reported fractures associated with ankylosing spondylitis, disseminated idiopathic hypertrophic arthropathy, and end-stage degenerative spondylosis,29,30 all of which can lead to functional cervical ankylosis over time and an increased risk for fractures with even minor trauma. A refined evaluation protocol for at-risk patients using reformatted CT scans has decreased the likelihood of missed injuries and assists in treatment decisions.
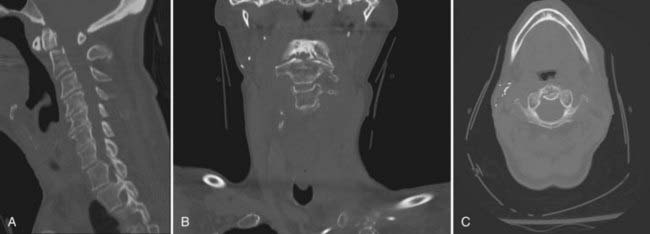
FIGURE 315-2 A-C, Reformatted computed tomography (CT) scans showing a type II dens fracture missed on plain radiographs.
Nonsurgical Management of Type II Fractures
Nonsurgical treatment of type II odontoid fractures consists of either rigid collar fixation or halo immobilization. Halo-vest treatment has been shown to limit upper cervical motion by 75% versus 45% with a collar.31 The drawbacks with halo immobilization are many, including economic, social, pin site infections, skin breakdown, skull perforation, and overall nonunion on the order of about 32%.2,6,24,26,32–40
Several studies have attempted to characterize the risk factors involved in nonunion of type II fractures. Platzer and colleagues found that 75 of 90 patients returned to their preinjury activity level and were satisfied with halo–thoracic vest treatment. Successful fracture healing was achieved in 84% of patients undergoing this treatment. Cases in which nonunion was demonstrable on radiographs or CT scans within 6 to 12 months after trauma were attributed to increased age or greater dens displacement.24
Seybold and Bayley found a 65% overall fusion rate with halo immobilization and no significant difference in outcome in patients older than 60 years, in patients younger than 60 years, or by degree of displacement.41 Greene and colleagues reviewed 340 acute axis fractures and identified two categories of unstable type II fractures, which they recommended be treated by early surgical fusion. The first involves dens displacement of 6 mm or greater, and the second involves comminution of the dens.42 Hadley and coworkers found a 67% nonunion rate in patients with 6-mm or greater subluxation as opposed to a 9% nonunion rate in those with lesser degrees of displacement. They failed to find any correlation between a patient’s age or direction of subluxation.43–45 Dunn and Seljeskog found an increased risk for nonunion with conservative management in patients older than 65 years and in those with posteriorly displaced odontoid fragments. They reported a nonunion rate of 70% with retrolisthesis versus 30% with anterolisthesis.46
Because of these risk factors for nonunion (age >65 years, >6-mm displacement, posterior displacement), surgical management evolved as an appropriate treatment modality. Indications for surgery include irreducible or unstable fracture for which reduction is impossible; significant neurological deficit; previous nonunion; prolonged delay in treatment; injuries that preclude halo placement, including skull fractures and chest or facial injuries; and patients at high risk for nonunion, including the elderly and debilitated.47–49
Surgical management of these injuries can be approached either anteriorly or posteriorly. Posterior approaches involve the use of wire or cable, clamps, or direct screw fixation.50 These techniques involve C1-2 fusion and loss of motion at this joint. Loss of rotary motion at C1-2 is usually in the 50% range.51,52 Anterior procedures involve direct screw fixation across the fracture line. Traynelis and associates performed an evidence-based review of posterior bone and wire fixation of odontoid fractures and noted an overall success rate of 64%, with the morbidity and mortality rate approaching 2%.53,54 A variety of bone and wire fusion techniques have been described, including the Gallie (midline graft with a single wire), Brooks (bilateral sublaminar wires), and Sonntag (interspinous) methods. These techniques create a posterior tension band. Although successful, these techniques are not strong in extension and axial rotation. To overcome these deficiencies, Magerl described the technique of transarticular C1-2 fixation.76–78 This method involves screw fixation through the lateral joints of C1-2. Extensive preoperative planning is required to determine the course of the vertebral arteries because they may be injured by the trajectory of the screw. Harms and Melcher recently described a construct consisting of direct lateral mass screw fixation of C1 and pars or pedicle screw fixation of C2.58 This technique has proved to be biomechanically sound and technically easier than transarticular fixation, does not require the use of midline bone grafts, and can be performed despite C1 laminectomy.
