Chapter 678 Epidemiology and Prevention of Injuries
Approximately 30 million children and adolescents participate in organized sports in the USA. Approximately 3 million injuries occur annually if injury is defined as time lost from the sport. Deaths in sports are rare, with the majority of nontraumatic deaths caused by cardiac diseases (Chapter 430). Overall, injury rates and injury severity in sports increase with age and pubertal development, related to the greater speed, strength, and intensity of competition.
Preparticipation Sports Examination
The PSE is performed with a directed history and a directed physical examination, including a screening musculoskeletal examination. It identifies possible problems in 1-8% of athletes and excludes <1% from participation. The PSE is not a substitute for the recommended comprehensive annual evaluation, which looks at behaviors that are potentially harmful to teens, such as sexual activity, drug use, and violence, and assesses for depression and suicidal ideation. The purposes of the PSE include detecting medical conditions that delay or disqualify athletic participation owing to a risk of injury or death, detecting previously undiagnosed medical conditions, detecting medical conditions that need further evaluation or rehabilitation before participation, providing guidance for sports participation for patients with health conditions, and meeting legal and insurance obligations. If possible, the PSE should be combined with the comprehensive annual health visit with emphasis on preventive health care (Chapters 5 and 14).
History and Physical Examination
The essential components of the PSE are the history and focused medical and musculoskeletal screening examinations. Identified problems require more investigation (Tables 678-1 and 678-2). In the absence of symptoms, no screening laboratory tests are required.
| COMPONENT OF THE PHYSICAL EXAMINATION | CONDITION TO BE DETECTED |
|---|---|
| Vital signs | Hypertension, cardiac disease, brady- or tachycardia |
| Height and weight | Obesity, eating disorders |
| Vision and pupil size | Legal blindness, absent eye, anisocoria, amblyopia |
| Lymph node | Infectious diseases, malignancy |
| Cardiac (performed standing and supine) | Heart murmur, prior surgery, dysrhythmia |
| Pulmonary | Recurrent and exercise-induced bronchospasm, chronic lung disease |
| Abdomen | Organomegaly, abdominal mass |
| Skin | Contagious diseases (impetigo, herpes, staphylococcal, streptococcal) |
| Genitourinary | Varicocele, undescended testes, tumor, hernia |
| Musculoskeletal | Acute and chronic injuries, physical anomalies (scoliosis) |
Table 678-2 MEDICAL CONDITIONS AND SPORTS PARTICIPATION
| CONDITION | MAY PARTICIPATE | EXPLANATION |
|---|---|---|
| Atlantoaxial instability (instability of the joint between cervical vertebrae 1 and 2) | Qualified yes | Athlete (particularly if he or she has Down syndrome or juvenile rheumatoid arthritis with cervical involvement) needs evaluation to assess the risk of spinal cord injury during sports participation, especially when using a trampoline |
| Bleeding disorder | Qualified yes | Athlete needs evaluation |
| Diabetes mellitus | Yes | All sports can be played with proper attention and appropriate adjustments to diet (particularly carbohydrate intake), blood glucose concentrations, hydration, and insulin therapy Blood glucose concentrations should be monitored before exercise, every 30 min during continuous exercise, 15 min after completion of exercise, and at bedtime |
| Eating disorders | Qualified yes | Athlete with an eating disorder needs medical and psychiatric assessment before participation |
| Fever | No | Elevated core temperature can indicate a pathologic medical condition (infection or disease) that is often manifest by increased resting metabolism and heart rate. Accordingly, during the athlete’s usual exercise regimen, fever can result in greater heat storage, decreased heat tolerance, increased risk of heat illness, increased cardiopulmonary effort, reduced maximal exercise capacity, and increased risk of hypotension because of altered vascular tone and dehydration. On rare occasions, fever accompanies myocarditis or other conditions that can make usual exercise dangerous |
| Heat illness, history of | Qualified yes | Because of the likelihood of recurrence, the athlete needs individual assessment to determine the presence of predisposing conditions and behavior and to develop a prevention strategy that includes sufficient acclimatization (to the environment and to exercise intensity and duration), conditioning, hydration, and salt intake, as well as other effective measures to improve heat tolerance and to reduce heat injury risk (e.g., protective equipment and uniform configurations) |
| HIV infection | Yes | Because of the apparent minimal risk to others, all sports may be played as athlete’s state of health allows (especially if viral load is undetectable or very low) For all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood Certain sports (such as wrestling and boxing) can create a situation that favors viral transmission (likely bleeding plus skin breaks); if viral load is detectable, then athletes should be advised to avoid such high-contact sports |
