Chapter 10 Endovenous Approach to Recurrent Varicose Veins
Historical Background
Recurrence rates of varicose veins of 20% are common, with rates as high as 70% at 10 years.1–3 Up to 25% of procedures for varicose veins are performed for recurrent disease,4 thus placing considerable demands on health care resources. It is important to note that recurrent varicose vein surgery carries a much greater morbidity risk to the patient than does primary surgery.3 This risk is reduced markedly with endovenous techniques.
Etiology and Natural History of Disease
Patients who have had previous high ligation and stripping typically present with recurrent varicose veins; anatomic distribution of these veins is variable. Neovascularization is commonly seen following traditional stripping procedures and is thought to be secondary to “frustrated” venous drainage from the abdominal wall and perineum.5 Regardless of the mechanism, the result is recurrent reflux in the thigh or lower leg veins.
Multiple factors contribute in the development of recurrent disease. The weight of each factor has not yet been determined because there are no prospective studies with adequate sample size. The following descriptions are common etiologies seen at Miami Vein Center after clinical and color flow duplex imaging (CFDI) examinations are performed in patients presenting with recurrent varicose veins.
Pearls and Pitfalls
Previous High Ligation and Stripping
All patients with recurrent varicose veins should be evaluated with CFDI. Usually findings include neovascularity in the groin from which one or more tributary veins are found to descend the thigh. The tributary may attach to another tributary, a perforator, or a remnant of the great saphenous vein (GSV) in the thigh or calf (Fig. 10-1). The reflux extends into dilated tributaries of the skin; these vessels bulge and are palpable. In most cases, our approach is to enter any straight incompetent axial venous segments deep to the skin with a micropuncture access kit. These kits usually contain 4-Fr microsheaths, through which we place a 400- or 600-µm-diameter laser fiber. Perivenous tumescent anesthesia is placed, and the vein or veins are ablated in the usual manner. Because tortuous incompetent venous segments below the level of the skin do not allow the passage of guidewires, these are treated with ultrasound-guided foam sclerotherapy (Fig. 10-2).
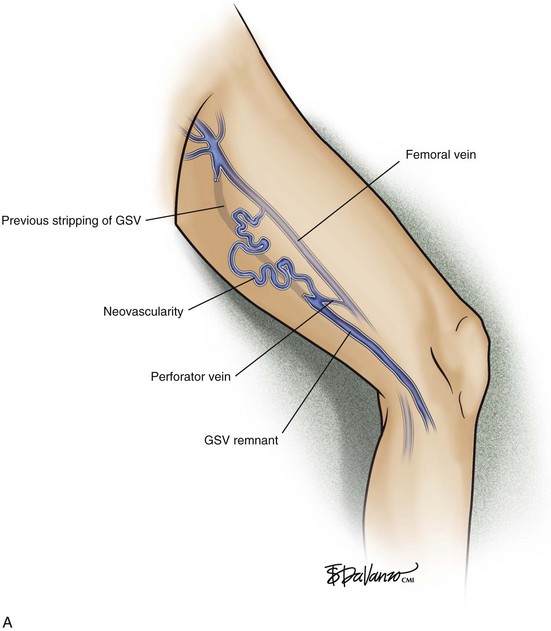

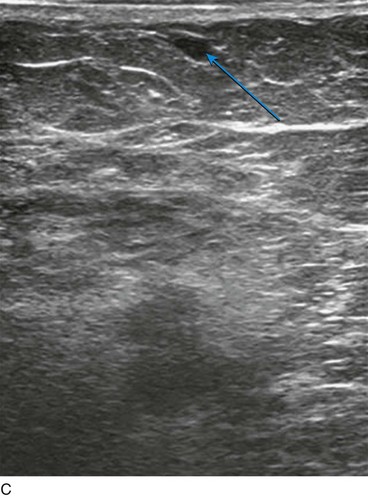
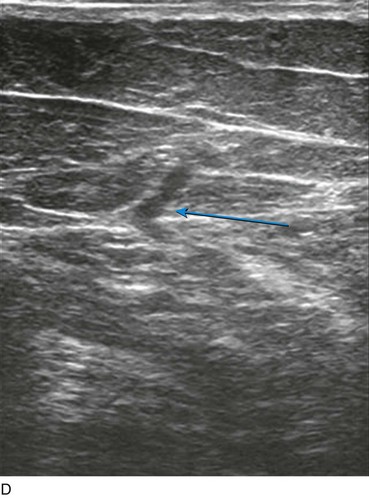
Fig 10–1 B, Treatment of recurrent varicose vein with the use of combination endovenous laser and foam scleropathy. C, Cross-sectional view of a subcutaneous tortuous tributary. These tortuous veins are ideal candidates for ultrasound-guided foam sclerotherapy treatment. D, Incompetent midthigh perforating vein is the source of the recurrent varicose veins, which is most effectively treated with thermal ablation if anatomically in a straight orientation. If oriented in a tortuous manner, however, ultrasound-guided foam sclerotherapy treatment is preferred.
