Chapter 31 Endobutton Anterior Cruciate Ligament Reconstruction Femoral Fixation
Biomechanics
Numerous studies have analyzed the pullout strength and stiffness of this device.1–7 Much was made at one point about a so-called “bungee effect,” in which the device’s fixation on the cortex and not in the tunnel supposedly resulted in lower stiffness. However, it has subsequently been shown that the greater stiffness resulting from cortical anchorage dwarfs the slightly reduced stiffness from the greater length of the construct.7 Also, as described elsewhere in the text, stiffness has no bearing on ultimate stability. This is because the stiffness of all grafts is independent of their mode of fixation once tunnel healing has occurred at about 2 months postoperatively. After this time, load is borne by the healed fibers that connect the graft to the tunnel, not by the device. Because the fixation device is not load bearing after this time, its stiffness is irrelevant. However, even before that time, stiffness is less important because the stiffness represents only elastic deformation of the graft. It is only plastic deformation, not elastic deformation, that will result in greater ultimate clinical laxity. In fact, reduced stiffness, or greater elasticity, in the graft-fixation construct will diminish the forces that tend to displace the fixation device in cyclical loading. This reduction in stiffness diminishes these forces by partially dissipating them in temporary elastic deformation of the graft. Therefore, ultimately, stability may actually be enhanced by protecting the construct from plastic deformation or fixation device slippage while tunnel healing is occurring.
Clinical Results
In the largest meta-analysis of anterior cruciate ligament reconstruction (ACLR) autografts, the EB-hamstring combination was found to have the highest stability rates of any graft-fixation construct when paired with modern tibial fixation.8–14 Morbidity has been minimal.15–18 In our experience,8 the EB has proven to be extremely reliable. After 13 years of continuous use, as well as follow-up of more than 80% of all implanted EBs, we have had no graft failures (see Chapter 69). Approximately 86% of grafts have had IKDC normal stability. We have had no hardware complications and no displaced EBs, and we have not had to remove an EB.
Surgical Technique
Femoral-Tunnel Formation
Finishing the Femoral Tunnel
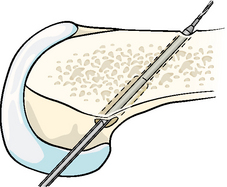
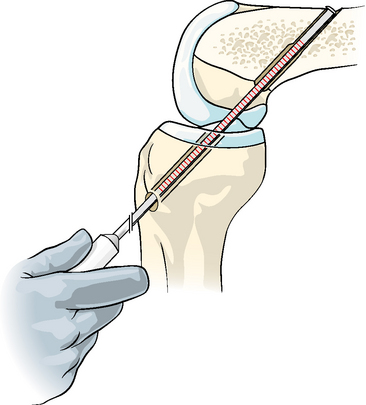
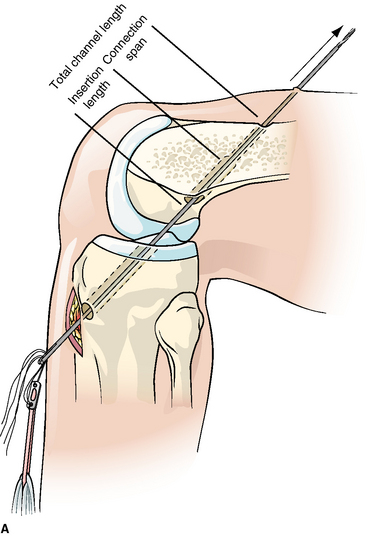
Once a satisfactory tunnel has been found, the laser pin is further drilled through the cortex. We observe the laser markings when giving way is achieved, which indicates the pin has burst through the cortex, so we have a good idea of the total channel length. Next, the appropriate acorn reamer is inserted over the pin. This is drilled nearly to the cortex, as measured from the laser pin. If high resistance is felt before the anticipated point is reached, drilling should be stopped to avoid breaking through the opposite cortex. Generally the acorn reamer will be drilled 1 to 2 mm shorter than the laser pin length indication of where the cortex was reached. The socket will usually be about 6 mm shorter than the total channel length. It must be within 9 mm of the length of the total tunnel to allow a 15-mm EB-CL to be used. This is because at least 6 mm of extra length is needed to allow a turning radius for the EB as it sits outside the femoral cortex (i.e., 6 + 9 = 15 mm). Once the socket is drilled, the acorn drill bit is withdrawn and a 4.5-mm bit is inserted and drilled through the outer cortex with the guide pin still in place (Fig. 31-1). After the 4.5-mm tunnel is drilled, the guide pin is removed with the 4.5-mm drill bit. Next, the long-depth gauge is used to measure the total channel length (Fig. 31-2). If it exceeds the socket length by more than 9 mm, the guide pin and then the acorn drill bit should be reinserted over the guide pin, and the socket should be drilled a little farther so that it is within 6 to 9 mm of the total length. If the far wall of the cortex is accidentally violated, this can be easily salvaged with an Xtendobutton, as will be described.
