Perianal fistula in active setting usually T2 hyperintense, T1 hypointense and enhancing on T1 C+ MR
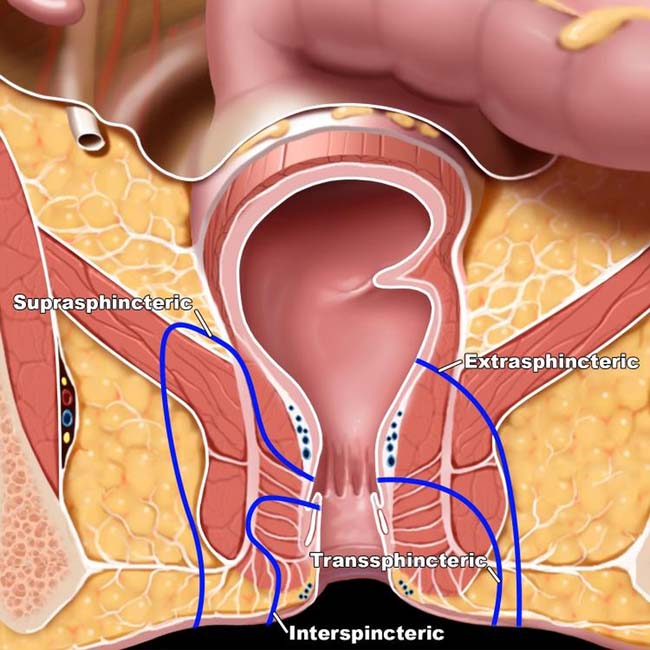
 Parks classification of perianal fistulas
Parks classification of perianal fistulas
– Intersphincteric fistula: Fistula traverses internal anal sphincter and extends downwards to skin surface
• Other fluoroscopic studies may have utility depending on location of fistulas (e.g., water soluble contrast enema for colovesical and colovaginal fistulas)
• CT: Detection of fistulas requires attention to both primary (e.g., direct fistulous tract filled with ectopic gas or contrast) and secondary (e.g., ectopic gas, abnormally tethered bowel loops) signs
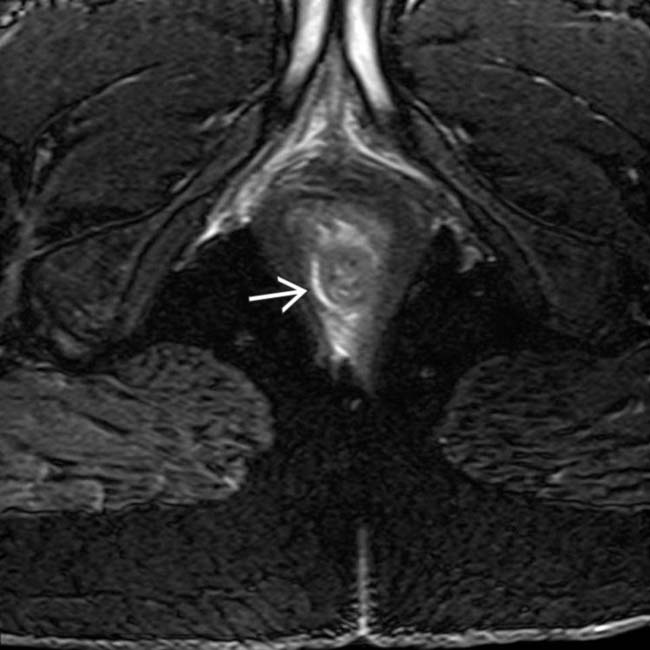
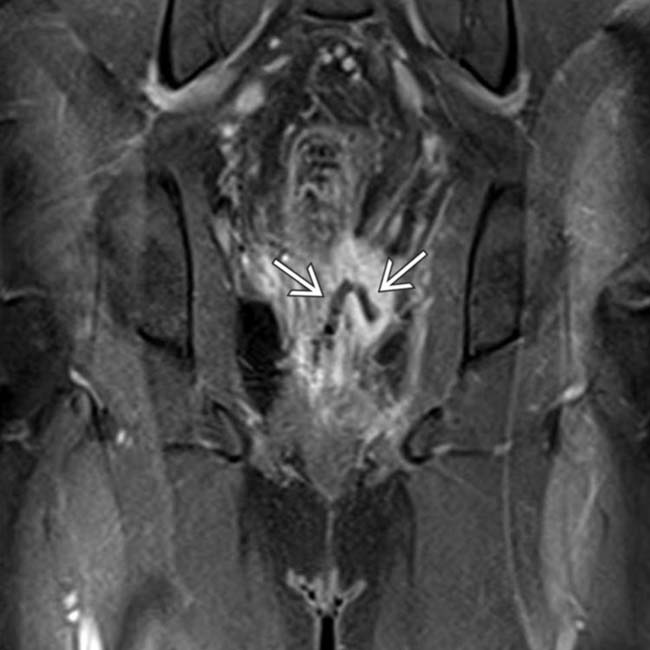
 in the intersphincteric space. The track is outside the internal sphincter, but does not cross the external sphincter, compatible with an intersphincteric perianal fistula.
