Best modality for identifying intramural/intraluminal gallbladder (GB) gas (100% sensitive)
• Ultrasound
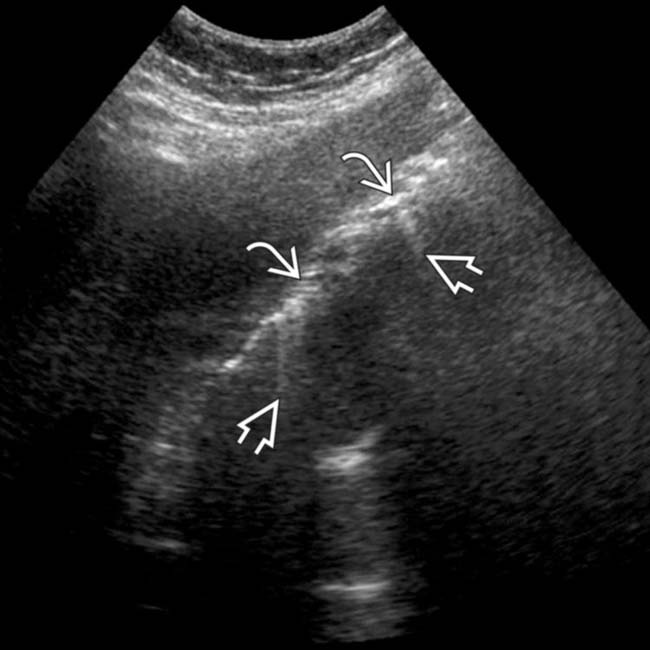
 in the gallbladder (GB) wall with “dirty” acoustic shadowing and “ring down” artifact
in the gallbladder (GB) wall with “dirty” acoustic shadowing and “ring down” artifact  , classic for emphysematous cholecystitis.
, classic for emphysematous cholecystitis.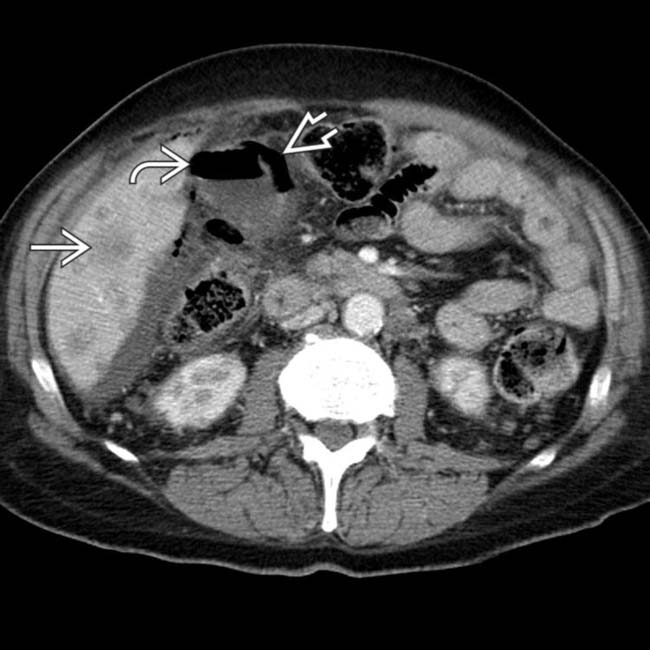
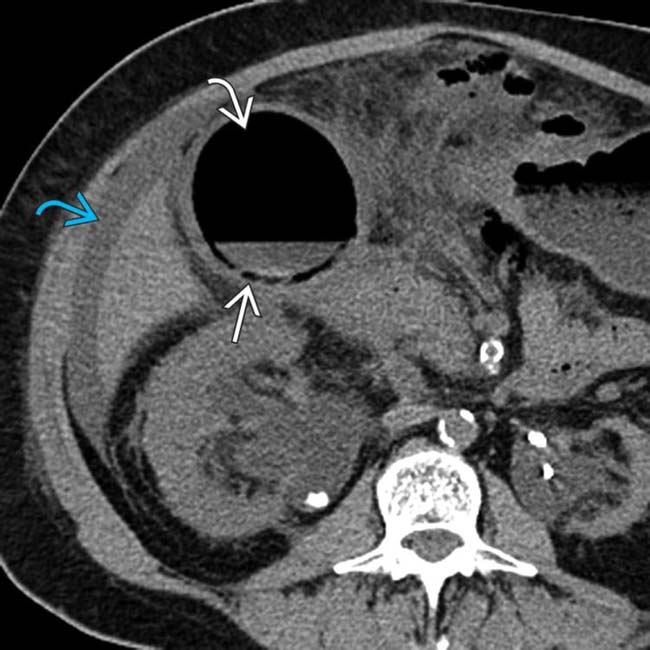
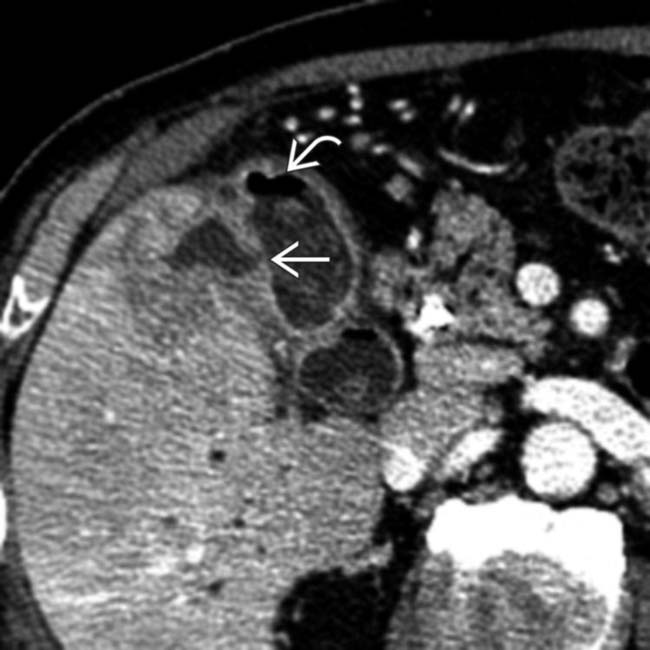
 . Gas is present within the GB lumen
. Gas is present within the GB lumen  , and the GB wall appears to be perforated
, and the GB wall appears to be perforated  . Gangrenous perforation of the GB was seen at surgery, possibly related to the patient’s chemotherapy.