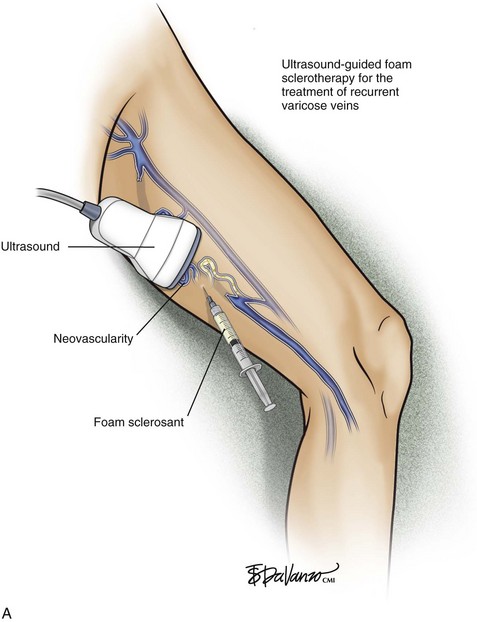

Fig 10–2 B, Ultrasound-guided foam sclerotherapy for the treatment of recurrent varicose veins; tortuous veins seen on ultrasound are in the background.
Finally, all bulging varicose veins that are palpable on the skin receive treatment with ambulatory phlebectomy. These three techniques, used concomitantly, yield very satisfactory results. These types of patients are told that the treatments are palliative and they likely will need “touch-up” treatments in the future.
Previous Phlebectomy Without GSV Stripping
Also common in our practice are patients presenting with recurrent varicose veins previously treated with phlebectomy only at an outside facility. These limbs, once examined with CFDI, usually have a large incompetent GSV descending from the groin and terminating ultimately in the calf at a site where large varicosities are noted. These patients do very well with routine GSV ablation using either radiofrequency or laser and using ambulatory phlebectomy for associated varicosities.
Previous Laser or Radiofrequency Ablation Without Phlebectomy
There are individuals who have seen other physicians and come to our practice with a history of GSV ablation that “worked temporarily.” That is, the venous cluster on the medial calf improved shortly after the procedure, but with time, the same cluster began filling and dilating. CFDI performed in our office usually shows successful ablation of the target GSV. However, the cluster of varicose veins in these cases has found a connection with an incompetent perforating vein. This is usually a Boyd perforating vein in the upper calf. This concept of an untreated “venous reservoir” dictates that other sources of reflux will eventually connect due to low venous resistance. Treatment involves either ultrasound-guided sclerotherapy or thermal ablation of the perforator (function of size) and ambulatory phlebectomy of the varicose clusters.
We have also seen cases in which two sources of venous hypertension from superficial axial vein reflux were identified preoperatively but only one was treated. In these cases usually only the incompetent GSV was ablated, and the incompetent anterior accessory saphenous vein was left untreated. There may be temporary improvement of the varicosities in direct continuity with the GSV; less direct varicosities may respond with minimal or no improvement. Our approach with these patients is thermal ablation of the anterior accessory saphenous vein followed by ambulatory phlebectomy at the same stage.
Previous GSV Ablation with No Improvement
When a patient has a history of previous GSV ablation performed at an outside facility and no improvement was observed by the patient, this should be a red flag that the patient was initially misdiagnosed. The majority of these cases were straightforward cases with classic SSV incompetence in the limbs; however, the original physician failed to view the posterior calf with CFDI. Ablation of the SSV with laser or radiofrequency energy in combination with ambulatory phlebectomy will quickly rectify this problem.
Gastrocnemial vein incompetence has a prevalence of up to 30% in patients with varicose veins. Most practitioners do not treat this vein. Also, incompetent perforators connecting through this vein at the posteromedial calf may be overlooked or missed. We have seen these as sources of recurrent varicose veins. Depending on the severity of the signs and symptoms of the disease, we may elect to treat gastrocnemius veins with ultrasound-guided sclerotherapy. Obviously, this adds controversy to the dearth of clinical information referable to this vein.
Comparative Effectiveness of Existing Treatments
There are no publications available that focus on endovenous treatment of recurrent varicose veins. The aforementioned techniques are self-taught techniques, applying standard endovenous principles. The adage developed by the author is “If an incompetent vein is straight—burn it; if it is tortuous—foam it; if the vein is palpable on the skin (straight or tortuous)—remove it with phlebectomy.”
