1. Simeón-Aznar, CP, et al. Systemic sclerosis sine scleroderma and limited cutaneous systemic sclerosis: similarities and differences. Clin Exp Rheumatol. 2014. [ePub].
2. Savarino, E, et al. Gastroesophageal reflux and pulmonary fibrosis in scleroderma: a study using pH-impedance monitoring. Am J Respir Crit Care Med. 2009; 179(5):408–413.
3. Hinchcliff, M, et al. Systemic sclerosis/scleroderma: a treatable multisystem disease. Am Fam Physician. 2008; 78(8):961–968.
4. Vonk, MC, et al. Oesophageal dilatation on high-resolution computed tomography scan of the lungs as a sign of scleroderma. Ann Rheum Dis. 2008; 67(9):1317–1321.
5. Sifrim, D, et al. Non-achalasic motor disorders of the oesophagus. Best Pract Res Clin Gastroenterol. 2007; 21(4):575–593.
6. Ntoumazios, SK, et al. Esophageal involvement in scleroderma: gastroesophageal reflux, the common problem. Semin Arthritis Rheum. 2006; 36(3):173–181.
7. Mayes, MD. Scleroderma epidemiology. Rheum Dis Clin North Am. 2003; 29(2):239–254.
8. Goldblatt, F, et al. Antibody-mediated gastrointestinal dysmotility in scleroderma. Gastroenterology. 2002; 123(4):1144–1150.
9. Coggins, CA, et al. Wide-mouthed sacculations in the esophagus: a radiographic finding in scleroderma. AJR Am J Roentgenol. 2001; 176(4):953–954.
10. Duchini, A, et al. Gastrointestinal hemorrhage in patients with systemic sclerosis and CREST syndrome. Am J Gastroenterol. 1998; 93(9):1453–1456.
11. Weston, S, et al. Clinical and upper gastrointestinal motility features in systemic sclerosis and related disorders. Am J Gastroenterol. 1998; 93(7):1085–1089.
12. Lock, G, et al. Gastrointestinal manifestations of progressive systemic sclerosis. Am J Gastroenterol. 1997; 92(5):763–771.
13. Young, MA, et al. Gastrointestinal manifestations of scleroderma. Rheum Dis Clin North Am. 1996; 22(4):797–823.
14. Kahan, A, et al. Gastrointestinal involvement in systemic sclerosis. Clin Dermatol. 1994; 12(2):259–265.
15. Ott, DJ. Esophageal motility disorders. Semin Roentgenol. 1994; 29(4):321–331.

 with a distal esophageal stricture
with a distal esophageal stricture  . Esophageal peristalsis was completely absent.
. Esophageal peristalsis was completely absent.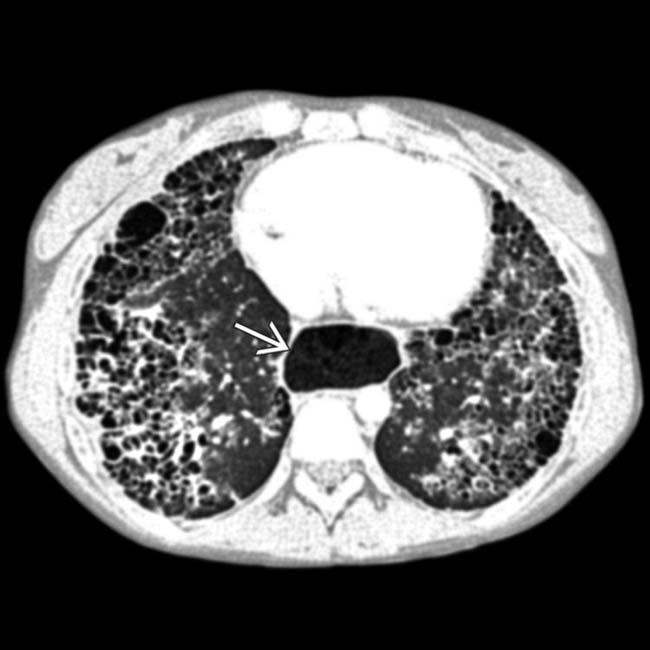
 , all findings due to scleroderma.
, all findings due to scleroderma.
