Chapter 706 Envenomations
General Approach to the Envenomated Child
Snake Bites
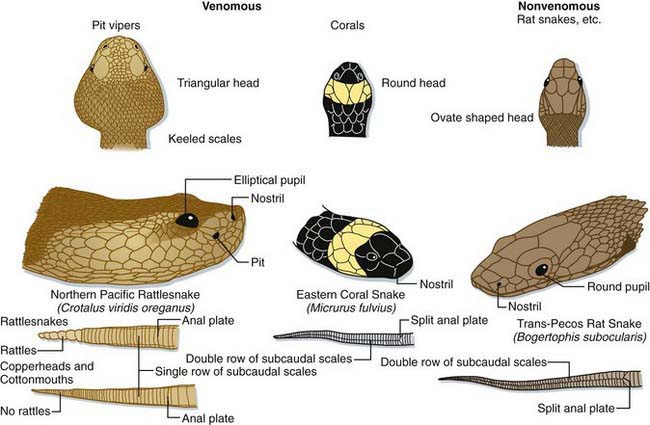
Most snake bites are inflicted by nonvenomous species and are of no more consequence than a potentially contaminated puncture wound (Fig. 706-1). Venomous snakes, however, kill many tens of thousands of people in the world each year. The precise number is difficult to ascertain, because the toll in human suffering is far greatest in developing nations. Developed nations, with established medical care systems, have relatively few fatalities each year.
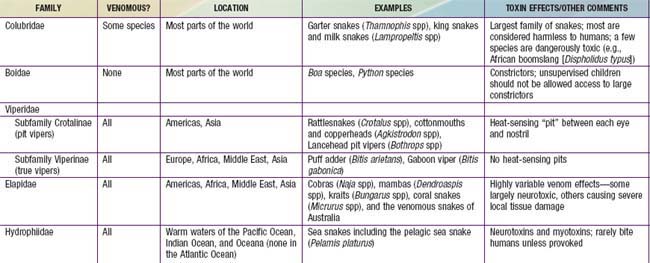
Most of the world’s medically significant venomous snakes belong to one of two families—Viperidae and Elapidae (Table 706-1). In developing nations, most snake envenomations occur in agricultural workers who inadvertently contact snakes while in the fields. Many victims of snake envenomation in developed nations are adolescent or young adult males, frequently intoxicated, who are attempting to handle or catch the snake. Bites are located on an extremity in over 95% of cases. In the USA, approximately 98% of venomous snake bites are inflicted by pit vipers (family Viperidae; subfamily Crotalinae). A small fraction of bites are caused by coral snakes (family Elapidae) in the South and Southwest, and by exotic snakes that have been imported.
Venoms and Effects
Snake venoms are complex mixtures of proteins including large enzymes that cause local tissue destruction and low molecular weight polypeptides that have the more lethal systemic effects. The symptoms and severity of an envenomation vary according to the type of snake, the amount of venom injected, and the location of the bite. The fear caused by a snake bite can result in nausea, vomiting, diarrhea, cold/clammy skin, and even syncope regardless of whether or not venom was injected. In general, viper venoms can have deleterious effects on almost any organ system. Most viper bites cause significant local pain, swelling, ecchymosis, and variable necrosis of the bitten extremity (Fig. 706-2). The pain and swelling typically begin quickly after the bite and progress over hours to days. Serious envenomations may result in a consumptive coagulopathy, hypotension, and respiratory distress. In contrast, venoms from the Elapidae tend to be more neurotoxic with little or no local tissue damage. These bites cause variable local pain and the onset of systemic effects can be delayed for hours. Manifestations of neurotoxicity generally begin with cranial nerve palsies such as ptosis, dysarthria, and dysphagia and may progress to respiratory failure and complete paralysis. There are exceptions; some members of the Elapidae family cause little or no neurotoxicity but rather severe tissue necrosis (e.g., African spitting cobras). Some vipers cause significant neurotoxicity (e.g., some populations of the Mohave rattlesnake [Crotalus scutulatus]). Physicians should proactively learn the important species in their regions, including how the species can be identified, the expected effects of their venoms, and proper approaches to management.
Management
Indications for administering antivenom can be found in Table 706-2.
| Evidence of systemic toxicity: | |
| Hemodynamic or respiratory instability | Hypotension, respiratory distress |
| Hemotoxicity | Clinically significant bleeding or abnormal coagulation studies |
| Neurotoxicity | Any evidence of toxicity: usually beginning with cranial nerve abnormalities and progressing to descending paralysis including the diaphragm |
| Evidence of local toxicity | Progressive soft tissue swelling |
Spider Bites
Neurotoxic Spiders
Venoms and Effects
Neurotoxic spiders all possess venoms that act at neural synapses, both at neuromuscular junctions and at autonomic nervous system junctions. All of the widow spiders (Latrodectus spp, including the well-studied black widow [Latrodectus mactans; Fig. 706-3)] and the Australian red-back spider [Latrodectus hasseltii]) possess very similar venoms, with the most important neurotoxin being α-latrotoxin. The neurotoxin of the Sydney funnel web spider (Atrax robustus) is robustoxin.