Depicted in Figure 10-3 is an endovenous sheath inside a saphenous vein remnant (to deliver laser energy), with a syringe prepared with a foamed sclerosant attached to the sheath side-arm to deliver foam into an area of neovascularization—and the patient is marked for phlebectomy. We have had no complications with this approach in several hundred recurrent varicose vein cases. Recurrences after endovenous treatment develop secondary to progression of disease and are retreatable with the same approach.
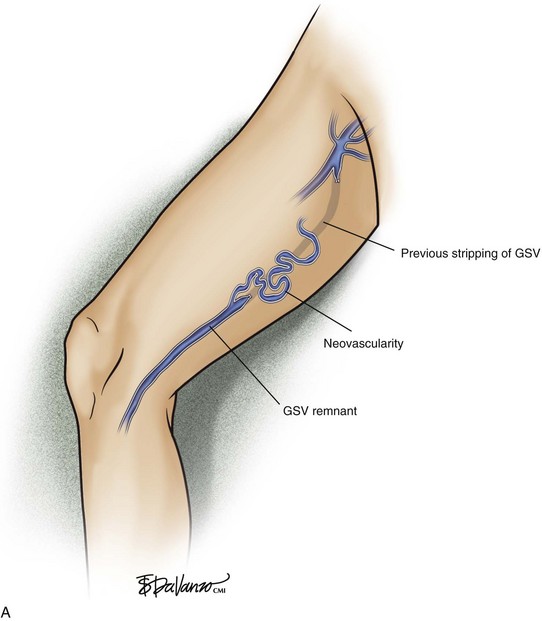
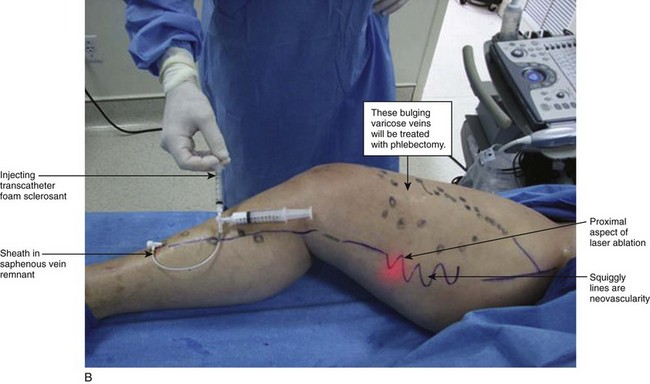
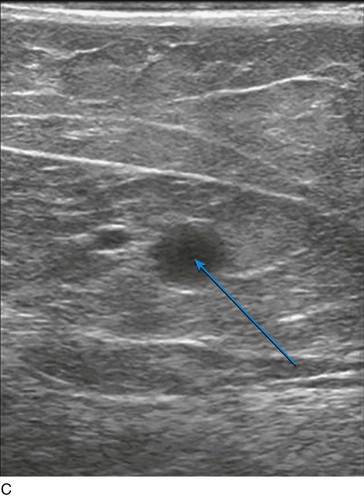
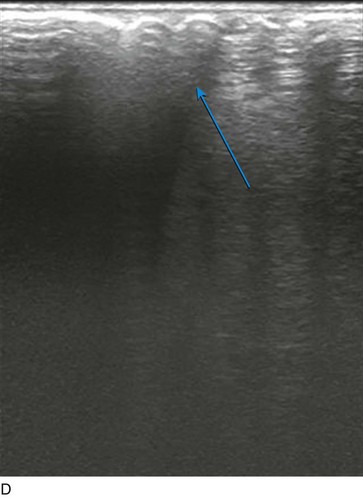
Fig 10–3 B, Recurrent varicose veins from neovascularity in upper thigh and a refluxing saphenous vein remnant. Treatment with a combination of ultrasound foam sclerotherapy, endovenous laser ablation, and ambulatory phlebectomy. C, Arrow points to saphenous vein remnant. D, Arrow points to foam-filled varicose veins just below skin surface.
1 Negus D. Recurrent varicose veins; a national problem. Br J Surg. 1993;80:823-824.
2 Rivlin S. The surgical cure of primary varicose veins. Br J Surg. 1975;62:913-917.
3 Royle JP. Recurrent varicose veins. World J Surg. 1986;10:944-953.
4 Hayden A, Holdsworth J. Complications following re-exploration of the groin for recurrent varicose veins. Ann R Coll Surg Engl. 2001;83:272-273.
5 Chandler JG, Pichot O, Sessa C, et al. Treatment of primary venous insufficiency by endovenous saphenous vein obliteration. Vasc Surg. 2000;34:201-214.
