Enhancing (hyperemic) peripheral inner rim (increased vascularity)
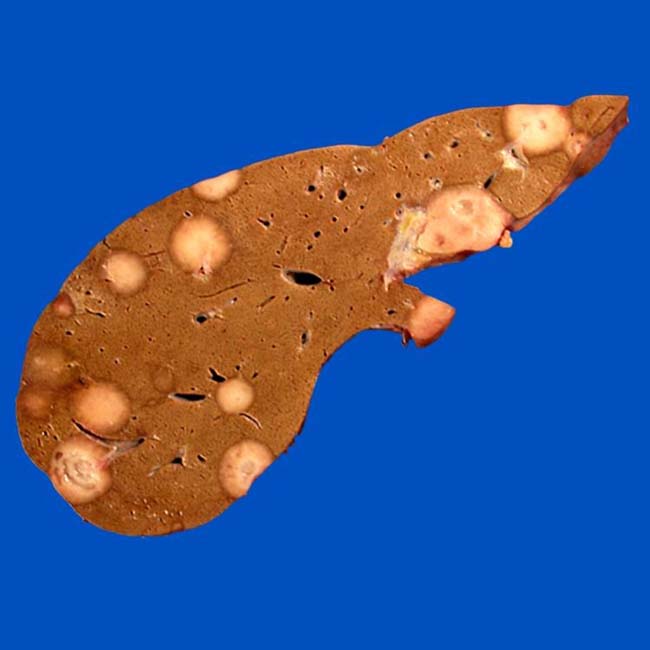
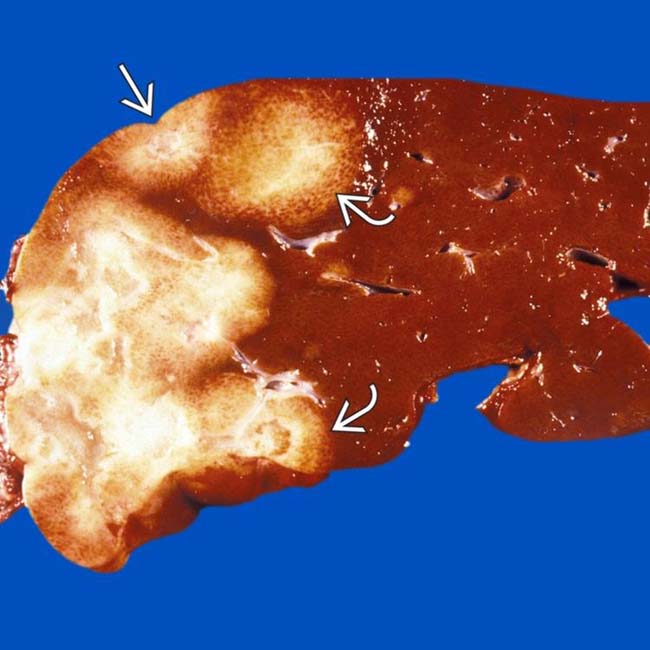
• Spectrum of growth in lesions may be seen: Nodular form (more common); diffuse or extensive form (very rare)

 with a “target” appearance (central lucency), typical CT findings of epithelioid hemangioendothelioma (EHE). The subcapsular lesions are associated with retraction of the overlying liver capsule
with a “target” appearance (central lucency), typical CT findings of epithelioid hemangioendothelioma (EHE). The subcapsular lesions are associated with retraction of the overlying liver capsule  .
.
 typical of EHE, mostly in a peripheral location within the liver.
typical of EHE, mostly in a peripheral location within the liver.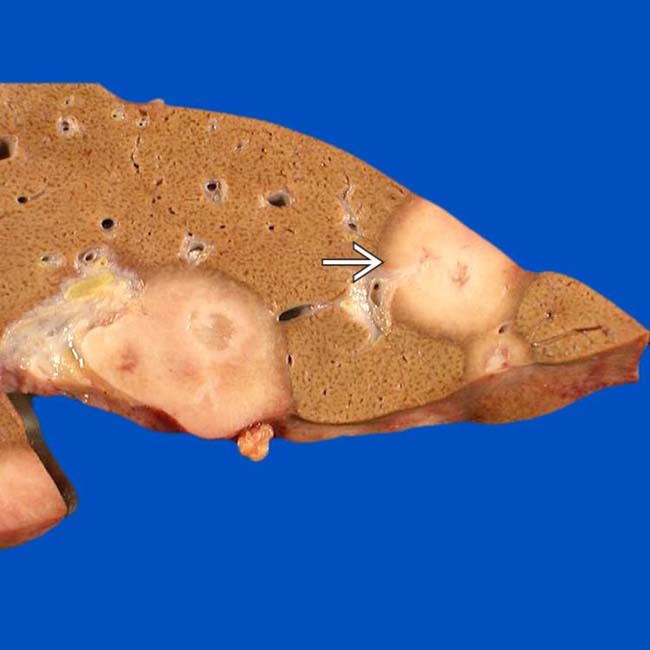
 and hyperemic tumor.
