26
Epidermolysis Bullosa
• Inherited EB is traditionally divided into three major categories – EB simplex (EBS), junctional EB (JEB), and dystrophic EB (DEB) – that differ in the ultrastructural site of blister formation (Fig. 26.1).
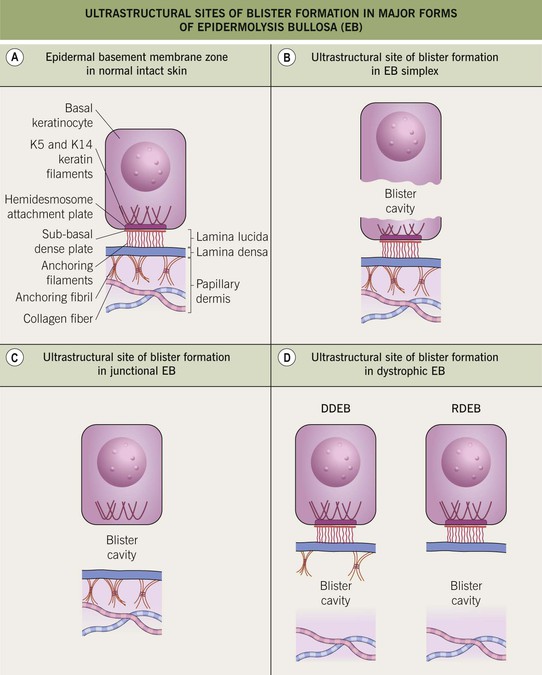
Fig. 26.1 Ultrastructural sites of blister formation in major forms of epidermolysis bullosa (EB). A In intact skin, the ultrastructural regions of the epidermal basement membrane zone consist of (1) basal keratinocytes and the hemidesmosomal plaque; (2) the lamina lucida; (3) the lamina densa; (4) the upper papillary dermis. B In EB simplex (EBS), blisters arise within the lower portion of basal keratinocytes. C In junctional EB (JEB), blisters form within the lamina lucida. D In dystrophic EB (DEB), blisters develop below the lamina densa. Anchoring fibrils are reduced in number in dominant DEB (DDEB) and absent or rudimentary in recessive DEB (RDEB). K5 and K14, keratin 5 and keratin 14, respectively.
• The major subtypes of EB and Kindler syndrome (now classified as a fourth form of EB) are summarized in Table 26.1.
Table 26.1
Epidermolysis bullosa (EB) subtypes.
Former names are in parentheses. Suprabasal forms of EB simplex due to desmosomal defects (e.g. plakophilin deficiency) are also included in the EB spectrum; these rare disorders feature blistering (with acantholysis in skin biopsy specimens), PPK, nail dystrophy, and hypotrichosis.
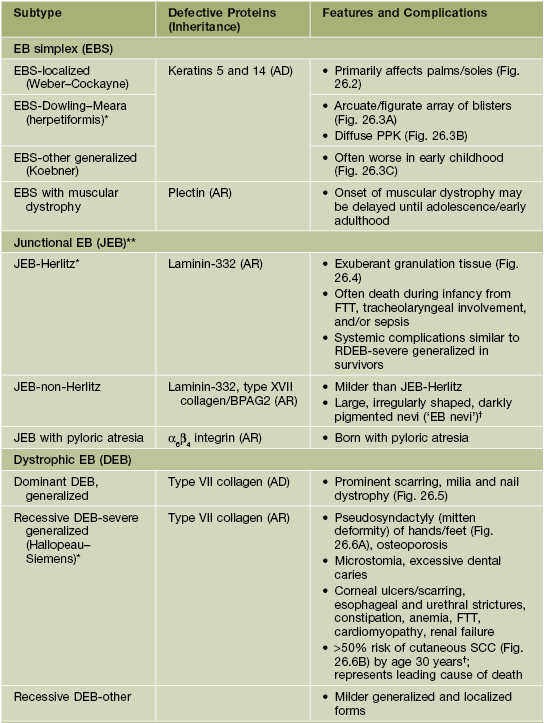
* Most severe subtype in EBS, JEB, and DEB groups, respectively.
** Dental enamel hypoplasia occurs in all forms of JEB.
† ‘EB nevi’ occasionally occur in other EB subtypes, and patients with RDEB–severe generalized have an increased risk of melanoma.
‡ Mediates anchorage between the actin cytoskeleton and the extracellular matrix via focal adhesions.
AD, autosomal dominant; AR, autosomal recessive; BPAG, bullous pemphigoid antigen; FTT, failure to thrive; PPK, palmoplantar keratoderma.