| Malignant neoplasm | Qualified yes | Athlete needs individual assessment |
| Musculoskeletal disorders | Qualified yes | Athlete needs individual assessment |
| Myopathies | Qualified yes | Athlete needs individual assessment |
| Obesity | Yes | Because of the increased risk of heat illness and cardiovascular strain, obese athletes particularly need careful acclimatization (to the environment and to exercise intensity and duration), sufficient hydration, and potential activity and recovery modifications during competition and training. |
| Organ transplant recipient (and those taking immunosuppressive medications) | Qualified yes | Athlete needs individual assessment for contact, collision, and limited-contact sports In addition to potential risk of infections, some medications (e.g., prednisone) increase tendency for bruising |
| Skin infections, including herpes simplex, molluscum contagiosum, verrucae (warts), staphylococcal and streptococcal infections (furuncles [boils], carbuncles, impetigo, methicillin-resistant Staphylococcus aureus [cellulitis and/or abscesses]), scabies, and tinea | Qualified yes | During contagious periods, participation in gymnastics or cheerleading with mats, martial arts, wrestling, or other collision, contact, or limited-contact sports is not allowed |
| Spleen, enlarged | Qualified yes | If the spleen is acutely enlarged, then participation should be avoided because of risk of rupture If the spleen is chronically enlarged, then individual assessment is needed before collision, contact, or limited-contact sports are played |
| CARDIOVASCULAR | ||
| Carditis (inflammation of the heart) | No | Carditis can result in sudden death with exertion |
| Hypertension (high blood pressure) | Qualified yes | Those with hypertension >5 mm Hg above the 99th percentile for age, sex, and height should avoid heavy weightlifting and power lifting, bodybuilding, and high-static component sports Those with sustained hypertension (>95th percentile for age, sex, and height) need evaluation The National High Blood Pressure Education Program Working Group report defined prehypertension and stage 1 and stage 2 hypertension in children and adolescents <18 yr of age |
| Congenital heart disease (structural heart defects present at birth) | Qualified yes | Consultation with a cardiologist is recommended Those who have mild forms may participate fully in most cases; those who have moderate or severe forms or who have undergone surgery need evaluation The 36th Bethesda Conference defined mild, moderate, and severe disease for common cardiac lesions |
| Heart murmur | Qualified yes | If the murmur is innocent (does not indicate heart disease), full participation is permitted; otherwise, athlete needs evaluation (see structural heart disease, especially hypertrophic cardiomyopathy and mitral valve prolapse) |
| Dysrhythmia (Irregular Heart Rhythm) | ||
| Long-QT syndrome | Qualified yes | Consultation with a cardiologist is advised. Those with symptoms (chest pain, syncope, near-syncope, dizziness, shortness of breath, or other symptoms of possible dysrhythmia) or evidence of mitral regurgitation on physical examination need evaluation; all others may participate fully |
| Malignant ventricular arrhythmias | Qualified yes | |
| Symptomatic Wolff-Parkinson-White syndrome | Qualified yes | |
| Advanced heart block | Qualified yes | |
| Family history of sudden death or previous sudden cardiac event | Qualified yes | |
| Implantation of a cardioverter-defibrillator | Qualified yes | |
| Structural or Acquired Heart Disease | ||
| Hypertrophic cardiomyopathy | Qualified no | Consultation with a cardiologist is recommended. The 36th Bethesda Conference provided detailed recommendations. Most of these conditions carry a significant risk of sudden cardiac death associated with intense physical exercise. Hypertrophic cardiomyopathy requires thorough and repeated evaluations, because disease can change manifestations during later adolescence. Marfan syndrome with an aortic aneurysm also can cause sudden death during intense physical exercise. An athlete who has ever received chemotherapy with anthracyclines may be at increased risk for cardiac problems owing to the cardiotoxic effects of the medications, and resistance training in this population should be approached with caution; strength training that avoids isometric contractions may be permitted. Athlete needs evaluation |
| Coronary artery anomalies | Qualified no | |
| Arrhythmogenic right ventricular cardiomyopathy | Qualified no | |
| Acute rheumatic fever with carditis | Qualified no | |
| Ehlers-Danlos syndrome, vascular form | Qualified no | |
| Marfan syndrome | Qualified yes | |
| Mitral valve prolapse | Qualified yes | |
| Anthracycline use | Qualified yes | |
| Vasculitis, vascular disease | Qualified yes | |