Because of the potential morbidity and loss of motion with posterior C1-2 fusion, the use of anterior screw fixation for type II odontoid fractures has become increasingly popular. This technique provides immediate stabilization; we have performed this procedure and often discharged the patient the next day. The first reports of odontoid fixation were reported by Nakanishi in 198059 and Bohler in 1982.60 These early reports involved extensive neck dissection and were not widely adopted.
As surgical techniques became more refined, direct anterior screw fixation of C2 fractures has become more popular, and many clinicians now consider this procedure to be the treatment of choice for these injuries. Fusion rates in several series have ranged from 79% to 100%, with acceptably low morbidity.25,27,61–64 Apfelbaum and coworkers reviewed their series of 147 patients who underwent anterior screw fixation and found an overall fusion rate of 77%, which rose to 88% with acute fractures.65 An analysis of patient factors noted that fracture orientation was the only significant variable that affected fusion rates. Fractures with anterior oblique orientation were more likely to be associated with fusion failure or fibrous union than were posterior oblique or horizontal fractures. The two most common hardware failures were screw backout and screw pullout. Screws that backed out were associated with lack of engagement of the distal cortex of the odontoid tip. Screws pulled out of the body of C2 in patients who had fractures that involved the C2 body. Current recommendations are posterior stabilization for severely comminuted fractures of the body of C2. Platzer and coauthors recently reported a series of 79 patients who underwent anterior screw fixation and found that patients younger than 65 years had better outcomes than those older than 65.25
Indications for Anterior Odontoid Screw Fixation
As noted earlier, most patients with acute type II fractures are candidates for anterior screw fixation. This approach allows direct fixation across the fracture line and provides immediate stabilization of the injury while maintaining motion at the C1-2 joint. Contraindications to this technique include rupture of the transverse ligament (which can be assessed with MRI) and significant comminution of the C2 body. Relative contraindications include osteopenia, which affects pullout strength of the screw, and anterior obliquely sloping fractures, which can allow the odontoid process to slide along the fracture line as the screw pulls it inferiorly. This tends to be less of an issue with acute fractures but is more important with fractures more than several weeks old. Apfelbaum and coworkers noted that anterior screw fixation can generally be performed for fractures up to 6 months old; in patients with chronic nonunion, scar tissue develops and makes screw passage difficult.65 Patients with contraindications to anterior screw fixation are optimally treated with transarticular screw fixation or the Harms C1-2 technique. Patients with type III odontoid fractures and ruptured transverse ligaments are also best treated with a posterior procedure; if the ligament is intact but there is motion at the fracture site, anterior screw fixation can be considered.
Anterior Odontoid Screw Fixation
Several authors have described anterior C2 osteosynthesis in detail; for a more detailed description of the procedure, the reader is referred to other sources.24,25,63,65–68
At this point in the procedure, cannulation of the fracture can begin. Two similar techniques have been described—the cannulated screw technique and the standard lag screw technique. In the cannulated screw technique, the C2-3 anulus is opened as the starting point for drilling, and a Kirschner wire (K wire) is inserted at the anterior lip of C2 in a sagittal direction such that it is angled posteriorly and exits the posterior tip of the odontoid. AP fluoroscopy is useful to ensure that the K wire is in the midline, and a lateral view ensures the appropriate trajectory. A drill guide system is placed over the K wire once the pilot hole has been made. The drill is now passed through the body of C2 to the fracture line, and after the surgeon is assured that the spine remains aligned, a hole is drilled to and then through the posterior apex of the odontoid. The drill is removed, the pilot hole is tapped, and a lag screw is inserted through the guide tube through the fracture. It should be emphasized that frequent imaging is useful in achieving optimal trajectory through the fracture. In the lag screw technique, a drill bit is inserted into the anterior edge of C2, and a hole is drilled without the use of a K wire. A screw is then inserted through the drill guide. A hand drill or power drill can be used. Biomechanical studies have shown that one screw is as stable as two screws.7,25,65,69,70–72
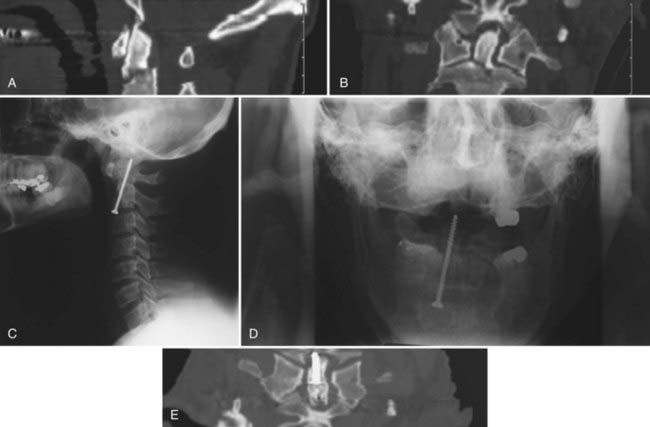
The wound is closed in standard fashion. We often place the patient in a collar for 4 to 6 weeks. The patient is usually discharged within 48 hours. Several studies have documented the high rate of healing and low morbidity of this operation65,72–75; it is possible that direct anterior screw fixation of odontoid fractures will become the treatment of choice in young patients with acute type II fractures (Fig. 315-3).