Preparing the Endobutton/Graft Construct
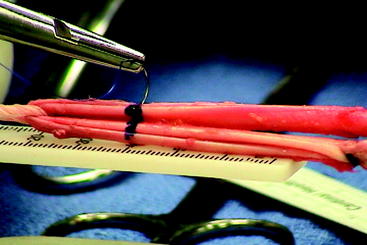
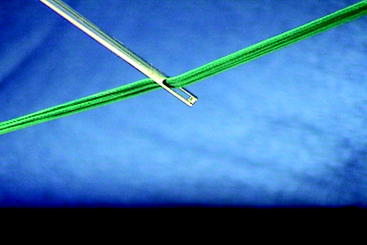
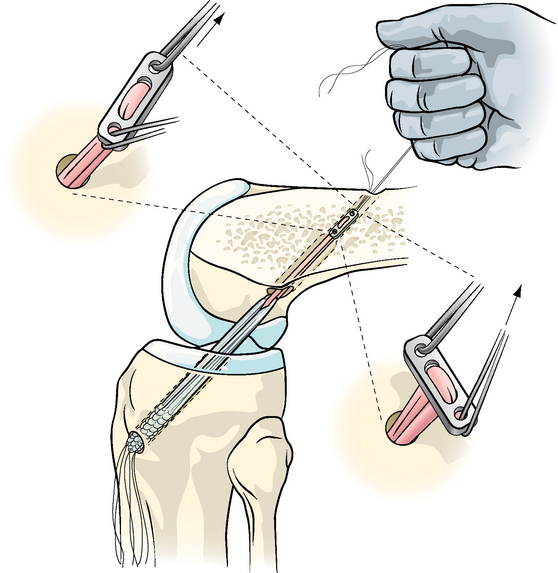
The EB-CL is positioned in the holder on the Graftmaster board. The graft is then passed through the fabric loop attached to the EB (Fig. 31-3). A violet #3–0 or 4–0 monofilament absorbable suture is then sewn across the graft (Fig. 31-4) at a distance from the EB that is 2 mm greater than the total channel length, as identified on the Graftmaster board on which the construct is positioned. In the earlier example, the total channel length was 34 mm, so the suture would be placed at 36 mm from the EB. This will provide arthroscopic evidence that the graft has been passed to the proper depth later in the procedure. This area should also be marked with a marking pin. This absorbable colored suture also locks the graft in place, preventing it from sliding on the fabric loop. A #5 suture is then passed through one eyehole and a #2 suture through the other eyehole of the EB. All four suture ends are then passed through the eye of the long passing pin (Fig. 31-5), and a hemostat is applied to the four suture ends near their tips to lock the graft onto the pin.
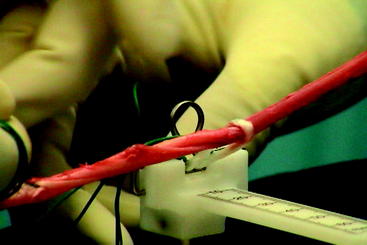
Fig. 31-3 The prepared graft is passed through the fabric loop until each arm of the graft is the same length.
Passing the Graft
The long pin with the graft and sutures attached is then passed into the tibial tunnel into the knee, where it is visualized with the arthroscope. The knee should be flexed during this passage to the same degree as when the femoral tunnel was drilled. The pin is then inserted into the femoral tunnel and passed proximalward out through a puncture in the soft tissue, where it is pulled free of the passing sutures (Fig. 31-6). Sometimes the pin must be redirected subtly within the femoral socket before it finds the smaller 4.5-mm tunnel and makes its way into the soft tissue. The two #5 sutures are then grasped with a Kocher clamp. The sutures are wound onto the closed Kocher jaws like a spool. The Kocher with wound sutures is then strongly pulled until the graft can be felt to pass into the femoral socket and become fully seated. The previously inserted violet suture and ink markings on the graft are visualized arthroscopically just outside the femoral-tunnel opening, which confirms that the graft is in proper position. If the graft is not fully seated, the Kocher can be wound like a windlass to pull in the graft. Cycling of the knee may also help.
