CHAPTER 31 Essex-Lopresti Fractures
Injury Pattern and Biomechanics
When a fall on an outstretched hand leads to a comminuted radial head fracture, longitudinal radioulnar dissociation (LRUD) may result if the forearm interosseous ligament (IOL) tears as well. This is often referred to as the Essex-Lopresti lesion. This injury pattern was initially described by Curr and Coe in 1946,1 but Essex-Lopresti illustrated the importance of diagnosing longitudinal radioulnar instability.2 Fracture of the radial head, disruption of the central third of the IOL, historically referred to as the interosseous membrane,3–7 and injury to the distal radioulnar joint (DRUJ), contribute to loss of forearm stability. In LRUD, lack of forearm stability leads to loss of forearm rotation, decreased wrist extension, ulnar wrist pain, and elbow pain.3–7 Understanding normal forearm biomechanics facilitates treatment of this challenging clinical problem.
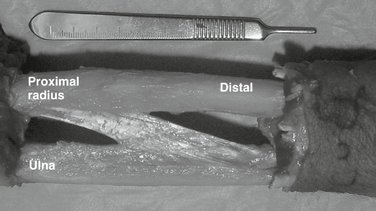
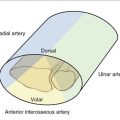
The biomechanics of the forearm axis are best explained in terms of load transfer and stability. With use of the hand, and forceful grip, forces are transferred through the wrist to the elbow via the forearm IOL. Abnormal load transfer may result in pain secondary to abnormally high joint contact stresses at the elbow and ulnocarpal joints. As the forearm is loaded axially in compression, the IOL is loaded in tension. The IOL functions not only to transfer load from the radius to the ulna but also to pull the radius and ulna together at the proximal and distal radioulnar joints (Fig. 31-1).8–12 Numerous studies have shown that the IOL and the triangular fibrocartilage complex (TFCC) help to provide stability to the DRUJ.13–17
Diagnosis
With a high-energy axial load applied to the forearm through the wrist, the radial head can fracture. With enough energy, the IOL and DRUJ can also be disrupted. Injury to the IOL and DRUJ can be easily overlooked if attention is focused on the radial head fracture alone.18 After a few weeks, patients with LRUD can present with ulnar-sided wrist pain, loss of forearm rotation, and elbow pain. Physical examination will show painful rotation and ulnar deviation, forearm swelling, and lateral elbow tenderness.
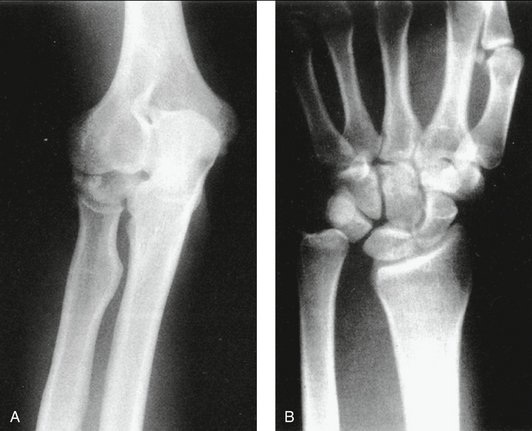
Minimal radial shortening of up to 2 mm may be expected with a simple fracture of the radial head.19,20 However, greater than 2 mm of radial shortening and radial head comminution are strongly suggestive of LRUD (Fig. 31-2).21
Edwards and Jupiter22 proposed a classification system for the Essex-Lopresti type radial head fractures:
Patients presenting with a comminuted radial head may present acutely with symptomatic LRUD, but they also have the potential to develop late LRUD. Although patients with LRUD may present acutely with wrist pain and forearm swelling, this is typically not the case. Forearm and wrist films should be obtained along with elbow films. Magnetic resonance imaging and ultrasonography have also proved useful in imaging IOL tears.23–27 Radius stability can be assessed intraoperatively by applying axial load to the radius (“shuck” test). Proximal migration of the radius in late LRUD may be frank or occult. In frank cases, LRUD is seen on plain radiographs. In occult cases, power grip and axial stress views may elicit ulnar-positive variance.28,29 Proximal migration of the radius may be fixed or reducible; distinguishing this can help guide treatment. If frank, dynamic fluoroscopic evaluation utilizing finger traps can illustrate if the deformity is reducible, then ulnar-positive variance may be “reduced” to ulnar-neutral variance. In the occult case, ulnar-positive variance is, by definition, dynamic.