in the intersphincteric space. The track is outside the internal sphincter, but does not cross the external sphincter, compatible with an intersphincteric perianal fistula.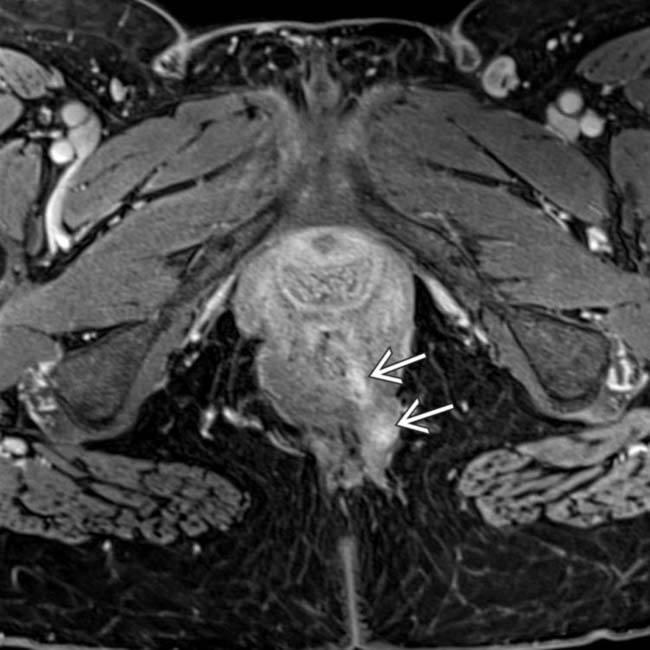
 arising from the anal canal at the 5-o’clock position. Enhancement along fistulous tracts suggests that the fistula is active, rather than chronic and healed.
arising from the anal canal at the 5-o’clock position. Enhancement along fistulous tracts suggests that the fistula is active, rather than chronic and healed.
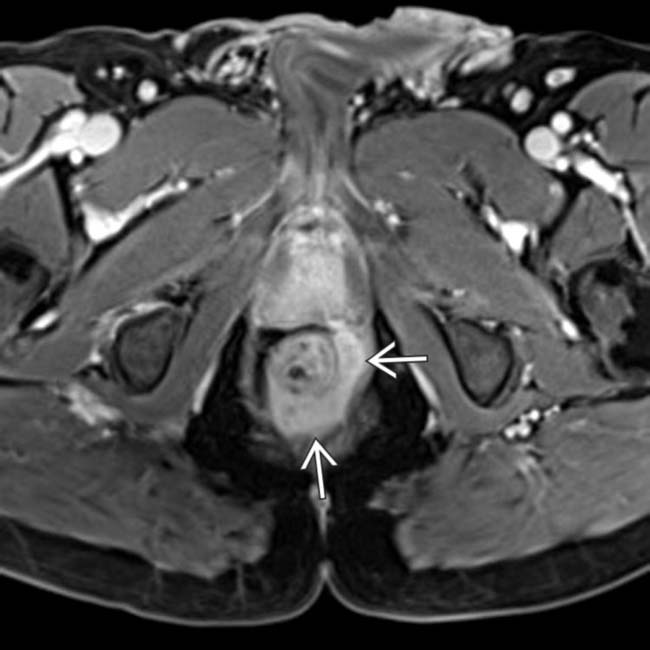
 . Seton catheters, often utilized to keep fistulous tracts open and facilitate drainage, appear low signal on all pulse sequences.