Transarticular Screw Placement for C2 Fractures
Transarticular screw fixation of C1-2, originally described by Magerl and Seemann,76 is a useful surgical technique in patients who are not candidates for anterior C2 screw fixation.17,77–81 Such patients include those with poor bone stock, such as the elderly (Fig. 315-4); patients whose fractures are older than 6 months; and patients with an injured transverse ligament. The procedure is technically more challenging than anterior C2 surgery and necessitates an intact C1 arch because interspinous wiring is also required to ensure long-term stabilization.67,81
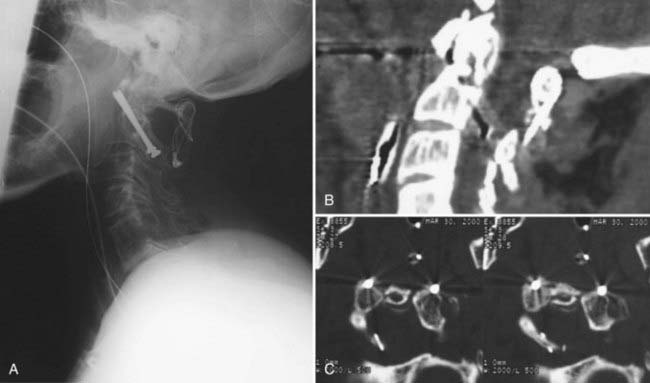
Once both transarticular screws have been placed, C1-2 interspinous wiring and bony fusion should be performed (Fig. 315-5). This can be done with the Brooks or Sonntag method and increases the stability of the construct so that bony fusion can take place. Bone graft can also be placed in the lateral gutters.82
Posterior C1-2 Screw-Rod Fixation
Posterior C1-2 screw-rod fixation overcomes some of these limitations. First described by Harms and Melcher,58 this procedure involves bilateral placement of screws with polyaxial heads into the C2 pedicles and lateral masses of C1 (Fig. 315-6). Fluoroscopy may be necessary to assess reduction of the subluxation and final screw placement.
Once C1 and C2 have been adequately exposed, the dorsal root ganglion of C2 can be retracted downward. This maneuver exposes the entry point of C1, which is the middle of the lateral mass, halfway between the arch of C1 and the C1-2 joint. Occasionally, the arch of C1 may need to be drilled off or removed with a Kerrison punch to expose the entry point. A high-speed drill is used to break through the cortex, and then a hole is drilled with a drill and drill guide. The direction is slightly medial and parallel to the C1 arch.83 Lateral fluoroscopy is useful for defining the trajectory; the ultimate target is the anterior cortex of the C1 lateral mass. An appropriate-length screw is placed bicortically once the hole is tapped. The screw is only partially threaded because there will be some length of the screw not engaged in C1.
Harms and Melcher reported on their series of 37 patients treated over a 3-year period.58 Half of these patients were operated on for trauma, and no neural or vascular complications were reported.