Current Treatment and Surgical Technique
When the IOL is torn, the radial head is essential for maintaining longitudinal stability. If ORIF is not possible, radial head arthroplasty functions to share the load at the elbow and prevent proximal migration of the radius. Although Silastic radial heads have been used in the past, nonmetallic implants have been shown to collapse over time and may cause synovitis.16,30–33 Metallic prostheses are stiffer than Silastic ones and are more effective in preventing proximal migration of the radius.34–37 However, long-term clinical results of metallic radial heads in cases of LRUD are still lacking in the literature. There may be complications due to implant loosening and dislocation and elbow stiffness and capitellar wear from oversizing the implant.
Modular radial heads offer a more anatomical design. Grewal and associates recently reported favorable short-term clinical results at 2 years with modular radial head replacement for comminuted radial head fractures.37 Even though this study lacked a control group, the authors found no evidence of overstuffing and 81% did not have arthritic changes. However, the outcomes of modular radial heads in patients with Essex-Lopresti fracture-dislocations in particular remain to be seen.
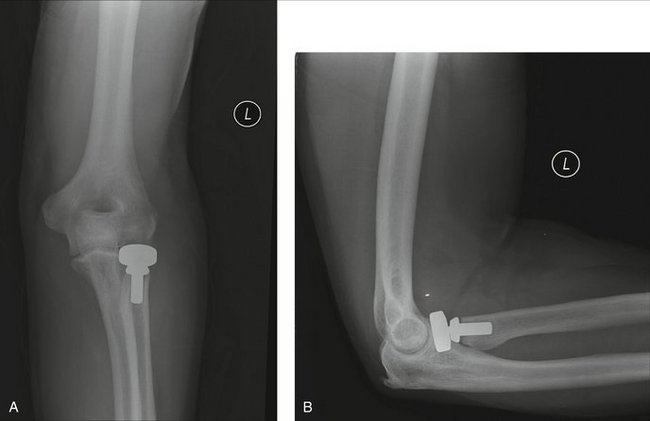
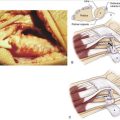
Treatment of Acute LRUD
The overall goal of treatment is to restore load sharing between the radius and ulna and prevent long-term proximal migration of the radius. The structures that require attention include the radial head, the TFCC, and the IOL. The radial head should be preserved if ORIF is possible. However, comminution of the radial head may prevent repair. Therefore, restoring radial length will require metallic radial head arthroplasty (Fig. 31-3). In addition, pinning of the DRUJ for 4 weeks is recommended to allow the TFCC and DRUJ capsule to heal. Furthermore, because failure of this acute treatment strategy has significant consequences, and as the technique of open foveal reattachment of the torn TFCC has been refined, we advise a more aggressive approach to address the wrist after radial head replacement and restoration of the normal radioulnar relationship—open TFCC repair plus DRUJ pinning. This will ensure as precise a restoration of normal anatomy at the wrist as possible.
Contraindications
Silastic radial heads and radial head allografts are contraindicated. Any decision to salvage the radial head fracture must be based on feasibility of repair. Metallic radial head arthroplasty is probably the better option when comminution exists such that rigid fixation and articular reconstruction are not possible.