. Seton catheters, often utilized to keep fistulous tracts open and facilitate drainage, appear low signal on all pulse sequences.IMAGING
General Features
Imaging Recommendations
• Best imaging tool
 MR considered best modality for perianal fistulas and sinus tracts due to superior soft tissue resolution and ability to discriminate different anatomic components of perianal region
MR considered best modality for perianal fistulas and sinus tracts due to superior soft tissue resolution and ability to discriminate different anatomic components of perianal region
 MR considered best modality for perianal fistulas and sinus tracts due to superior soft tissue resolution and ability to discriminate different anatomic components of perianal region
MR considered best modality for perianal fistulas and sinus tracts due to superior soft tissue resolution and ability to discriminate different anatomic components of perianal region
MR Findings
• MR now considered imaging modality of choice for evaluation of perianal fistulas
 MR can determine relationship of fistulous tract with anal sphincters, identify exact site of opening of fistulous tract in anal canal, and differentiate fistulas which arise from distal rectum from those that arise from anal canal
MR can determine relationship of fistulous tract with anal sphincters, identify exact site of opening of fistulous tract in anal canal, and differentiate fistulas which arise from distal rectum from those that arise from anal canal
 MR can determine relationship of fistulous tract with anal sphincters, identify exact site of opening of fistulous tract in anal canal, and differentiate fistulas which arise from distal rectum from those that arise from anal canal
MR can determine relationship of fistulous tract with anal sphincters, identify exact site of opening of fistulous tract in anal canal, and differentiate fistulas which arise from distal rectum from those that arise from anal canal• MR protocol design (for perianal fistulas)
 High resolution T2-weighted images through perianal region are critical to diagnosis
High resolution T2-weighted images through perianal region are critical to diagnosis
 High resolution T2-weighted images through perianal region are critical to diagnosis
High resolution T2-weighted images through perianal region are critical to diagnosis
– Typically fat saturation (either frequency-selective fat saturation or inversion recovery/STIR) included in at least 1 plane
– High-resolution 3D T2-weighted images (i.e., T2 SPACE) are increasingly utilized to provide more precise delineation of fistulous tracts
• MR findings of perianal fistulas
 Active fistulas typically show enhancement on T1 C+ images, while old, healed fistulous tracts do not
Active fistulas typically show enhancement on T1 C+ images, while old, healed fistulous tracts do not
 Active fistulas typically show enhancement on T1 C+ images, while old, healed fistulous tracts do not
Active fistulas typically show enhancement on T1 C+ images, while old, healed fistulous tracts do not
• Classification of perianal fistulas
 Parks classification based primarily on surgical findings and secondarily applied to MR
Parks classification based primarily on surgical findings and secondarily applied to MR
 St. James University Hospital classification (based primarily on MR findings)
St. James University Hospital classification (based primarily on MR findings)
 Parks classification based primarily on surgical findings and secondarily applied to MR
Parks classification based primarily on surgical findings and secondarily applied to MR
– Intersphincteric fistula (45% of cases): Fistula traverses internal anal sphincter and extends downwards to skin surface (no involvement of external sphincter)
– Transsphincteric fistula (30% of cases): Fistula traverses both internal and external anal sphincters before extending through ischioanal fossa to skin surface
 St. James University Hospital classification (based primarily on MR findings)
St. James University Hospital classification (based primarily on MR findings)