and hyperemic tumor.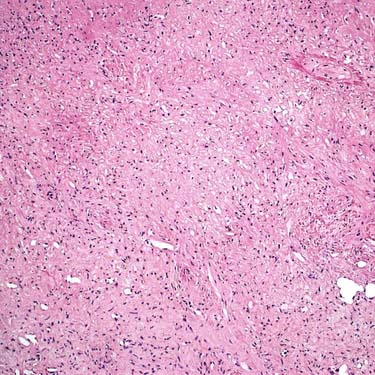

 .
.
 .
.
 . The capsular retraction over 1 of the peripheral masses is also evident
. The capsular retraction over 1 of the peripheral masses is also evident  . The liver itself is not cirrhotic.
. The liver itself is not cirrhotic.
 . Note the hypodense center, inner rim of hypervascular enhancement, and outer rim of avascular hypodensity.
. Note the hypodense center, inner rim of hypervascular enhancement, and outer rim of avascular hypodensity.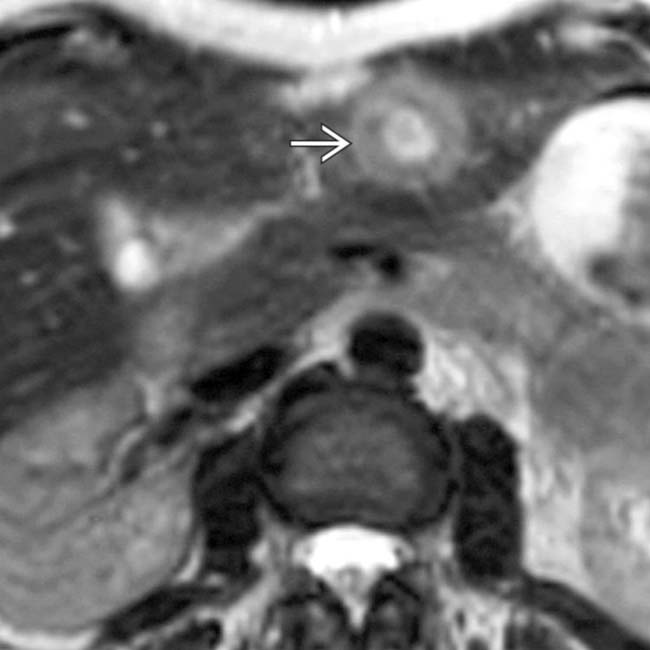
 with central hyperintensity, an inner rim of hypointensity, and an outer rim of hyperintensity.
with central hyperintensity, an inner rim of hypointensity, and an outer rim of hyperintensity.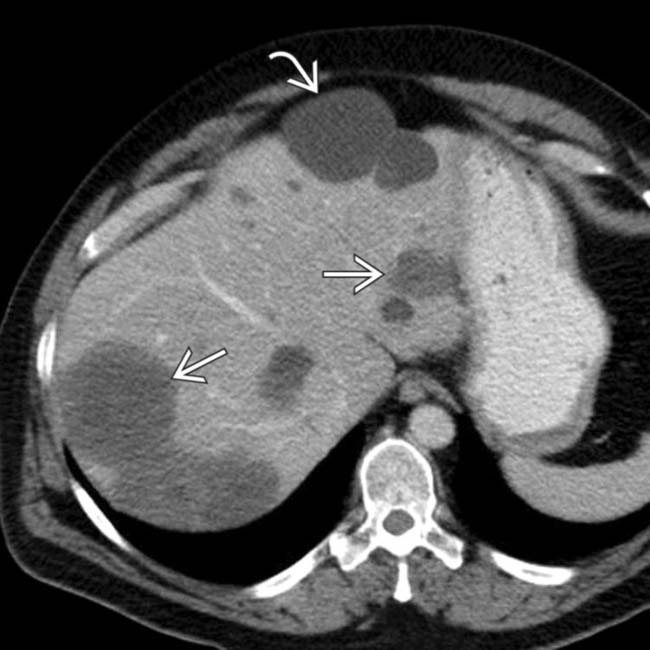