 .
.
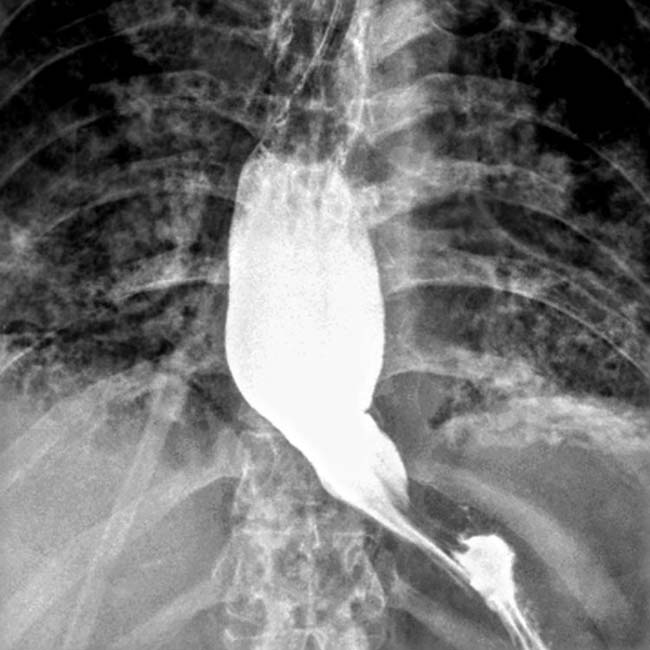
 . The esophageal lumen is mildly dilated, and there is a stricture at the GE junction
. The esophageal lumen is mildly dilated, and there is a stricture at the GE junction  .
.
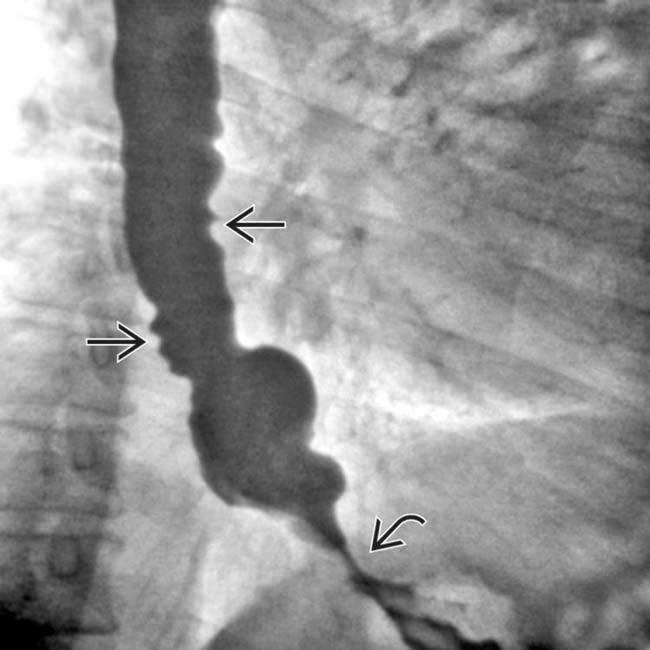
 , and the lumen is dilated with minimal peristalsis in this classic “hidebound” bowel.
, and the lumen is dilated with minimal peristalsis in this classic “hidebound” bowel.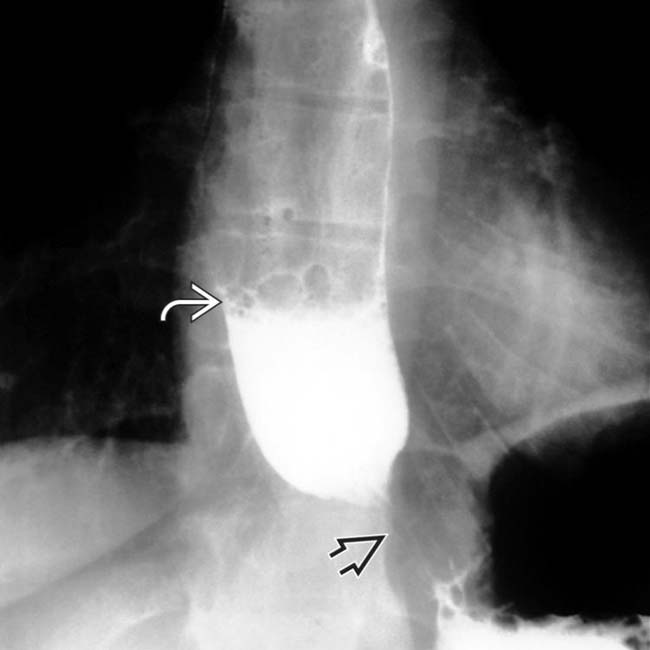
 at the GE junction. The esophagus was slow to empty, even in the upright position, with a fluid-barium level seen
at the GE junction. The esophagus was slow to empty, even in the upright position, with a fluid-barium level seen  .