Fluoroscopic Findings
• Upper GI
CT Findings
• Gut-to-gut fistula (e.g., enteroenteric, enterocolic, colocolic)
• Enterocutaneous fistula
• Colovesical fistula to thick-walled bladder
• Diverticulitis with fistula
• Pancreatitis with fistula
PATHOLOGY
General Features
• Etiology
 Surgical causes
Surgical causes
 Surgical causes
Surgical causes
– Probably represents most common cause; usually result from bowel injury during surgery, including inadvertant enterotomy, anastomotic leak, or erosion of foreign body into bowel
CLINICAL ISSUES
Presentation
• Most common signs/symptoms
 Enterocutaneous fistulas often present with fever, abdominal pain, distension, and drainage from wound (with signs of wound infection)
Enterocutaneous fistulas often present with fever, abdominal pain, distension, and drainage from wound (with signs of wound infection)
 Other symptoms include sepsis, pneumaturia (colovesical fistula), feces per vagina (rectovaginal fistula), diarrhea (due to fistulization to distal colon), bowel obstruction (due to inflammation from fistula), or gastrointestinal bleeding
Other symptoms include sepsis, pneumaturia (colovesical fistula), feces per vagina (rectovaginal fistula), diarrhea (due to fistulization to distal colon), bowel obstruction (due to inflammation from fistula), or gastrointestinal bleeding
 Enterocutaneous fistulas often present with fever, abdominal pain, distension, and drainage from wound (with signs of wound infection)
Enterocutaneous fistulas often present with fever, abdominal pain, distension, and drainage from wound (with signs of wound infection) Other symptoms include sepsis, pneumaturia (colovesical fistula), feces per vagina (rectovaginal fistula), diarrhea (due to fistulization to distal colon), bowel obstruction (due to inflammation from fistula), or gastrointestinal bleeding
Other symptoms include sepsis, pneumaturia (colovesical fistula), feces per vagina (rectovaginal fistula), diarrhea (due to fistulization to distal colon), bowel obstruction (due to inflammation from fistula), or gastrointestinal bleedingTreatment
• Fluid support, correction of electrolyte abnormalities, and antibiotics to treat underlying infection
• Enterocutaneous fistulas may close spontaneously with bowel rest, IV fluids, parenteral nutrition, ± somatostatin
• Internal gut-to-gut fistulas involving small or large bowel loops do not typically close spontaneously and often require surgical correction
• Perianal fistulas in patients with idiopathic fistulas usually surgically managed
 Preoperative knowledge of fistula’s relationship with sphincter complex is critical for preservation of continence
Preoperative knowledge of fistula’s relationship with sphincter complex is critical for preservation of continence
 Preoperative knowledge of fistula’s relationship with sphincter complex is critical for preservation of continence
Preoperative knowledge of fistula’s relationship with sphincter complex is critical for preservation of continence
 arising from the rectum above the levator muscle complex.
arising from the rectum above the levator muscle complex.
 in this patient arising in the supralevator space and directly crossing the levator muscle complex into the ischioanal fossa without involving the anal sphincters.
in this patient arising in the supralevator space and directly crossing the levator muscle complex into the ischioanal fossa without involving the anal sphincters.
 crossing the external sphincter and extending into the posterior soft tissues on the left. Notice that the fistula is contiguous with a large T2 hyperintense “horseshoe” type abscess
crossing the external sphincter and extending into the posterior soft tissues on the left. Notice that the fistula is contiguous with a large T2 hyperintense “horseshoe” type abscess  in the intersphincteric space.
in the intersphincteric space.
 and the fistula
and the fistula  .
.
 rising upward from the intersphincteric space into the supralevator space, before crossing the levator ani muscle complex, compatible with a suprasphincteric fistula.