Treatment of Late LRUD
When LRUD is unrecognized, hence untreated, restoration of radial length may not be possible. Characterizing proximal migration of the radius as fixed or reducible is critical to the decision-making in such “chronic” cases.38 Traction films with finger traps may be helpful. Fundamentally, intraoperative assessment relies on whether the proximal radius can be “pushed distally” when grasped with a towel clamp. In such cases, radial head replacement is recommended. Treatment recommendations for the reducible DRUJ are the same as for the acute case. However, if the radius cannot be pushed distally, and the DRUJ reduced, ulnar shortening osteotomy or use of an Ilizarov fixator (in a staged procedure) should be used to obtain ulnar-neutral variance. As experience with metallic ulnar head replacement increases, ulnar head arthroplasty may have a role when DRUJ arthritis exists. Although ulnar impaction, DRUJ arthritis, or an irreducible DRUJ may have been treated with distal ulna resection in low-demand wrists, this should not be performed in these types of cases. Grip strength will be compromised because of radioulnar impingement, and load transfer between the hand and elbow will be even more compromised. Indeed, understanding that transverse force vectors exist at the wrist and that the forearm unit functions with the IOL to unload the proximal radius mandates that neither the distal ulna nor the radial head is ever simply resected.
Although IOL reconstruction is still considered experimental, late cases of LRUD may represent the most compelling indication for such a strategy—to improve load sharing between the radius and ulna and reduce loads on the radial head implant.39,40
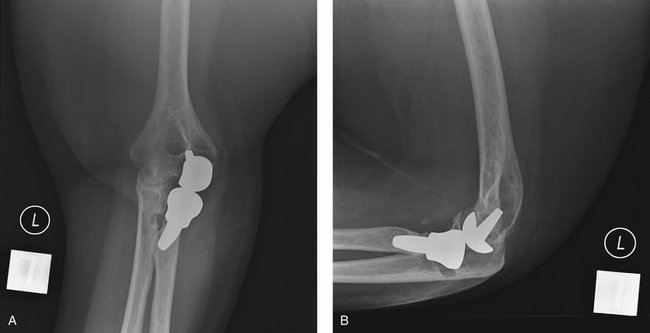
If capitellar wear has developed in chronic cases of untreated LRUD, capitellar resurfacing may be an option at the same time that radial head replacement is performed. Little data exist to support this innovative strategy, but uniarthroplasty (Small Bone Innovations, Inc., New York, NY) may hold promise in the future for such cases (Fig. 31-4).
IOL Reconstruction
In evaluating treatment of the Essex-Lopresti fracture-dislocation, a strategy that includes IOL reconstruction as well as radial head replacement and TFCC repair may be most attractive because historical options described earlier have provided inconsistent and, too frequently, inadequate results.3,6,39–46 Because IOL reconstruction is still considered experimental, it is not typically recommended. However, reconstruction of the IOL is feasible and likely efficacious based on anatomical and biomechanical studies.
The goal of IOL reconstruction is to restore anatomical load transfer without limiting forearm rotation. Chandler and associates and Forster and coworkers have suggested that tendon graft be placed at an angle of 20 to 24 degrees to the long axis of the ulna.47,48 Chandler and associates also found that the IOL inserts on the radius at a point 57% proximal to the distal radius and 34% proximal to the distal ulna.48 These findings correlate well with those of Skahen and associates49 and Fujita.50 Despite agreement regarding where the IOL footprint is, however, there remains debate on the graft type, placement, and reconstruction technique. Grafts such as hamstring tendons or patellar tendon have similar material properties to the IOL.46,51,52 However, these grafts pose issues with donor site morbidity.53–57 Graft stiffness of the palmaris longus and single-bundle flexor carpi radialis have been shown to be significantly different from the intact IOL.43,52 There is some clinical and basic science experience with the patellar tendon graft using a dorsal onlay technique described by Ruch and associates.46 However, this reconstruction is nonanatomical and graft length may dictate graft placement.43–46 Long-term clinical outcomes remain to be seen with the patellar tendon graft and onlay technique. Other authors have investigated IOL reconstruction techniques in the laboratory by placing the graft in line with the axis of rotation, but, again, this is nonanatomical and remains a cadaveric experiment.58,59
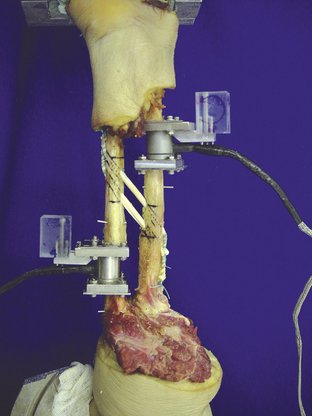
In our laboratory we have investigated IOL reconstruction using a flexor carpi radialis graft placed anatomically in the footprint of the IOL on the radius and ulna. We found that an anatomical single-bundle graft restored approximately 76% of the load transferred through the intact IOL. We also found that an anatomical double-bundle graft was able to restore normal forearm load transfer to that of the intact IOL.39,40 As favorable experience with tendon allograft for such procedures as elbow MCL and LCL reconstruction has grown, we have found that the potential morbidity of autograft use can be safely eliminated. This allows the selection of a lengthy graft such as the tibialis anterior as an alternative to the flexor carpi radialis autograft. Our proposed technique utilizes an anatomical single-bundle technique; this is expected to restore load transfer to approximately 75% of normal (Fig. 31-5). Tibialis anterior tendon graft can be anchored at the radius and ulna with biotenodesis screws (Arthrex, Naples, FL). As experience develops, a double-bundle reconstruction may become feasible, with the added benefit that biomechanical data suggest restoration of normal load transfer.