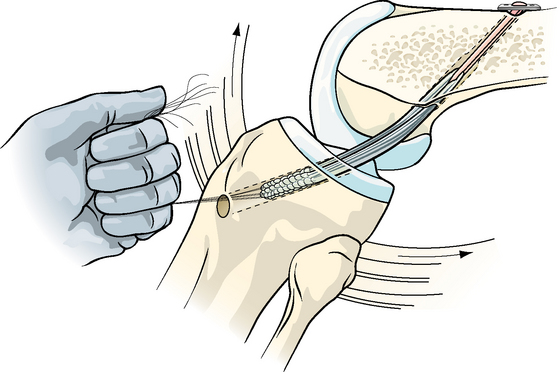
Seating the Endobutton
The two #2 sutures are then pulled to flatten the EB on the external femoral surface. After slack is taken up, a slight toggling should be felt (Fig. 31-7). Strong retrograde tension should be applied to the whipstitches as they dangle out the tibial incision while the knee is flexed and extended to make sure the graft cannot be pulled back out (Fig. 31-8). We then wrap the sutures around the smooth shank of the tibial screw and hold very strong tension while fully flexing and extending the knee three times. This serves to eliminate slack from the graft. Equally importantly, this will serve to pull the graft out of the knee if the EB has not been seated. For this reason, this step is very important. We have had the graft withdraw in this fashion two or three times and have successfully reseated it each time (see “Troubleshooting”). We have never had a graft pull out later. However, if this step had been omitted, later loosening could have occurred in these cases. The tibial screw or other tibial fixation method is then tightened.
Troubleshooting
In this section, we list all the EB problems that we have either encountered or theorized but not encountered. In all cases the difficulty was dealt with, the surgery was finished with only a minor delay, and a good result was obtained. In 13 years of continuous use we have never had an EB-related complication, EB failure, or migration. We have never had to remove an EB nor had a graft fail when fixated with an EB.8 Rarely, however, one of the following problems may arise. If the surgeon is prepared, these problems should pose no difficulty. The EB has proven to be remarkably trouble free over the most extended use of any soft tissue femoral fixation device.
Problem 1: What if the Endobutton Will not Flatten and the Graft Pulls back through and into the Knee?
Problem 2: What if the Endobutton Flattens Initially but Is Pulled Back out when the Graft is Tensioned?
Problem 3: What if the Passing Sutures cannot be Pulled out of the Endobutton After Fixation?
Problem 4: What if the Endobutton-CL Is so Long that There Is too Little Graft in the Femoral Tunnel?
Cause
Mismeasurement of the tunnel or miscalculation with selection of an EB-CL that is too long.
Remedy
Even if there were less graft in the tunnel than we had planned, we would leave it alone if there were at least 15 mm of graft in the tunnel. Studies19,20 and the experience of ourselves and others have shown this to be adequate. If less than 15 mm were in the tunnel and the fabric loop were visible through the arthroscope, we would recommend cutting the loop arthroscopically and then using the 4.5-mm bit to push the EB outward into the soft tissue. The tunnel would then be remeasured, and another EB-CL of more appropriate length would be used. If the fabric loop were not visible arthroscopically or could not be cut and if less than 15 mm of graft were in the tunnel, we would make a small second incision to either remove the EB or feed it back into the tunnel so that it could be removed from below. We would then remeasure the tunnel and use an appropriately shorter EB so that satisfactory graft remained in the tunnel.