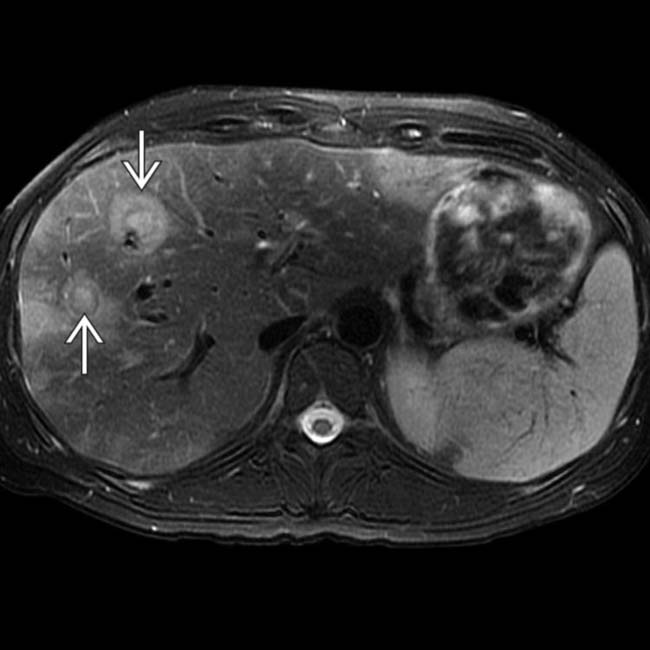
 are of water density and homogeneous; whereas, multiple foci of EHE
are of water density and homogeneous; whereas, multiple foci of EHE  are heterogeneous.
are heterogeneous.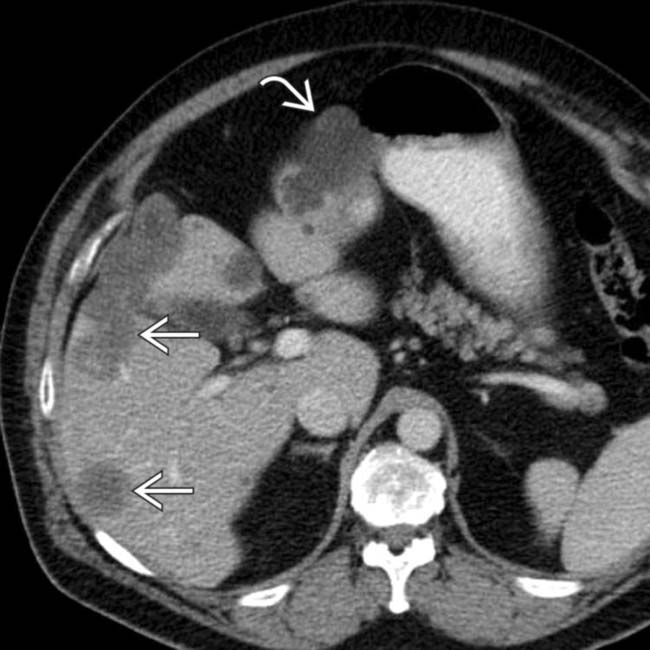
 and foci of EHE
and foci of EHE  , many of which are confluent. Multiplicity, peripheral location, confluence, and capsular retraction are all classic features of EHE.
, many of which are confluent. Multiplicity, peripheral location, confluence, and capsular retraction are all classic features of EHE.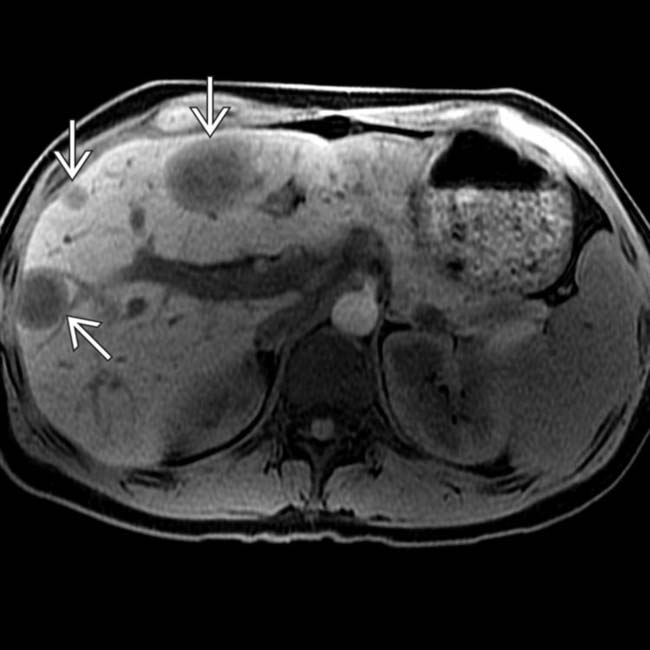
 , with the typical peripheral location and “target” appearance, with the central fibrotic stroma appearing especially hypointense.