Odontoid Fractures in the Elderly
The population older than 85 years is the fastest growing demographic group in the United States and is expected to double over the next 17 years.84 Odontoid fractures are the most common cervical spine fracture in patients 70 years and older2,6 and the most common of all spinal fractures in patients 80 years and older.6,85
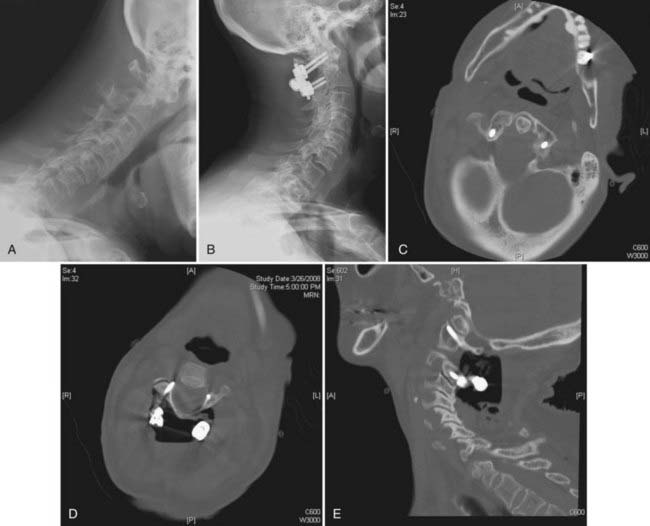
With the aging of America’s population, the increase in C2 fractures has and will probably continue to increase; the comorbid conditions of these patients will continue to present new challenges to the practicing spine care professional.26,84,86–89 The long-held dogma of surgical intervention or halo immobilization has recently been challenged by those who have chosen to use a rigid collar and close follow-up to treat elderly patients with multiple comorbid conditions.87 Studies have shown that in a significant percentage of these patients, a fibrous bridge forms between the base of the dens and the displaced portion of the odontoid process.65 The decision to use rigid or soft collar versus halo immobilization comes in light of reports demonstrating pulmonary complications and loss of fracture alignment in those treated by primary operative fixation (Fig. 315-7).90 Several reports have shown higher mortality with halo immobilization in this group of patients that has been attributed to pneumonia and cardiac or respiratory failure than in those treated with a rigid collar.6,86 Conversely, Frangen and colleagues have shown in a recent paper that dorsal C1-2 fusion for stabilization of type II odontoid fractures with transarticular screws in older patients can be performed with good clinical results and lower mortality than reported after treatment with halo immobilization alone.26 The decision to operate or treat a patient with halo versus collar immobilization continues to be a difficult one.
Hangman’s Fracture
Hangman’s fracture, or traumatic spondylolisthesis of the axis, has been described in the literature for more than 100 years.91,92 It is the second most common type of axis fracture.93,94 Wood-Jones described a series of five hanging victims and noted a fracture separating the posterior arch of C2 from the C1-2 complex.95 In 1954, Grogono noted a similar fracture pattern in a patient involved in a motor vehicle collision.96 This injury was further described by Schneider and associates97 and given the name hangman’s fracture, a bilateral fracture through the pars interarticularis of the axis.
This injury is caused by distraction or compression while the neck is hyperextended. Schneider noted that the weight of the skull is transmitted through the occipital condyles and the C1-2 lateral masses, where it converges at the base of C2; it then passes through to the weak pars.97 Hyperextension causes a distracting force on the disk and anterior longitudinal ligament while simultaneously compressing the posterior facets, which causes a fracture of the pars and rupture of the disk and anterior longitudinal ligament. Autopsy studies have confirmed this mechanism of injury.
Most patients have nonspecific neck pain. Less than 10% have neurological injury because the spinal canal is widened after the injury.98,99 Almost a third of these patients will have other spine injuries, and a significant number will sustain associated head, chest, or facial trauma.100,101
The most commonly used classification of hangman’s fractures is the Levine and Edwards’ modification102 of the system of Effendi and colleagues.101 In this scheme there are four types of fractures. Type I fractures are bilateral pars interarticularis fractures with less than 3 mm of displacement of C2 on C3 and no angulation. Type II fractures have greater than 3 mm of displacement and angulation of C2 on C3. Type IIA fractures have severe angulation but little or no displacement. This is associated with disk disruption and injury to the posterior longitudinal ligament. Type III fractures are injuries with increased subluxation and angulation and also have unilateral or bilateral facet dislocation along with injury to the posterior and anterior ligaments. Starr and Eismont described a type II variant consisting of the fracture line extending through the posterior cortex of the C2 body.103 These patients have a high incidence of neurological deficit (33%). Types III and IIA are the rarest of these injuries but the most likely to be unstable.103
Radiographic evaluation of hangman’s fractures includes plain radiographs, CT scans, and MRI to evaluate the injured ligaments (Fig. 315-8).
As noted earlier, most hangman’s fractures are not associated with neurological injury and can be treated nonsurgically.104 Most type I fractures can be treated with a rigid collar; in several large series there was a low rate of nonhealed fractures.42,45,100,105 Some authors have advocated the use of halo immobilization for type II fractures if they can be reduced with traction.33 Nonreducible type II and type III fractures (which are difficult to reduce) often require surgical management, as do nonunions. If surgery is required, options include posterior or anterior approaches. Some authors have recommended posterior C2-3 fusion,93,106,107 but this may serve to narrow the spinal canal because the angulation is not adequately addressed. An anterior C2-3 approach frequently suffices to treat these injuries (Fig. 315-9).