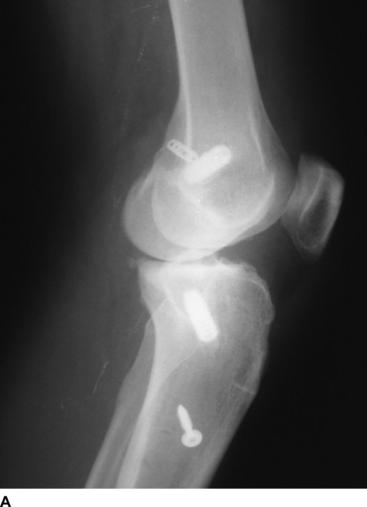
The Xtendobutton
Recently released, the Xtendobutton is a larger button that attaches to the standard EB (Fig. 31-9), effectively enlarging its profile as described earlier. It can be used routinely to eliminate the need to drill the narrower 4.5-mm tunnel. This larger profile can be used with larger tunnels up to at least a 10-mm tunnel. We still use the smaller 4.5-mm tunnel in conjunction with the larger socket because we believe the smaller bone removal may be beneficial and because we are comfortable with this technique after 13 years of continuous use. However, it is likely that the use of the Xtendobutton will prove to be just as reliable. Xtendobutton use eliminates the calculations involved with two tunnels, which may facilitate the procedure for the occasional user. As described earlier, the Xtendobutton is of great value if the surgeon penetrates out the far femoral cortex with the larger socket reamer such that the standard EB is too small to use. Before the introduction of the Xtendobutton a second incision would have had to be made over the femur for insertion of a femoral screw. The Xtendobutton allows the procedure to be completed in the usual fashion without a second femoral incision (Fig. 31-10).
Conclusions
1 Ahmad CS, Gardner TR, Groh M, et al. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:635-640.
2 Brand JJr, Weiler A, Caborn DNM, et al. Graft fixation in cruciate ligament surgery. Am J Sports Med. 2000;28:761-774.
3 Brand JJr, Hamilton D, Selby D, et al. Biomechanical comparison of quadriceps tendon fixation with patellar tendon bone plug interference fixation in cruciate ligament reconstruction. Arthroscopy. 2000;16:805-812.
4 Brown CH, Wilson DR, Hecker A, et al. Comparison of hamstring and patellar tendon femoral fixation: cyclic load. Presented at the 1999 Meeting of the American Orthopaedic Society for Sports Medicine, Traverse City, MI, June, 1999. 1999.
5 Rowden NJ, Sher D, Rogers GJ, et al. Anterior cruciate ligament graft fixation: initial comparison of patellar tendon and semitendinosus autografts in young fresh cadavers. Am J Sports Med. 1997;25:472-478.
6 Scheffler SU, Sudkamp NP, Gockenjan A, et al. Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: the impact of fixation level and fixation method under cyclic loading. Arthroscopy. 2002;18:304-315.
7 To JT, Howell SM, Hull ML. Contributions of femoral fixation methods to the stiffness of anterior cruciate ligament replacements at implantation. Arthroscopy. 1999;15:379-387.
8 Prodromos CC, Han YS, Keller BL, et al. Stability of hamstring anterior cruciate ligament reconstruction at two- to eight-year follow-up. Arthroscopy. 2005;21:138-146.
9 Gobbi A, Mahajan S, Zanazzo M, et al. Patellar tendon versus quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a prospective clinical investigation in athletes. Arthroscopy. 2003;19:592-601.
10 Gobbi A, Tuy B, Mahajan S, et al. Quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a clinical investigation in a group of athletes. Arthroscopy. 2003;19:691-699.
11 Cooley VJ, Deffner KT, Rosenberg TD. Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy. 2001;17:795-800.
12 Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564-573.
13 Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015-1025.
14 Prodromos CC, Joyce BT, Shi K, et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar-tendon graft and fixation type. Arthroscopy. 2005;21:1202-1208.
15 Karaoglu S, Halici M, Baktir A. An unidentified pitfall of Endobutton use: case report. Knee Surg Sports Traumatol Arthrosc. 2002;10:247-249.
16 Simonian PT, Behr CT, Stechschulte DJJr, et al. Potential pitfall of the Endobutton. Arthroscopy. 1998;14:66-69.
17 Muneta T, Yagishita K, Kurihara Y, et al. Intra-articular detachment of the Endobutton more than 18 months after anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:775-778.
18 Brucker P, Zelle BA, Fu FH. Intraarticular Endobutton displacement in anatomic anterior cruciate ligament double-bundle reconstruction: a case report. Op Tech Orthop. 2005;15:154-157.
19 Zantop T, Brucker P, Bell K, et al. The effect of tunnel-graft length on the primary and secondary stability in ACL reconstruction: a study in a goat model. Presented at the 2006 meeting of the European Society of Sports Traumatology, Knee Surgery, and Arthroscopy, Innsbruck, Australia, May, 2006. 2006.
20 Yamazaki S, Yasuda K, Tomita F, et al. The effect of intraosseous graft length on tendon-bone healing in anterior cruciate ligament reconstruction using flexor tendon. Knee Surg Sports Traumatol Arthrosc. 2006;14:1086-1093.