Contraindications
Contraindications revolve around how likely pain relief and functional restoration are with this approach as compared with creation of a one-bone forearm. In other words, if concern exists over the amount of distal and proximal radioulnar degeneration and if little forearm rotation exists, salvage alone may be advisable.
Results
We have no results to report at this time because our recommendations for surgical technique are based solely on biomechanical and anatomical studies. However, Osterman and associates45 treated 16 patients for chronic LRUD injuries with ulnar-shortening osteotomy and bone-ligament-bone reconstruction using a patellar tendon graft. The initial diagnoses were radial head fracture, radial head fracture with posterior dislocation, Monteggia fracture, radial head fracture with distal radius fracture, and Essex-Lopresti fracture. Interosseous ligament instability was identified an average of 10 months after radial head excision (range: 2 months to 12 years), with 75% of patients presenting within 2 years. The average ulnar variance was 3 mm (range: 2 to 5 mm) on standard posteroanterior radiographs. Other pathological processes included lunate impaction (4 patients), DRUJ arthritis (2 patients), and mild elbow arthritis (5 patients).
1. Curr JF, Coe WA. Dislocation of the inferior radio-ulnar joint. Br J Surg.. 1946;34:74.
2. Essex-Lopresti P. Fractures of the radial head with distal radio-ulna dislocation. J Bone Joint Surg Br.. 1951;33:244-247.
3. Hotchkiss RN. Fractures of the radial head and related instability and contracture of the forearm. Instr Course Lect.. 1998;47:173-177.
4. Hotchkiss RN. Injuries to the interosseous ligament of the forearm. Hand Clin.. 1994;10:391-398.
5. Mikic ZD, Vukadinovic SM. Late results in fractures of the radial head treated by excision. Clin Orthop Relat Res.. 1983:220-228.
6. Skahen JR. Reconstruction of the interosseous membrane of the forearm in cadavers. Palmer AK, Werner FW, Fortino MD, editors. J Hand Surg [Am].; 1997; 986-994.
7. Sowa DT, Hotchkiss RN, Weiland AJ. Symptomatic proximal translation of the radius following radial head resection. Clin Orthop Relat Res.. 1995:106-113.
8. Halls AA, Travill A. Transmission of pressures across the elbow joint. Anat Rec.. 1960;150:243-248.
9. Pfaeffle HJ, Fischer KJ, Manson TT, et al. Role of the forearm interosseous ligament: is it more than just longitudinal load transfer. J Hand Surg [Am].. 2000;25:683-688.
10. Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg [Am].. 1984;9:681-682.
11. Markolf KL, Lamey D, Yang S, et al. Radioulnar load-sharing in the forearm: a study in cadavera. J Bone Joint Surg Am.. 1998;80:879-888.
12. Birkbeck DP, Failla JM, Hoshaw SJ, et al. The interosseous membrane affects load distribution in the forearm. J Hand Surg [Am].. 1997;22:975-980.
13. Kleinman WB, Graham TJ. The distal radioulnar joint capsule: clinical anatomy and role in posttraumatic limitation of forearm rotation. J Hand Surg [Am].. 1998;23:588-599.
14. Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg [Am].. 2000;25:689-699.
15. Ward LD, Ambrose CG, Masson MV, Levaro F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg [Am].. 2000;25:341-351.
16. Hotchkiss RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg [Am].. 1989;14:256-261.
17. Rabinowitz RS, Light TR, Havey RM, et al. The role of the interosseous membrane and triangular fibrocartilage complex in forearm stability. J Hand Surg [Am].. 1994;19:385-393.
18. Jungbluth P, Frangen TM, Arens S, et al. The undiagnosed Essex-Lopresti injury. J Bone Joint Surg Br.. 2006;88:1629-1633.
19. Morrey BF, Chao EY, Hui FC. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am.. 1979;61:368.
20. Stephen IB. Excision of the radial head for closed fracture. Acta Orthop Scand.. 1981;52:409-412.
21. Davidson PA, Moseley JBJr, Tullos HS. Radial head fracture: a potentially complex injury. Clin Orthop Relat Res.. 1993:224-230.
22. Edwards GSJr, Jupiter JB. Radial head fractures with acute distal radioulnar dislocation. Essex-Lopresti revisited. Clin Orthop Relat Res.. 1988:61-69.
23. Failla JM, Jacobson J, van Holsbeeck M. Ultrasound diagnosis and surgical pathology of the torn interosseous membrane in forearm fractures/dislocations. J Hand Surg [Am].. 1999;24:257-266.
24. Nakamura T, Yabe Y, Horiuchi Y. In vivo MR studies of dynamic changes in the interosseous membrane of the forearm during rotation. J Hand Surg [Br].. 1999;24:245-248.
25. Starch DW, Dabezies EJ. Magnetic resonance imaging of the interosseous membrane of the forearm. J Bone Joint Surg Am.. 2001;83:235-238.
26. Wallace AL, Walsh WR, van Rooijen M, et al. The interosseous membrane in radio-ulnar dissociation. J Bone Joint Surg Br.. 1997;79:422-427.
27. Soubeyrand M, Lafont C, Oberlin C, et al. The “muscular hernia sign”: an original ultrasonographic sign to detect lesions of the forearm’s interosseous membrane. Surg Radiol Anat.. 2006;28:372-378.
28. Tomaino MM. The importance of the pronated grip x-ray view in evaluating ulnar variance. J Hand Surg [Am].. 2000;25:352-357.
29. Shen J, Papadonikolakis A, Garrett JP, et al. Ulnar-positive variance as a predictor of distal radioulnar joint ligament disruption. J Hand Surg [Am].. 2005;30:1172-1177.
30. Gordon M, Bullough PG. Synovial and osseous inflammation in failed silicone-rubber prostheses. J Bone Joint Surg Am.. 1982;64:574-580.
31. Morrey BF, Askew L, Chao EY. Silastic prosthetic replacement for the radial head. J Bone Joint Surg Am.. 1981;63:454-458.
32. Vanderwilde RS, Morrey BF, Melberg MW, Vinh TN. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg [Br].. 1994;76:78-81.
33. Worsing RAJr, Engber WD, Lange TA. Reactive synovitis from particulate silastic. J Bone Joint Surg Am.. 1982;64:581-585.
34. Judet T, Massin P, Bayeh PJ. Radial head prosthesis with floating cup in recent and old injuries of the elbow: preliminary results. Rev Chir Orthop Rep Appareil Moteur. 1994;80:123-130.
35. Knight DJ, Rymaszewski LA, Amis AA, Miller JH. Primary replacement of the fractured radial head with a metal prosthesis. J Bone Joint Surg Br.. 1993;75:572-576.
36. Popovic N, Gillet P, Rodriguez A, Lemaire R. Fracture of the radial head with associated elbow dislocation: results of treatment using a floating radial head prosthesis. J Orthop Trauma.. 2000;14:171-177.
37. Grewal R, MacDermid JC, Faber KJ, et al. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty: study of outcomes. J Bone Joint Surg Am.. 2006;88:2192-2200.