Miscellaneous C2 Fractures
Included in this category are nonodontoid, non-hangman’s fractures. These injuries occur infrequently, and no universal classification system exists to adequately categorize them. Most of these fractures are managed nonoperatively unless instability exists. Generally speaking, these fractures are grouped into four basic types: vertebral body fractures, lamina fractures, spinous process fractures, and lateral mass fractures. Benzel and coworkers described two types of vertical C2 body fractures and a horizontal rostral body fracture. No treatment recommendations were offered.108 Fujimura and colleagues described four types of C2 body fractures: sagittal, transverse, burst, and avulsion. All patients in this series were managed nonoperatively.109
Finally, in the largest series of miscellaneous C2 fractures, Greene and associates found only 1 patient (out of 67) who required surgical management for nonunion. All patients in this series were managed initially with external immobilization.42
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663-1674.
Apfelbaum RI, Lonser RR, Veres R, et al. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(2 suppl):227-236.
Aydinli U, Kara GK, Ozturk C, et al. Surgical treatment of odontoid fractures with C1 hook and C2 pedicle screw construct. Acta Orthop Belg. 2008;74:276-281.
Benzel EC, Hart BL, Ball PA, et al. Fractures of the C2 vertebral body. J Neurosurg. 1994;81:206-212.
Chapman J, Bransford R. Geriatric spine fractures: an emerging healthcare crisis. J Trauma. 2007;62(6 suppl):S61-S62.
Coric D, Wilson JA, Kelly DLJr. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85:550-554.
Duggal N, Chamberlain RH, Perez-Garza LE, et al. Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine. 2007;32:182-187.
Fielding JW, Francis WRJr, Hawkins RJ, et al. Traumatic spondylolisthesis of the axis. Clin Orthop Relat Res. 1989;239:47-52.
Frangen TM, Zilkens C, Muhr G, et al. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. 2007;63:83-89.
Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: analysis of management and outcomes in 340 consecutive cases. Spine. 1997;22:1843-1852.
Hadley MN, Browner CM, Liu SS, et al. New subtype of acute odontoid fractures (type IIA). Neurosurgery. 1988;22:67-71.
Hadley MN, Browner C, Sonntag VK. Axis fractures: a comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985;17:281-290.
Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467-2471.
Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464-475.
Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217-226.
Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman’s fractures. Eur Spine J. 2006;15:257-269.
Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 2006;31(11 suppl):S53-S60. discussion S61
Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(suppl 2):B54-B64.
Platzer P, Thalhammer G, Oberleitner G, et al. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89:1716-1722.
Platzer P, Thalhammer G, Ostermann R, et al. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714-1720.
Platzer P, Thalhammer G, Sarahrudi K, et al. Nonoperative management of odontoid fractures using a halothoracic vest. Neurosurgery. 2007;61:522-529. discussion 529-530
Schneider RC, Livingston KE, Cave AJ, et al. “Hangman’s fracture” of the cervical spine. J Neurosurg. 1965;22:141-154.
Starr JK, Eismont FJ. Atypical hangman’s fractures. Spine. 1993;18:1954-1957.
Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation: technical description and report of 22 cases. Neurosurgery. 1993;32:948-954. discussion 954-955
1 National Spinal Cord Injury Statistical Center, funded by the National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitative Services, US Department of Education, Washington, DC.
2 Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(suppl 2):B54-B64.
3 Patel JC, Tepas JJIII, Mollitt DL, et al. Pediatric cervical spine injuries: defining the disease. J Pediatr Surg. 2001;36:373-376.
4 Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg. 2001;36:1107-1114.
5 Bracken MB, Freeman DHJr, Hellenbrand K. Incidence of acute traumatic hospitalized spinal cord injury in the United States, 1970-1977. Am J Epidemiol. 1981;113:615-622.
6 Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 2006;31(11 suppl):S53-S60. discussion S61
7 Subach BR, Monroe MA, Haid RW, et al. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45:812-819. discussion 819-820
8 Vaccaro AR, Madigan L, Ehrler DM. Contemporary management of adult cervical odontoid fractures. Orthopedics. 2000;23:1109-1113.
9 Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663-1674.
10 Clark CR, White AA. Fractures of the dens: a multicenter study. J Bone Joint Surg Am. 1985;67:1340-1348.
11 Schaffler MB, Alson MD, Heller JG, et al. Morphology of the dens: a quantitative study. Spine. 1992;17:738-743.
12 Dvorak J, Schneider E, Saldinger P, et al. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6:452-461.
13 Amling M, Hahn M, Wening VJ, et al. The microarchitecture of the axis as the predisposing factor for fracture of the base of the odontoid process. A histomorphometric analysis of twenty-two autopsy specimens. J Bone Joint Surg Am. 1994;76:1840-1846.