| Kawasaki disease (coronary artery vasculitis) | Qualified yes | Consultation with a cardiologist is recommended. Athlete needs individual evaluation to assess risk on the basis of disease activity, pathologic changes, and medical regimen |
| Pulmonary hypertension | Qualified yes | |
| EYES | ||
| Functionally 1-eyed athlete | Qualified yes | A functionally 1-eyed athlete is defined as having best-corrected visual acuity worse than 20/40 in the poorer-seeing eye. Such an athlete would suffer significant disability if the better eye were seriously injured, as would an athlete with loss of an eye. Specifically, boxing and full-contact martial arts are not recommended for functionally 1-eyed athletes, because eye protection is impractical and/or not permitted. Some athletes who previously underwent intraocular eye surgery or had a serious eye injury may have increased risk of injury because of weakened eye tissue. Availability of eye guards approved by the American Society for Testing and Materials and other protective equipment might allow participation in most sports, but this must be judged on an individual basis |
| Loss of an eye | Qualified yes | |
| Detached retina or family history of retinal detachment at young age | Qualified yes | |
| High myopia | Qualified yes | |
| Connective tissue disorder, such as Marfan or Stickler syndrome | Qualified yes | |
| Previous intraocular eye surgery or serious eye injury | Qualified yes | |
| Conjunctivitis, infectious | Qualified no | Athlete with active infectious conjunctivitis should be excluded from swimming |
| GASTROINTESTINAL | ||
| Malabsorption syndromes (celiac disease or cystic fibrosis) | Qualified yes | Athlete needs individual assessment for general malnutrition or specific deficits resulting in coagulation or other defects; with appropriate treatment, these deficits can be treated adequately to permit normal activities |
| Short-bowel syndrome or other disorders requiring specialized nutritional support, including parenteral or enteral nutrition | Qualified yes | Athlete needs individual assessment for collision, contact, or limited-contact sports Central or peripheral indwelling venous catheter might require special considerations for activities and emergency preparedness for unexpected trauma to the device(s) |
| Hepatitis, infectious (primarily hepatitis C) | Yes | All athletes should receive hepatitis B vaccination before participation. Because of the apparent minimal risk to others, all sports may be played as the athlete’s state of health allows For all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood |
| Liver, enlarged | Qualified yes | If the liver is acutely enlarged, participation should be avoided because of risk of rupture If the liver is chronically enlarged, individual assessment is needed before collision, contact, or limited-contact sports are played Patients with chronic liver disease can have changes in liver function that affect stamina, mental status, coagulation, or nutritional status |
| Diarrhea, infectious | Qualified no | Unless symptoms are mild and athlete is fully hydrated, no participation is permitted, because diarrhea can increase risk of dehydration and heat illness (see fever) |
| GENITOURINARY | ||
| Kidney, absence of one | Qualified yes | Athlete needs individual assessment for contact, collision, and limited-contact sports Protective equipment can reduce risk of injury to the remaining kidney sufficiently to allow participation in most sports, providing such equipment remains in place during the activity |
| Ovary, absence of one | Yes | Risk of severe injury to remaining ovary is minimal |
| Pregnancy and postpartum period | Qualified yes | Athlete needs individual assessment As pregnancy progresses, modifications to usual exercise routines become necessary; activities with high risk of falling or abdominal trauma should be avoided Scuba diving and activities posing risk of altitude sickness should also be avoided during pregnancy After the birth, physiologic and morphologic changes of pregnancy take 4-6 wk to return to baseline |
| Testicle, undescended or absence of one | Yes | Certain sports require a protective cup |
| NEUROLOGIC | ||
| Cerebral palsy | Qualified yes | Athlete needs evaluation to assess functional capacity to perform sports-specific activity |
| History of serious head or spine trauma or abnormality, including craniotomy, epidural bleeding, subdural hematoma, intracerebral hemorrhage, second-impact syndrome, vascular malformation, and neck fracture | Qualified yes | Athlete needs individual assessment for collision, contact, or limited-contact sports |
| History of simple concussion (mild traumatic brain injury), multiple simple concussions, and/or complex concussion | Qualified yes | Athlete needs individual assessment Research supports a conservative approach to concussion management, including no athletic participation while symptomatic or when deficits in judgment or cognition are detected, followed by graduated return to full activity |
| Recurrent headaches | Yes | Athlete needs individual assessment |