rising upward from the intersphincteric space into the supralevator space, before crossing the levator ani muscle complex, compatible with a suprasphincteric fistula.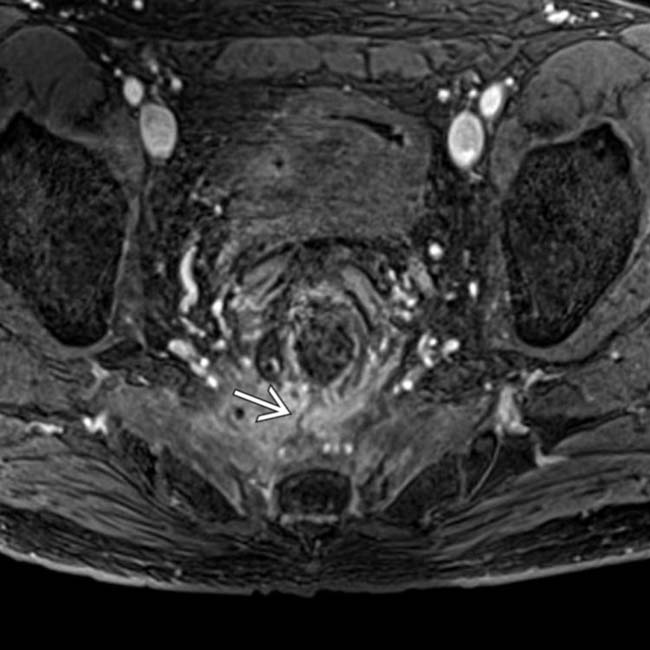
 extending posteriorly at the 6-o’clock position into the presacral space.
extending posteriorly at the 6-o’clock position into the presacral space.
 , and pericolonic infiltration in a 54-year-old woman with a long history of Crohn disease who developed foul-smelling vaginal discharge.
, and pericolonic infiltration in a 54-year-old woman with a long history of Crohn disease who developed foul-smelling vaginal discharge.
 .
.
 extending toward the vagina.
extending toward the vagina.
 and the vagina
and the vagina  through a fistulous tract
through a fistulous tract  starting low in the rectum. Contrast spilling out of the anus and vagina stains the overlying sheets.
starting low in the rectum. Contrast spilling out of the anus and vagina stains the overlying sheets.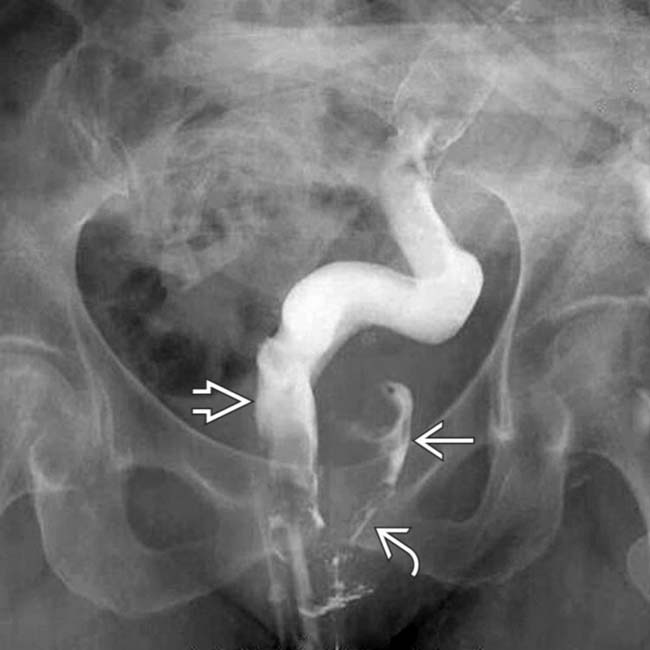
 , vagina
, vagina  , and fistula
, and fistula  .
.
 and vagina
and vagina  . Crohn disease is a common cause of spontaneous enteric fistulas, as it is a chronic, transmural inflammatory disease.
. Crohn disease is a common cause of spontaneous enteric fistulas, as it is a chronic, transmural inflammatory disease.