14 Hadley MN, Browner CM, Liu SS, et al. New subtype of acute odontoid fractures (type IIA). Neurosurgery. 1988;22:67-71.
15 Francavilla TL, Melisi J, Chappell ET, et al. Type I odontoid fractures. Neurosurgery. 1989;25:481.
16 Scott EW, Haid RWJr, Peace D. Type I fractures of the odontoid process: implications for atlanto-occipital instability. Case report. J Neurosurg. 1990;72:488-492.
17 Grob D. Transarticular screw fixation for atlanto-occipital dislocation. Spine. 2001;26:703-707.
18 Yanagawa Y, Takemoto MA, Takasu A, et al. Type I odontoid fracture—case report. Neurol Med Chir (Tokyo). 2005;45:92-96.
19 Dickman CA, Mamourian A, Sonntag VK, et al. Magnetic resonance imaging of the transverse atlantal ligament for the evaluation of atlantoaxial instability. J Neurosurg. 1991;75:221-227.
20 Strohm PC, Muller CA, Bley TA, et al. Ossiculum terminale (Bergmann). [Differentialdiagnose einer Densfraktur vom Typ Anderson I]. Unfallchirurg. 2003;106:1054-1056.
21 Liang CL, Lui CC, Lu K, et al. Atlantoaxial stability in ossiculum terminale. Case report. J Neurosurg. 2001;95(suppl 1):119-121.
22 Pointillart V, Orta AL, Freitas J, et al. Odontoid fractures. Review of 150 cases and practical application for treatment. Eur Spine J. 1994;3:282-285.
23 Maiman DJ, Larson SJ. Management of odontoid fractures. Neurosurgery. 1982;11:820.
24 Platzer P, Thalhammer G, Sarahrudi K, et al. Nonoperative management of odontoid fractures using a halothoracic vest. Neurosurgery. 2007;61:522-529. discussion 529-530
25 Platzer P, Thalhammer G, Ostermann R, et al. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714-1720.
26 Frangen TM, Zilkens C, Muhr G, et al. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. 2007;63:83-89.
27 Lee SH, Sung JK. Anterior odontoid fixation using a 4.5-mm Herbert screw: the first report of 20 consecutive cases with odontoid fracture. Surg Neurol. 2006;66:361-366. discussion 366
28 Kaya RA, Turkmenoglu O, Cavusoglu H, et al. Os odontoideum: a case report. Turk Neurosurg. 2005;15:157-161.
29 Ozgocmen S, Ardicoglu O. Odontoid fracture complicating ankylosing spondylitis. Spinal Cord. 2000;38:117-119.
30 Strohm PC, Zwingmann J, Bley TA, et al. [Injuries of the cervical spine with Forestier’s disease. Problems in the diagnostic and surgical management.]. Unfallchirurg. 2006;109:905-909.
31 Johnson RM, Hart DL, Simmons EF, et al. Cervical orthoses. A study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg Am. 1977;59:332-339.
32 Strohm PC, Bley TA, Ghanem N, et al. Clinical and radiological findings after different treatment of odontoid fractures type Anderson II and III. Acta Chir Orthop Traumatol Cech. 2006;73:151-156.
33 Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001;121:50-55.
34 Buchholz RD, Cheung KC. Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg. 1989;70:884-892.
35 Ekong CE, Schwartz ML, Tator CH, et al. Odontoid fracture: management with early mobilization using the halo device. Neurosurgery. 1981;9:631-637.
36 Hossain M, McLean A, Fraser MH. Outcome of halo immobilisation of 104 cases of cervical spine injury. Scott Med J. 2004;49:90-92.
37 Majercik S, Tashjian RZ, Biffl WL, et al. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350-356. discussion 356-358
38 Müller EJ, Wick M, Muhr G. [Subdural abscess as a complication of halo fixator.]. Unfallchirurg. 1998;101:655-657.
39 Müller EJ, Schwinnen I, Fischer K, et al. Non-rigid immobilisation of odontoid fractures. Eur Spine J. 2003;12:522-525.
40 Papagelopoulos PJ, Sapkas GS, Kateros KT, et al. Halo pin intracranial penetration and epidural abscess in a patient with a previous cranioplasty: case report and review of the literature. Spine. 2001;26:E463-E467.
41 Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine. 1998;23:1837-1846.
42 Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: analysis of management and outcomes in 340 consecutive cases. Spine. 1997;22:1843-1852.