Fig. 26.2 Localized epidermolysis bullosa simplex. A, B Bullae arising on the toes and plantar surfaces at sites of lateral or rotary traction. The majority of blisters occur in acral sites. B, Courtesy, Julie V. Schaffer, MD.



Fig. 26.3 Generalized forms of epidermolysis bullosa simplex (EBS). A Arcuate array of vesicles in a child with EBS, Dowling–Meara. B Diffuse palmar keratoderma in an adult with EBS, Dowling–Meara. C Widespread blistering in a toddler with EBS, other generalized. A, C, Courtesy, Julie V. Schaffer, MD.


Fig. 26.4 Junctional epidermolysis bullosa, Herlitz. A Blisters on the elbow and large areas of denuded skin; note the bright red color in the axilla and groin. B Blisters and large erosions on the abdomen of an infant. B, Courtesy, Julie V. Schaffer, MD.


Fig. 26.5 Dominant dystrophic epidermolysis bullosa. Note the prominent scarring on the chest (A) and hands (B) as well as milia and loss of the fingernails (B) in this teenage boy. Courtesy, Julie V. Schaffer, MD.


Fig. 26.6 Severe generalized recessive dystrophic epidermolysis bullosa. A Partial pseudosyndactyly (mitten deformities) in a child. B Large squamous cell carcinoma in a 21-year-old man. A, Courtesy, Jo-David Fine, MD; B, Courtesy, Julie V. Schaffer, MD.
Clinical Features of EB
• The severity and distribution of blistering vary depending on the EB subtype (see Table 26.1), the patient’s age (e.g. improving over time, especially for EBS), and environmental factors (e.g. sweating, friction).
• Scarring (usually atrophic), milia and nail dystrophy may develop in any subtype of EB, but they are most common in DEB (Fig. 26.8; see Figs. 26.5 and 26.6).
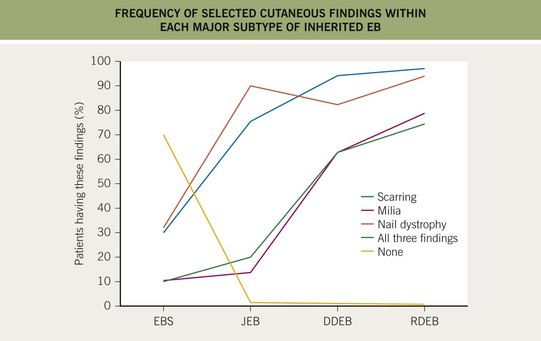
Fig. 26.8 Frequency of selected cutaneous findings within each major subtype of inherited epidermolysis bullosa (EB). Note the increasing frequency from localized EB simplex (EBS) to recessive dystrophic EB (RDEB). JEB, junctional EB; DDEB, dominant dystrophic EB.
• The molecular defects in EB can also affect other organs/tissues with an epithelial surface, such as the oral mucosa (most common), eye, and gastrointestinal and genitourinary tracts (see Table 26.1).
• DDx: sucking blisters and other genetic (e.g. epidermolytic ichthyosis), infectious (e.g. bullous impetigo, staphylococcal scalded skin syndrome) or autoimmune blistering disorders of infancy (see Chapter 28).
Management of EB
• Physicians and families can obtain helpful information from websites such as www.debra.org and www.debra-international.org.
For further information see Ch. 32. From Dermatology, Third Edition.