38. Smith AM, Urbanosky LR, Castle JA, et al. Radius pull test: predictor of longitudinal forearm instability. J Bone Joint Surg Am.. 2002;84:1970-1976.
39. Pfaeffle HJ, Stabile KJ, Li ZM, Tomaino MM. Reconstruction of the interosseous ligament unloads metallic radial head arthroplasty and the distal ulna in cadavers. J Hand Surg [Am].. 2006;31:269-278.
40. Pfaeffle HJ, Stabile KJ, Li ZM, Tomaino MM. Reconstruction of the interosseous ligament restores normal forearm compressive load transfer in cadavers. J Hand Surg [Am].. 2005;30:319-325.
41. Harrington IJ, Sekyi-Otu A, Barrington TW, et al. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma.. 2001;50:46-52.
42. Sellman DC, Seitz WHJr, Postak PD, Greenwald AS. Reconstructive strategies for radioulnar dissociation: a biomechanical study. J Orthop Trauma.. 1995;9:516-522.
43. Tejwani SG, Markolf KL, Benhaim P. Graft reconstruction of the interosseous membrane in conjunction with metallic radial head replacement: a cadaveric study. J Hand Surg [Am].. 2005;30:335-342.
44. Tejwani SG, Markolf KL, Benhaim P. Reconstruction of the interosseous membrane of the forearm with a graft substitute: a cadaveric study. J Hand Surg [Am].. 2005;30:326-334.
45. Osterman AL, Culp RW, Warhold LG: Reconstruction of the interosseous membrane using a bone-ligament-bone graft. Presented before the American Academy of Orthopaedic Surgeons, 2000.
46. Ruch DS, Change DS, Koman LA. Reconstruction of longitudinal stability of the forearm after disruption of interosseous ligament and radial head excision (Essex-Lopresti lesion). J South Orthop Assoc.. 1999;8:47-52.
47. Forster RI, Sharkey NA, Szabo RM. Forearm interosseous ligament isometry. J Hand Surg [Am].. 1999;24:538-545.
48. Chandler JW, Stabile KJ, Pfaeffle HJ, et al. Anatomic parameters for planning of interosseous ligament reconstruction using computer-assisted techniques. J Hand Surg [Am].. 2003;28:111-116.
49. Skahen JR. The interosseous membrane of the forearm: anatomy and function. Palmer AK, Werner FW, Fortino MD, editors. J Hand Surg [Am].; 1997; 981-985.
50. Fujita M. An anatomical study on the interosseous membrane of the forearm. Nippon Sei Gakkai Zasshi. 1995;69:938-950.
51. Pfaeffle HJ, Tomaino MM, Grewal R, et al. Tensile properties of the interosseous membrane of the human forearm. J Orthop Res.. 1996;14:842-845.
52. Stabile KJ, Pfaeffle J, Saris I, et al. Structural properties of reconstruction constructs for the interosseous ligament of the forearm. J Hand Surg [Am].. 2005;30:312-318.
53. Matsumoto A, Yoshiya S, Muratsu H, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med.. 2006;34:213-219.
54. Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy.. 2001;17:971-980.
55. Miller MD, Nichols T, Butler CA. Patella fracture and proximal patellar tendon rupture following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy.. 1999;15:640-643.
56. Kohn D, Sander-Beuermann A. Donor-site morbidity after harvest of a bone-tendon-bone patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc.. 1994;2:219-223.
57. Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med.. 1989;17:760-765.
58. Soubeyrand M, Oberlin C, Dumontier C, et al. Ligamentoplasty of the forearm interosseous membrane using the semitendinosus tendon: anatomical study and surgical procedure. Surg Radiol Anat.. 2006;28:300-307.
59. Marcotte A, Osterman AL. Longitudinal radioulnar dissociation: identification and treatment of acute and chronic injuries. Hand Clin.. 2007;23:195-208.
60. Brockman E. Two cases of disability at the wrist joint following excision of the radial head. Proc R Soc Med.. 1930;21(5):904-905.
61. Graham TJ, Fischer TJ, Hotchkiss RN, Kleinman WB. Disorders of the forearm axis. Hand Clin.. 1998;14:305-316.