43 Hadley MN, Browner C, Sonntag VK. Axis fractures: a comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985;17:281-290.
44 Hadley MN, Dickman CA, Browner CM, et al. Acute traumatic atlas fractures: management and long term outcome. Neurosurgery. 1988;23:31-35.
45 Hadley MN, Dickman CA, Browner CM, et al. Acute axis fractures: a review of 229 cases. J Neurosurg. 1989;71:642-647.
46 Dunn ME, Seljeskog EL. Experience in the management of odontoid process injuries: an analysis of 128 cases. Neurosurgery. 1986;18:306-310.
47 Garfin SR, Botte MJ, Waters RL, et al. Complications in the use of the halo-fixation device. J Bone Joint Surg Am. 1986;68:320-325.
48 Koivikko MP, Kiuru MJ, Koskinen SK, et al. Factors associated with nonunion in conservatively-treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004;86:1146-1151.
49 Saeed MU, Dacuycuy MA, Kennedy DJ. Halo pin insertion-associated brain abscess: case report and review of literature. Spine. 2007;32:E271-E274.
50 Dickman CA, Sonntag VKH, Papadopoulos SM, et al. The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991;74:190-198.
51 Jeanneret B, Vernet O, Frei S, et al. Atlantoaxial mobility after screw fixation of the odontoid: a computed tomographic study. J Spinal Disord. 1991;4:203-211.
52 White AAIII, Panjabi MM. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop Clin North Am. 1978;9:867-878.
53 Traynelis VC. Evidence-based management of type II odontoid fractures. Clin Neurosurg. 1997;44:41-49.
54 Lennarson PJ, Mostafavi H, Traynelis VC, et al. Management of type II dens fractures: a case-control study. Spine. 2000;25:1234-1237.
55 Härtl R, Chamberlain RH, Fifield MS, et al. Biomechanical comparison of two new atlantoaxial fixation techniques with C1-2 transarticular screw-graft fixation. J Neurosurg Spine. 2006;5:336-342.
56 Henriques T, Cunningham BW, Olerud C, et al. Biomechanical comparison of five different atlantoaxial posterior fixation techniques. Spine. 2000;25:2877-2883.
57 Hott JS, Lynch JJ, Chamberlain RH, et al. Biomechanical comparison of C1-2 posterior fixation techniques. J Neurosurg Spine. 2005;2:175-181.
58 Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467-2471.
59 Nakanishi T. Internal fixation of odontoid fracture. Orthop Trauma Surg. 1980;23:399-406.
60 Bohler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982;64:18-27.
61 Aydinli U, Kara GK, Ozturk C, et al. Surgical treatment of odontoid fractures with C1 hook and C2 pedicle screw construct. Acta Orthop Belg. 2008;74:276-281.
62 Platzer P, Thalhammer G, Oberleitner G, et al. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89:1716-1722.
63 Song KJ, Lee KB, Kim KN. Treatment of odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2007;14:824-830.
64 Etter C, Coscia M, Jaberg H, et al. Direct anterior fixation of dens fractures with a cannulated screw system. Spine. 1991;16(3 suppl):S25-S32.
65 Apfelbaum RI, Lonser RR, Veres R, et al. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(2 suppl):227-236.
66 Eck JC, Walker MP, Currier BL, et al. Biomechanical comparison of unicortical versus bicortical C1 lateral mass screw fixation. J Spinal Disord Tech. 2007;20:505-508.
67 York JE, Klimo P, Apfelbaum RI. Treatment of axis fractures. In: Winn HR, editor. Youmans Neurological Surgery. 5th ed. Philadelphia: WB Saunders; 2004:4939-4949.
68 Apfelbaum RI. Anterior screw fixation of odontoid fractures. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas, Vol. 2. Park Ridge IL: AANS Publication Committee; 1995:189-199.
69 Ames CP, Crawford NR, Chamberlain RH, et al. Biomechanical evaluation of a bioresorbable odontoid screw. J Neurosurg Spine. 2005;2:182-187.
70 Aebi M, Thalgott JS, Webb JK. Stabilization techniques: upper cervical spine. In: Aebi M, Thalgott JS, Webb JK, editors. AO ASIF Principles in Spine Surgery. New York: Springer-Verlag; 1998:42-53.
71 Montesano PX, Anderson PA, Schlehr F, et al. Odontoid fractures treated by anterior odontoid screw fixation. Spine. 1991;16(3 suppl):S33-S37.
72 Rainov NG, Heidecke V, Burkert W. Direct anterior fixation of odontoid fractures with a hollow spreading screw system. Acta Neurochir (Wien). 1996;138:146-153.