| Seizure disorder, well controlled | Yes | Risk of seizure during participation is minimal |
| Seizure disorder, poorly controlled | Qualified yes | Athlete needs individual assessment for collision, contact, or limited-contact sports The following noncontact sports should be avoided: archery, riflery, swimming, weightlifting, power lifting, strength training, and sports involving heights; in these sports, a seizure during activity can pose a risk to self or others |
| Recurrent plexopathy (burner or stinger) and cervical cord neuropraxia with persistent defects | Qualified yes | Athlete needs individual assessment for collision, contact, or limited-contact sports; regaining normal strength is an important benchmark for return to play |
| RESPIRATORY | ||
| Pulmonary compromise, including cystic fibrosis | Qualified yes | Athlete needs individual assessment but, generally, all sports may be played if oxygenation remains satisfactory during graded exercise test Athletes with cystic fibrosis need acclimatization and good hydration to reduce risk of heat illness |
| Asthma | Yes | With proper medication and education, only athletes with severe asthma need to modify their participation For those using inhalers, recommend having a written action plan and using a peak flowmeter daily Athletes with asthma might encounter risks when scuba diving |
| Acute upper respiratory infection | Qualified yes | Upper respiratory obstruction can affect pulmonary function Athlete needs individual assessment for all except mild disease (see Fever) |
| RHEUMATOLOGIC | ||
| Juvenile rheumatoid arthritis | Qualified yes | Athletes with systemic or polyarticular juvenile rheumatoid arthritis and history of cervical spine involvement need radiographs of C1 and C2 to assess risk of spinal cord injury Athletes with systemic or HLA-B27–associated arthritis require cardiovascular assessment for possible cardiac complications during exercise For those with micrognathia (open bite and exposed teeth), mouth guards are helpful If uveitis is present, risk of eye damage from trauma is increased; ophthalmologic assessment is recommended In visually impaired athletes, guidelines for functionally 1-eyed athletes should be followed |
| Juvenile dermatomyositis, idiopathic myositis | Qualified yes | Athlete with juvenile dermatomyositis or systemic lupus erythematosis with cardiac involvement requires cardiology assessment before participation. Athletes receiving systemic corticosteroid therapy are at higher risk for osteoporotic fractures and avascular necrosis, which should be assessed before clearance; those receiving immunosuppressive medications are at higher risk for serious infection. Sports activities should be avoided when myositis is active. Rhabdomyolysis during intensive exercise can cause renal injury in athletes with idiopathic myositis and other myopathies. Because of photosensitivity with juvenile dermatomyositis and systemic lupus erythematosus, sun protection is necessary during outdoor activities. With Raynaud phenomenon, exposure to the cold presents risk to hands and feet |
| Systemic lupus erythematosus | Qualified yes | |
| Raynaud phenomenon | Qualified yes | |
| SICKLE CELL | ||
| Sickle cell disease | Qualified yes | Athlete needs individual assessment In general, if illness status permits, all sports may be played; however, any sport or activity that entails overexertion, overheating, dehydration, or chilling should be avoided Participation at high altitude, especially when not acclimatized, also poses risk of sickle cell crisis |
| Sickle cell trait | Yes | Athletes with sickle cell trait generally do not have increased risk of sudden death or other medical problems during athletic participation under normal environmental conditions; however, when high exertional activity is performed under extreme conditions of heat and humidity or increased altitude, such catastrophic complications have occurred rarely Athletes with sickle cell trait, like all athletes, should be progressively acclimatized to the environment and to the intensity and duration of activities and should be sufficiently hydrated to reduce the risk of exertional heat illness and/or rhabdomyolysis According to National Institutes of Health management guidelines, sickle cell trait is not a contraindication to participation in competitive athletics, and there is no requirement for screening before participation More research is needed to fully assess potential risks and benefits of screening athletes for sickle cell trait |
This table is intended for use by medical and nonmedical personnel. “Needs evaluation” means that a physician with appropriate knowledge and experience should assess the safety of a given sport for an athlete with the listed medical condition. Unless otherwise noted, this need for special consideration is because of variability in the severity of the disease, the risk of injury for the specific sports, or both.
From Rice SG; the Council on Sports Medicine and Fitness, American Academy of Pediatrics: Medical conditions affecting sports participation, Pediatrics 121:841–848, 2008.