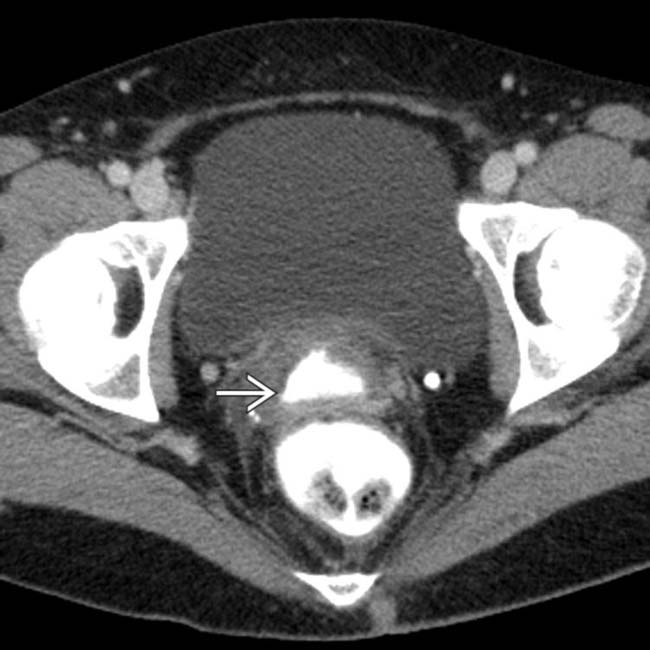
 in an elderly woman who presented with urinary sepsis and high fever. The colonic lumen is opacified by rectal contrast medium.
in an elderly woman who presented with urinary sepsis and high fever. The colonic lumen is opacified by rectal contrast medium.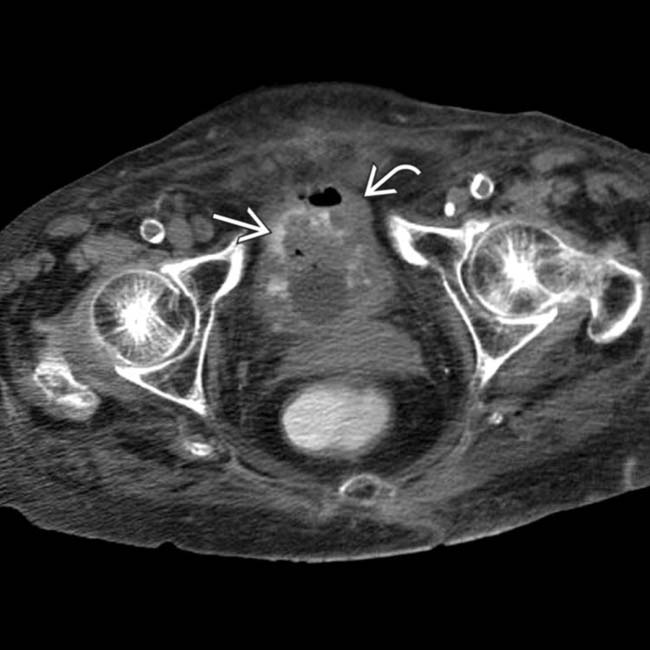
 that is filled with gas, particulate (fecal) debris, and rectally administered contrast medium
that is filled with gas, particulate (fecal) debris, and rectally administered contrast medium  , confirming a colovesical fistula. Diverticulitis was confirmed as the etiology.
, confirming a colovesical fistula. Diverticulitis was confirmed as the etiology.
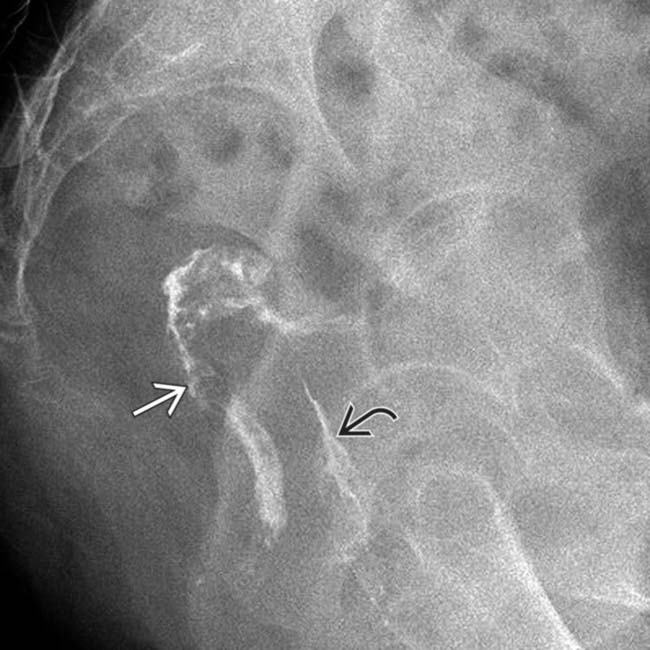
 in a 60-year-old woman who had undergone a prior hysterectomy and developed foul-smelling vaginal discharge.
in a 60-year-old woman who had undergone a prior hysterectomy and developed foul-smelling vaginal discharge.
 to the back wall of the vagina or cervix
to the back wall of the vagina or cervix  .