[/level-membership-for-surgery-category]
Chapter 10 Endovenous Approach to Recurrent Varicose Veins
Historical Background
Recurrence rates of varicose veins of 20% are common, with rates as high as 70% at 10 years.1–3 Up to 25% of procedures for varicose veins are performed for recurrent disease,4 thus placing considerable demands on health care resources. It is important to note that recurrent varicose vein surgery carries a much greater morbidity risk to the patient than does primary surgery.3 This risk is reduced markedly with endovenous techniques.
Etiology and Natural History of Disease
Patients who have had previous high ligation and stripping typically present with recurrent varicose veins; anatomic distribution of these veins is variable. Neovascularization is commonly seen following traditional stripping procedures and is thought to be secondary to “frustrated” venous drainage from the abdominal wall and perineum.5 Regardless of the mechanism, the result is recurrent reflux in the thigh or lower leg veins.
Multiple factors contribute in the development of recurrent disease. The weight of each factor has not yet been determined because there are no prospective studies with adequate sample size. The following descriptions are common etiologies seen at Miami Vein Center after clinical and color flow duplex imaging (CFDI) examinations are performed in patients presenting with recurrent varicose veins.
Pearls and Pitfalls
Previous High Ligation and Stripping
All patients with recurrent varicose veins should be evaluated with CFDI. Usually findings include neovascularity in the groin from which one or more tributary veins are found to descend the thigh. The tributary may attach to another tributary, a perforator, or a remnant of the great saphenous vein (GSV) in the thigh or calf (Fig. 10-1). The reflux extends into dilated tributaries of the skin; these vessels bulge and are palpable. In most cases, our approach is to enter any straight incompetent axial venous segments deep to the skin with a micropuncture access kit. These kits usually contain 4-Fr microsheaths, through which we place a 400- or 600-µm-diameter laser fiber. Perivenous tumescent anesthesia is placed, and the vein or veins are ablated in the usual manner. Because tortuous incompetent venous segments below the level of the skin do not allow the passage of guidewires, these are treated with ultrasound-guided foam sclerotherapy (Fig. 10-2).
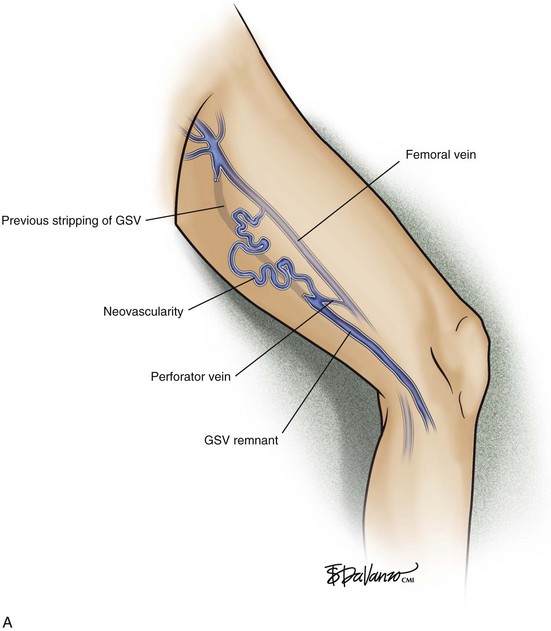

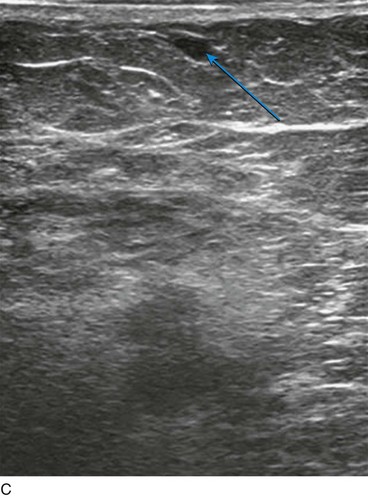
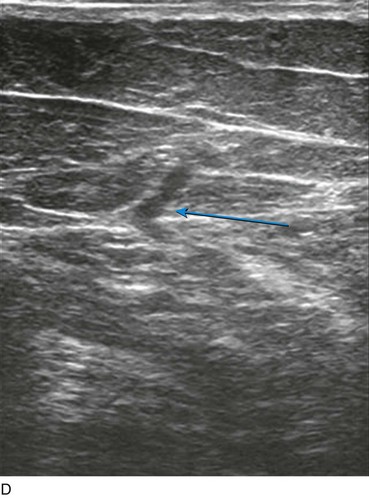
Fig 10–1 B, Treatment of recurrent varicose vein with the use of combination endovenous laser and foam scleropathy. C,