Necrotizing Spiders
Venoms and Effects
Although many spiders may cause a small amount of local tissue damage after their bites, the spiders most notorious for their dermonecrotic potential are the violin or recluse spiders of the genus Loxosceles. The best known member of this genus is the brown recluse (Loxosceles reclusa) (Fig. 706-4), found in the midwestern and southern portions of the USA. The venom of Loxosceles spiders contains a phospholipase enzyme, sphingomyelinase D, which attacks cell membranes and can cause local tissue damage that can occasionally be severe. The bite of this spider is generally painless and initially goes unnoticed. A few hours after the bite, pain related to focal ischemia begins at the site. Within a day, the site may have a central clear or blood-filled vesicle with surrounding ecchymosis and a rim of pale ischemia. The lesion may gradually expand over a period of days to weeks until necrotic tissue sloughs and healing begins.
Hymenoptera Stings
Venoms and Effects
Hymenoptera venoms, mixtures of proteins and vasoactive substances, are not very potent. Most stings result in only local pain, redness, and swelling, followed by itching and resolution. Some patients experience a large local reaction in which swelling progresses beyond the sting site, possibly involving the entire extremity. Approximately 0.4-0.8% of children are at risk for acute, life-threatening reactions due to hymenoptera venom sensitivity. Each year, an estimated 50-150 people in the USA die of allergic anaphylaxis caused by hymenoptera stings (Chapter 64). Rare cases of delayed serum sickness can follow hymenoptera stings. Finally, with the spread of Africanized honey bees (Apis mellifera scutellata), massive stinging episodes resulting in systemic venom toxicity (hypotension, respiratory failure, shock, hemolysis, and renal failure) appear to be increasing in Latin America and the southwestern U.S. states.
Auerbach PS. Envenomation by aquatic invertebrates. In: Auerbach PS, editor. Wilderness medicine. ed 5. St Louis: Mosby; 2007:1691-1729.
Auerbach PS. Envenomation by aquatic vertebrates. In: Auerbach PS, editor. Wilderness medicine. ed 5. St Louis: Mosby; 2007:1730-1749.
Bawaskar HS, Bawaskar PM. Efficacy and safety of scorpion antivenom plus prazosin compared with prazosin alone for venomous scorpion (Mesobuthus tamulus) sting: randomised open label clinical trial. BMJ. 2010;341:c7136.
Boyer LV, Theodorou AA, Berg RA, et al. Antivenom for critically ill children with neurotoxicity from scorpion stings. N Engl J Med. 2009;360:2090-2098.
Bronstein AC, Spyker DA, Cantilena LRJr, et al. 2007 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol (Phila). 2008;46:927-1057.
Gold BS, Dart RC, Barish RA, et al. Bites of venomous snakes. N Engl J Med. 2002;347:347-356.
Gutierrez JM, Lomonte B, Leon G, et al. Trends in snakebite envenomation therapy: scientific, technological and public health considerations. Curr Pharm Design. 2007;13:2935-2950.
McDade J, Aygun B, Ware RE. Brown recluse spider (Loxosceles reclusa) envenomation leading to acute hemolytic anemia in six adolescents. J Pediatr. 2010;156:155-157.
Mills EJ, Ford N. Research into scorpion stings. BMJ. 2011;342:c7369.
Moffitt JE, Golden DBK, Reisman RE, et al. Stinging insect hypersensitivity: a practice parameter update. J Allergy Clin Immunol. 2004;114:869-886.
Morocco A, Morocco A. Sea urchin envenomation. Clin Toxicol. 2005;43:119-120.
Norris RL, Bush SP. Bites by venomous reptiles in the Americas. In: Auerbach PS, editor. Wilderness medicine. ed 5. St Louis: Mosby; 2007:1051-1085.
Simpson ID, Norris RL. The global snakebite crisis—a public health issue misunderstood, not neglected. Wild Environ Med. 2009;20:43-46.
Singer AJ, Dagum AB, Singer AJ, et al. Current management of acute cutaneous wounds. N Engl J Med. 2008;359:1037-1046.
Swanson DL, Vetter RS, Swanson DL, et al. Bites of brown recluse spiders and suspected necrotic arachnidism. N Engl J Med. 2005;352:700-707.
Warrell DA. Snake bite. Lancet. 2010;375:77-86.
Williams D, Gutierez JM, Harrison R, et al. The global snake bite initiative: an antidote for snake bite. Lancet. 2010;375:89-91.
World Health Organization. Snake antivenom immunoglobulins (website). www.who.int/bloodproducts/snakeantivenoms. Accessed December 3, 2010
World Health Organization. Venomous snakes distribution and species risk categories (website). http://apps.who.int/bloodproducts/snakeantivenoms/database/. Accessed December 3, 2010