Sudden death during sports can result from undetected cardiac disease such as hypertrophic or other cardiomyopathies, anomalous coronary vessels, or a ruptured aorta in Marfan syndrome (Chapter 693). In many cases, the underlying heart disease is not suspected, and death is the first sign of heart disease (Chapter 430). Chest radiographs, electrocardiograms (ECGs), and echocardiograms are not recommended as routine screening tests. If there is a suspicion of heart disease, such as a history of syncope, presyncope, palpitations, or excessive dyspnea with exercise, or a family history of a condition such as hypertrophic cardiomyopathy or prolonged QT or Marfan syndrome, the evaluation should be complete and include a 12-lead ECG, an echocardiogram, Holter or event-capture monitoring, and a stress test with electrocardiographic monitoring. Recommendations for participation with identified cardiac disease should be made in consultation with a cardiologist.
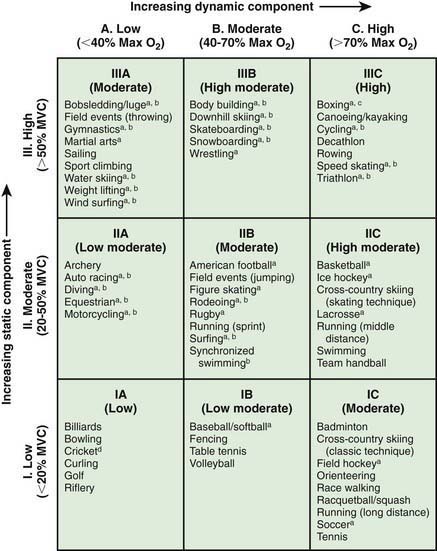
Disqualification and limitations for sports participation among various medical conditions are available from the American Academy of Pediatrics (see Table 678-2). Sports may also be classified by intensity (Fig. 678-1) and contact (Table 678-3). Athletes may seek to participate in sports against medical advice and have done so successfully for professional sports. Section 504(a) of the Rehabilitation Act of 1973 prohibits discrimination against disabled athletes if they have capabilities or skills required to play a competitive sport. This was reinforced through the Americans with Disabilities Act of 1990. An amateur athlete has no absolute right to decide whether to participate in competitive sports. Participation in competitive sports is considered a privilege, not a right. Knapp v Northwestern University established that “difficult medical decisions involving complex medical problems can be made by responsible physicians exercising prudent judgment (which will be necessarily conservative when definitive scientific evidence is lacking or conflicting) and relying on the recommendations of specialist consultants or guidelines established by a panel of experts.”
Table 678-3 CLASSIFICATION OF SPORTS BY CONTACT
CONTACT OR COLLISION
LIMITED CONTACT
NONCONTACT
* Participation not recommended by the American Academy of Pediatrics.
† The American Academy of Pediatrics recommends limiting the amount of body checking allowed for hockey players ≤15 yr to reduce injuries.
‡ A race (contest) in which competitors use a map and compass to find their way through unfamiliar territory.
From the American Academy of Pediatrics, Committee on Sports Medicine and Fitness: Medical conditions affecting sports participation, Pediatrics 107:1205, 2001.
Advisory Committee Physical Activity. Guidelines Advisory Committee Report 2008 to the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev. 2009;67:114-120.
American Academy of Pediatrics, American Academy of Family Physicians, American Medical Society for Sports Medicine, American Orthopedic Society for Sports Medicine, American Osteopathic Association for Sports Medicine. Preparticipation physical evaluation monograph, ed 3. Minneapolis: McGraw-Hill Medical Publishing; 2004.
Anderson SJ. Sports injuries. Curr Prob Pediatr Adolesc Health Care. 2005;35:105-176.
Brenner JS, Council on Sports Medicine and Fitness. Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics. 2007;119:1242-1245.
Brooks JHM, Erith SJ. Warm-up programmes in sport. BMJ. 2009;338:61-62.
Jonhagen S, Ackermann P, Erikssin T, et al. Sports massage after eccentric exercise. Am J Sports Med. 2004;32:1499-1503.
Knowles SB. Is there an injury epidemic in girls’ sports? Br J Sports Med. 2010;44:38-44.
MacAuley D, Best TM. Reducing risk of injury due to exercise. Br Med J. 2002;325:451-452.
Olsen OE, Myklebust G, Engebretsen L, et al. Exercises to prevent lower limb injuries in youth sports: cluster randomized controlled trial. Br Med J. 2005;330:449-452.
Rice SG, Council on Sports Medicine and FitnessAmerican Academy of Pediatrics. Medical conditions affecting sports participation. Pediatrics. 2008;121:841-848.