73 Jenkins JD, Coric D, Branch CLJr. A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366-370.
74 Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9:56-59.
75 Geisler FH, Cheng C, Poka A, et al. Anterior screw fixation of posteriorly displaced type II odontoid fractures. Neurosurgery. 1989;25:30-38.
76 Magerl F, Seemann P-S. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical Spine I. New York: Springer; 1986:322-327.
77 Grob D, Magerl F. [Surgical stabilization of C1 and C2 fractures.]. Orthopade. 1987;16:46-54.
78 Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464-475.
79 Grob D, Jeanneret B, Aebi M, et al. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br. 1991;73:972-976.
80 Grob D, Crisco JJ, Panjabi MM, et al. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine. 1992;17:480-490.
81 Apfelbaum RI. Posterior C1-2 screw fixation for atlantoaxial instability. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas, Vol. 4. Park Ridge, IL: AANS Publication Committee; 1995:19-28.
82 Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation: technical description and report of 22 cases. Neurosurgery. 1993;32:948-954. discussion 954-955
83 Rocha R, Safavi-Abbasi S, Reis C, et al. Working area, safety zones, and angles of approach for posterior C-1 lateral mass screw placement: a quantitative anatomical and morphometric evaluation. J Neurosurg Spine. 2007;6:247-254.
84 Chapman J, Bransford R. Geriatric spine fractures: an emerging healthcare crisis. J Trauma. 2007;62(6 suppl):S61-S62.
85 Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures with special reference to the elderly patient. Clin Orthop Relat Res. 1985;193:178-183.
86 Müller EJ, Wick M, Russe O, et al. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360-365.
87 Kuntz C4th, Mirza SK, Jarell AD, et al. Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurg Focus. 2000;8(6):e7.
88 Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients; a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord. 1995;8:166-169.
89 Ryan MD, Taylor TK. Odontoid fractures in the elderly. J Spinal Disord. 1993;6:397-401.
90 Tashjian RZ, Majercik S, Biffl WL, et al. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199-203.
91 Haughton S. On hanging, considered from a mechanical and physiological point of view. Philos Mag J Sci. 1866;32:23-34.
92 Haughton S. Judicial hanging. Lancet. 1913;1:629.
93 Duggal N, Chamberlain RH, Perez-Garza LE, et al. Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine. 2007;32:182-187.
94 White AAIII, Panjabi MM. Clinical Biomechanics of the Spine, 2nd ed. Philadelphia: JB Lippincott; 1990.
95 Wood-Jones F. The ideal lesion produced by judicial hanging. Lancet. 1913;1:53.
96 Grogono B. Injuries of the atlas and axis. J Bone Joint Surg Br. 1954;36:397-410.
97 Schneider RC, Livingston KE, Cave AJ, et al. “Hangman’s fracture” of the cervical spine. J Neurosurg. 1965;22:141-154.
98 Fielding JW, Francis WRJr, Hawkins RJ, et al. Traumatic spondylolisthesis of the axis. Clin Orthop Relat Res. 1989;239:47-52.
99 Francis WR, Fielding JW, Hawkins RJ, et al. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br. 1981;63:313-318.
100 Coric D, Wilson JA, Kelly DLJr. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85:550-554.
101 Effendi B, Roy D, Cornish B, et al. Fractures of the ring of the axis: a classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63:319-327.
102 Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217-226.
103 Starr JK, Eismont FJ. Atypical hangman’s fractures. Spine. 1993;18:1954-1957.
104 Li XF, Dai LY, Lu H, et al. A systematic review of the management of hangman’s fractures. Eur Spine J. 2006;15:257-269.
105 Vieweg U, Meyer B, Schramm J. Differential treatment in acute upper cervical spine injuries: a critical review of a single-institution series. Surg Neurol. 2000;54:203-210.
106 Hakalo J, Wronski J. Operative treatment of hangman’s fractures of C2. Posterior direct pars screw repair or anterior plate-cage stabilization? Neurol Neurochir Pol. 2008;42:28-36.
107 Tuite GF, Papadopoulos SM, Sonntag VK. Caspar plate fixation for the treatment of complex hangman’s fractures. Neurosurgery. 1992;30:761-764. discussion 764-765
108 Benzel EC, Hart BL, Ball PA, et al. Fractures of the C2 vertebral body. J Neurosurg. 1994;81:206-212.
109 Fujimura Y, Nishi Y, Kobayashi K. Classification and treatment of axis body fractures. J Orthop Trauma. 1996;10:536-540.