Enterobacteriaceae
I Defining and Differential Properties of Enteric Bacteria
• All Enterobacteriaceae are gram-negative rods, which contain lipopolysaccharide (LPS) in their cell envelope.
• Most have flagella and are motile.
2. Biochemical and growth properties
• All ferment glucose and are oxidase negative.
• Lactose-fermenting genera are generally benign
• Non–lactose-fermenting genera may be more pathogenic.
• All are facultative anaerobes, permitting survival in the gastrointestinal (GI) tract.
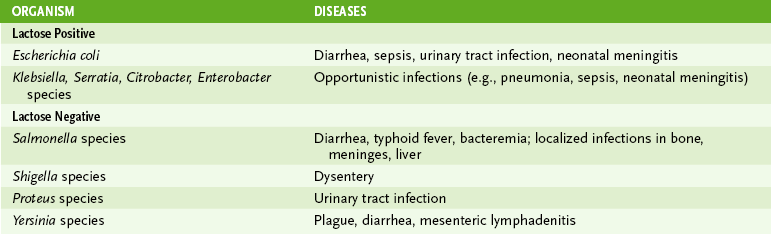
• Growth on differential media distinguishes Enterobacteriaceae from gram-positive organisms and from each other (Table 11-1).
1. Endotoxin, a part of the LPS produced by all Enterobacteriaceae, is responsible for many of the systemic manifestations of infection.
2. Exotoxins, produced by some species and strains, cause diarrhea.
3. Adhesins and fimbriae on some species promote adhesion to the colon, bladder, or other tissues.
4. Intracellular growth (Shigella, Salmonella and Yersinia species and enteroinvasive Escherichia coli) protects organisms from host defenses.
5. Antibiotic resistance develops rapidly and often is encoded on plasmids, which can be transferred to related bacteria.
6. Capsule on Klebsiella and Salmonella species is antiphagocytic.
7. The genes for many of the virulence factors are clustered and coordinately controlled within pathogenicity islands.
C Distribution and infection (Table 11-2)
1. Enterobacteriaceae are found worldwide in soil, water, and vegetation.
2. They are part of the normal intestinal flora of animals and humans.
• Salmonella, Shigella, and Yersinia species are invasive and always associated with disease in humans.
• Disease is acquired from animal reservoirs or human carriers.
• E. coli and Klebsiella, Enterobacter, and Proteus species, and other enteric bacteria are generally noninvasive and part of the normal flora in humans.
• Disease occurs when these organisms are introduced into normally sterile sites.
• Immunocompromised and debilitated patients are at greatest risk for disease. Some strains have acquired specific virulence factors that increase their pathogenicity.
II Lactose-Fermenting Enterobacteriaceae
a. Endotoxin is present in all strains
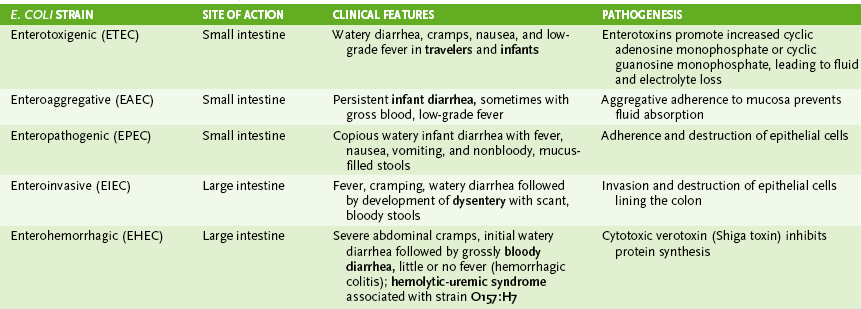
b. Noncytotoxic enterotoxins: enterotoxigenic strains (ETEC)
1) Heat-labile (LT) enterotoxin causes increased cyclic adenosine monophosphate (cAMP) levels, leading to altered electrolyte transport and diarrhea.
2) Heat-stabile (ST) enterotoxin stimulates cyclic guanosine monophosphate (cGMP) production, leading to fluid loss and diarrhea.
c. Enterohemorrhagic strains (EHEC)
d. Enteroinvasive strains (EIEC)
e. Enteropathogenic strains (EPEC) and enteroaggregative strains (EAEC)
a. Complication of gastroenteritis caused by EHEC (e.g., strain O157:H7), which occurs primarily in children
b. Associated with ingestion of contaminated undercooked hamburgers and other beef products
c. Marked by acute renal failure, thrombocytopenia, and microangiopathic hemolytic anemia
a. Organisms enter from urinary or GI tracts.
b. E. coli is the most common gram-negative agent of septicemia (Box 11-1).
• Spontaneous peritonitis in adults with cirrhosis and ascites
III Non–Lactose-Fermenting Enterobacteriaceae
• Salmonella species are carried in the GI tract of many animals but are not part of the normal human flora. Numerous serotypes are recognized based on surface antigens.
2. Salmonella species diseases
• Enteritis (Salmonella enteritidis and other serotypes)
a. Incubation period is 6 to 48 hours.
b. Spontaneous resolution usually occurs within 2 to 7 days.
c. Symptoms include nausea, vomiting, and nonbloody diarrhea.
d. Symptomatic treatment, including rehydration, is sufficient.
• Typhoid (enteric) fever (Salmonella typhi)
a. After incubation period of 10 to 14 days, initial symptoms include steadily increasing fever, headache, myalgia, malaise, and anorexia.
b. Invasion of M cells in Peyer patches results in gastrointestinal symptoms (necrosis, hemorrhage, and perforation of intestinal wall) after the second week of illness.
• Bacteremia releases endotoxin causing fever and other systemic symptoms.
• Localized infections in other sites (e.g., osteomyelitis, meningitis)
• All four Shigella species are pathogenic in humans and cause similar disease manifestations.
• Invasion of colonic mucosa and replication within mucosal cells
2. Shigellosis (bacillary dysentery)
• Initial symptoms include profuse watery diarrhea, abdominal cramps, and fever.
• Tenesmus and the presence of blood, mucus, and polymorphonuclear leukocytes in stool are indicative of invasion of the bowel wall (ulcerative colitis).
• Yersinia pestis is carried by numerous small animals, including domestic cats, and can be transmitted to humans via flea vectors.
2. Diseases caused by Y. pestis
a. Acquired from bite of infected flea
b. Prairie dogs are reservoir for the pathogen.
c. Incubation period of 7 days
d. High fever, painful bubo (inflamed, swollen lymph node) in groin or axilla, conjunctivitis, bacteremia that can lead to death in untreated patients (mortality rate > 75%)
• Y. enterocolitica is carried in livestock, rabbits, and rodents and transmitted to humans in contaminated food, water, or blood products.
1. Enterocolitis (most common disease)
• Bloody diarrhea, fever, and abdominal pain usually last 1 or 2 weeks. Chronic form may last more than 1 year.