.
 , confirming a colovaginal fistula.
, confirming a colovaginal fistula.
 from the distal colon (or rectum)
from the distal colon (or rectum)  to the vagina (or cervix)
to the vagina (or cervix)  . Diverticulitis and hysterectomy are both associated with colovaginal fistula.
. Diverticulitis and hysterectomy are both associated with colovaginal fistula.
 , mucosal hyperenhancement, and extraluminal gas and fluid
, mucosal hyperenhancement, and extraluminal gas and fluid  .
.
 extending from the low rectum or anus toward the skin. These are characteristic features of Crohn disease. Please note that CT is far inferior to MR in both the identification and classification of perianal fistulas.
extending from the low rectum or anus toward the skin. These are characteristic features of Crohn disease. Please note that CT is far inferior to MR in both the identification and classification of perianal fistulas.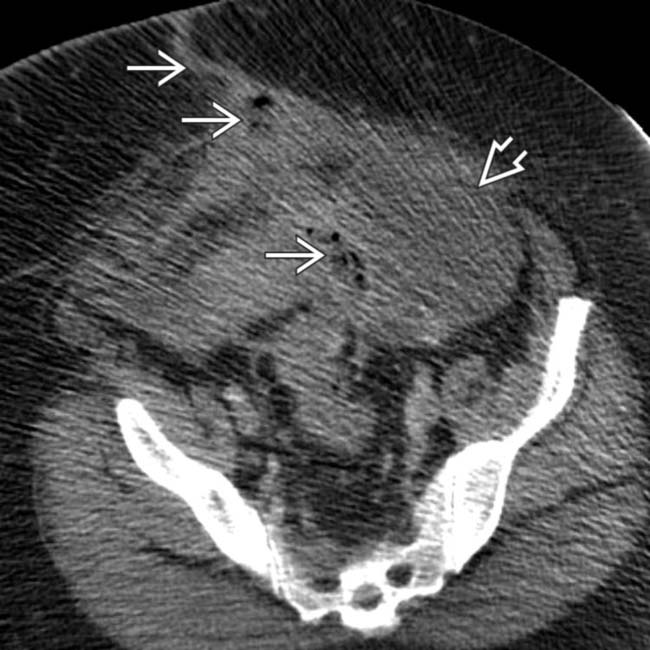
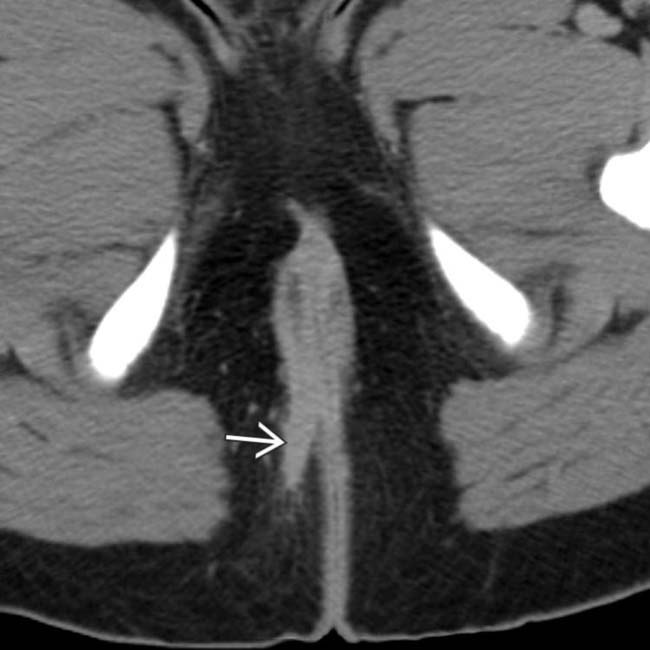
 adjacent to the sigmoid colon. There is a tract of gas and fluid
adjacent to the sigmoid colon. There is a tract of gas and fluid  leading to the anterior abdominal wall defect.