, with the typical peripheral location and “target” appearance, with the central fibrotic stroma appearing especially hypointense.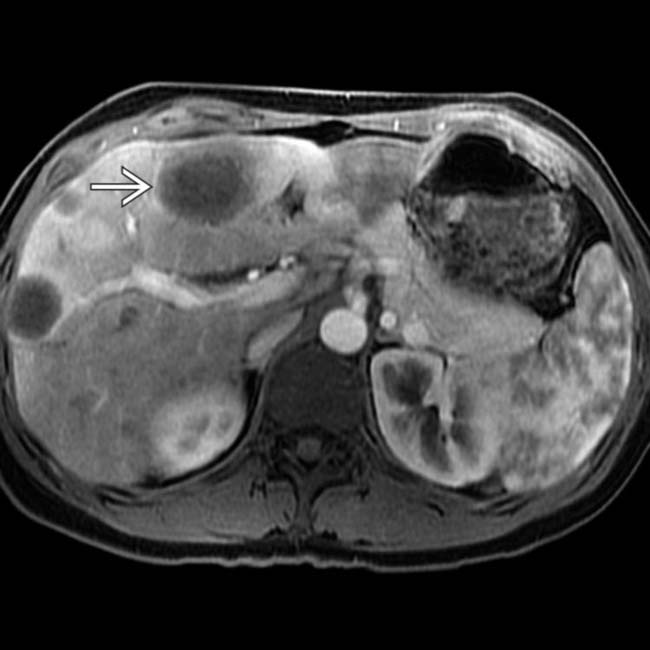
 .
.
 , with the fibrous stroma in the center of the tumors being relatively hyperintense.
, with the fibrous stroma in the center of the tumors being relatively hyperintense.
 . These are typical clinical and imaging features of hepatic EHE.
. These are typical clinical and imaging features of hepatic EHE.
 throughout the periphery of both hepatic lobes. Note the confluent tumor in the lateral segment with marked volume loss
throughout the periphery of both hepatic lobes. Note the confluent tumor in the lateral segment with marked volume loss  .
.
 of some of the tumor foci, consisting of central low density and surrounding layers of relatively high and low density. Note the absence of imaging signs of cirrhosis.
of some of the tumor foci, consisting of central low density and surrounding layers of relatively high and low density. Note the absence of imaging signs of cirrhosis.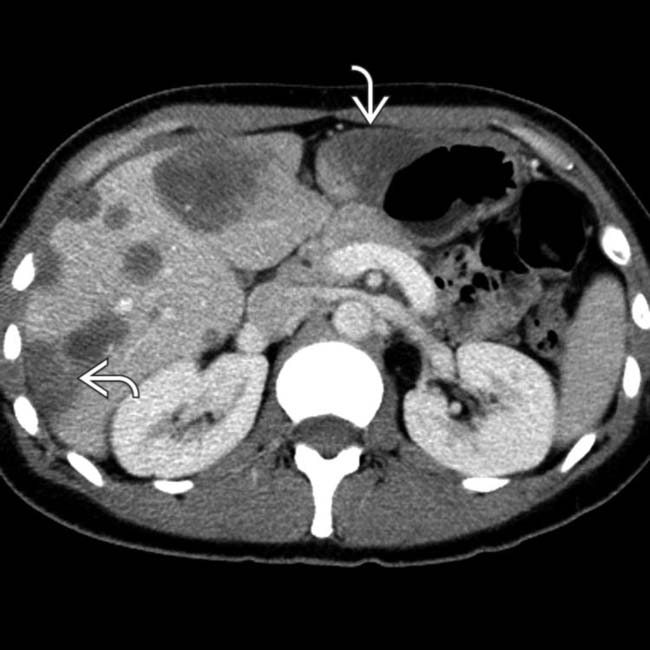
 .
.
 and the hemispheric shape of the subcapsular lesions
and the hemispheric shape of the subcapsular lesions  .
.
 , indicating loss of volume in the affected segments of liver.
, indicating loss of volume in the affected segments of liver.
 .
.