.
 , with abrupt narrowing as it crosses the spine. The duodenum is the most frequently affected part of the GI tract beyond the esophagus.
, with abrupt narrowing as it crosses the spine. The duodenum is the most frequently affected part of the GI tract beyond the esophagus.
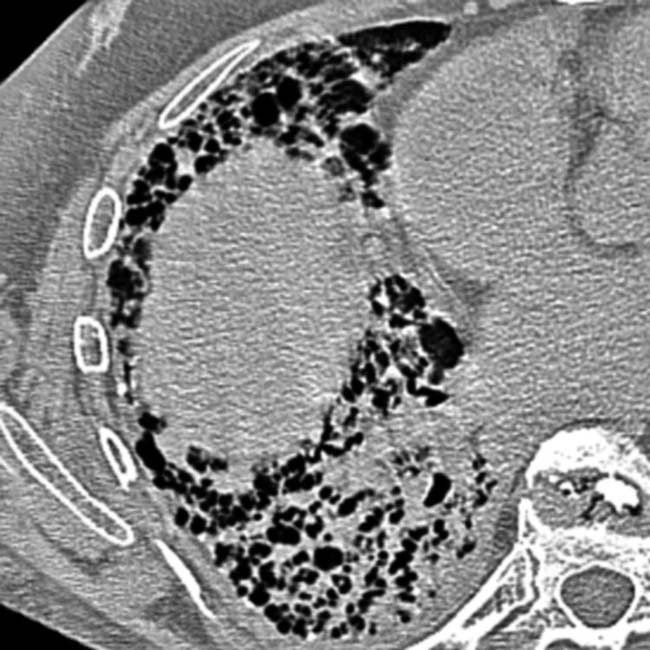
 . The esophagus had no primary peristalsis. These are relatively early signs of scleroderma, and no stricture or ulcerations have yet developed.
. The esophagus had no primary peristalsis. These are relatively early signs of scleroderma, and no stricture or ulcerations have yet developed.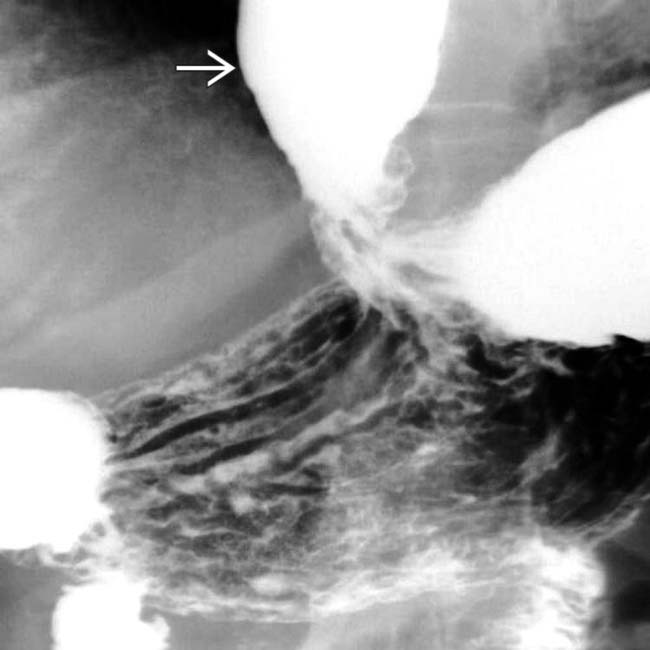
 .
.