leading to the anterior abdominal wall defect.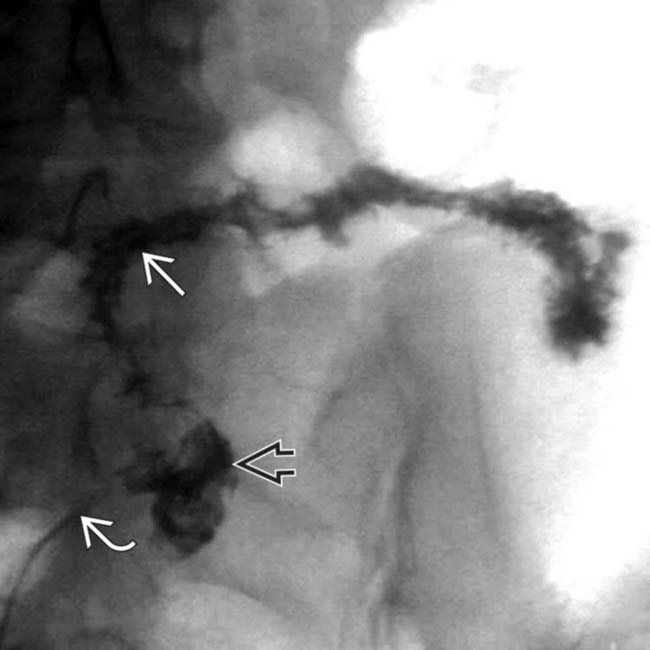
 inserted into the abdominal wall defect), in the same patient, opacifies an abdominal abscess cavity
inserted into the abdominal wall defect), in the same patient, opacifies an abdominal abscess cavity  and the sigmoid colon lumen
and the sigmoid colon lumen  . Diverticulitis was the etiology of this spontaneous colocutaneous fistula.
. Diverticulitis was the etiology of this spontaneous colocutaneous fistula.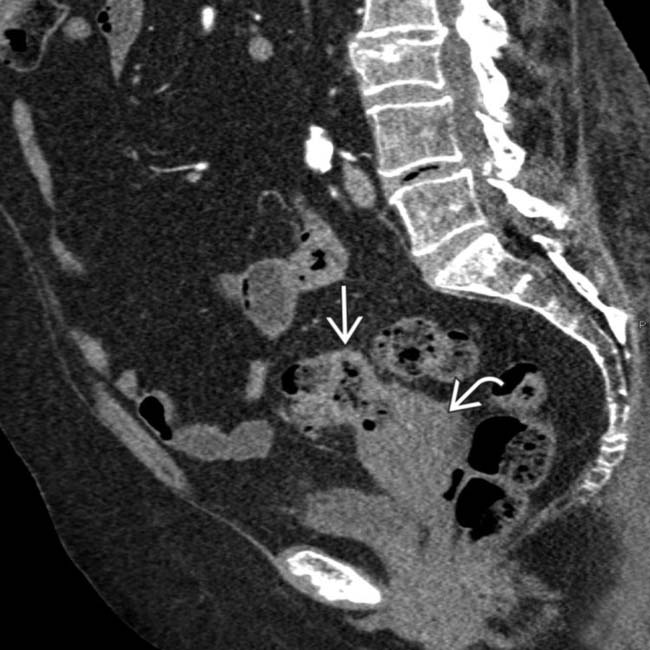
 and uterus
and uterus  near the fundus.
near the fundus.
 , including direct contact between the inflamed colon and the bladder, focal wall thickening of the bladder at the site of contact, and the presence of ectopic gas
, including direct contact between the inflamed colon and the bladder, focal wall thickening of the bladder at the site of contact, and the presence of ectopic gas  within the bladder lumen.
within the bladder lumen.


















































