. Gangrenous perforation of the GB was seen at surgery, possibly related to the patient’s chemotherapy.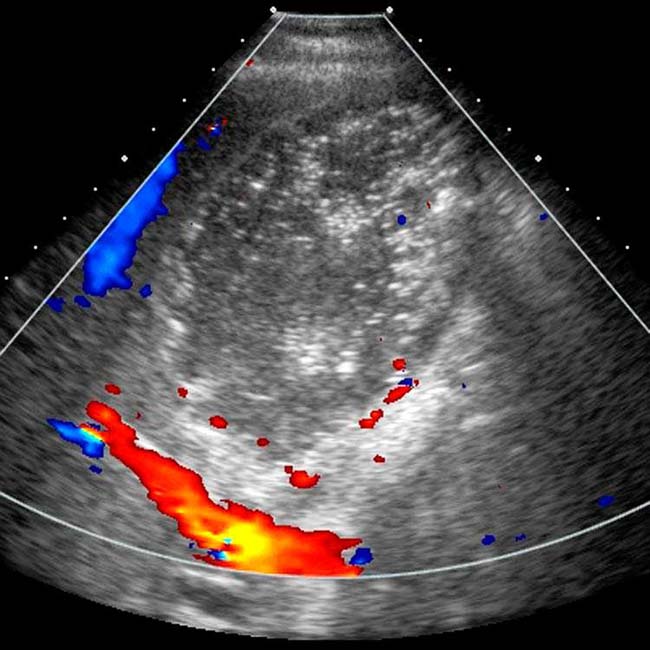
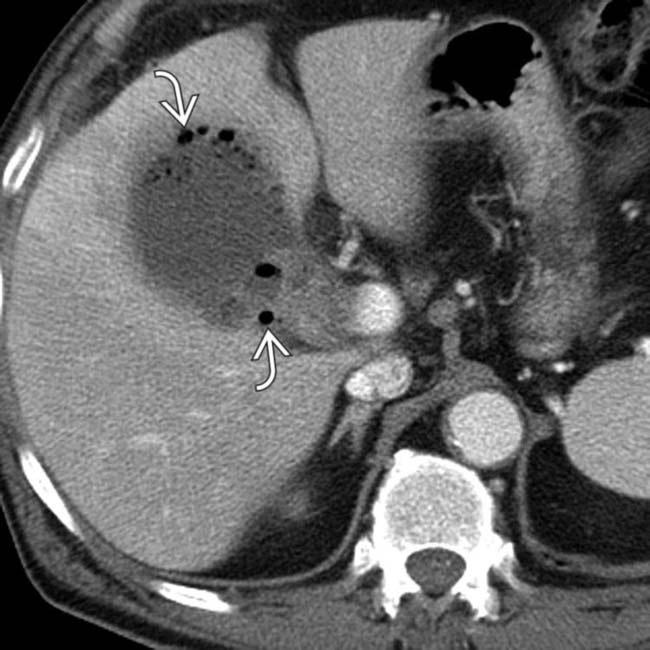
 within the wall and lumen corresponding to the echogenic foci identified on sonography, in keeping with emphysematous cholecystitis.
within the wall and lumen corresponding to the echogenic foci identified on sonography, in keeping with emphysematous cholecystitis.IMAGING
General Features
MR Findings
• Intraluminal and intramural gas appear as signal voids on all pulse sequences
Ultrasonographic Findings
• Gas in GB wall manifests as highly echogenic reflectors with dense posterior acoustic “dirty” shadowing
• Intraluminal gas bubbles should be mobile on real-time US and may rise up to nondependent portions of GB similar to bubbles of champagne (champagne sign)
DIFFERENTIAL DIAGNOSIS
Gangrenous Cholecystitis
Gas-Forming Hepatic Abscess
 and lumen
and lumen  of the GB, which has a thickened wall. Note the presence of significant surrounding fat stranding and ascites
of the GB, which has a thickened wall. Note the presence of significant surrounding fat stranding and ascites  ,
,
 , but also gas
, but also gas  extending outside the GB, in keeping with perforation. Emphysematous cholecystitis carries a high risk of both wall gangrene and perforation.
extending outside the GB, in keeping with perforation. Emphysematous cholecystitis carries a high risk of both wall gangrene and perforation.
 and nondependent linear intramural echogenicity
and nondependent linear intramural echogenicity  . Note the “dirty” posterior shadowing
. Note the “dirty” posterior shadowing  , an ultrasound artifact characteristic of gas.
, an ultrasound artifact characteristic of gas.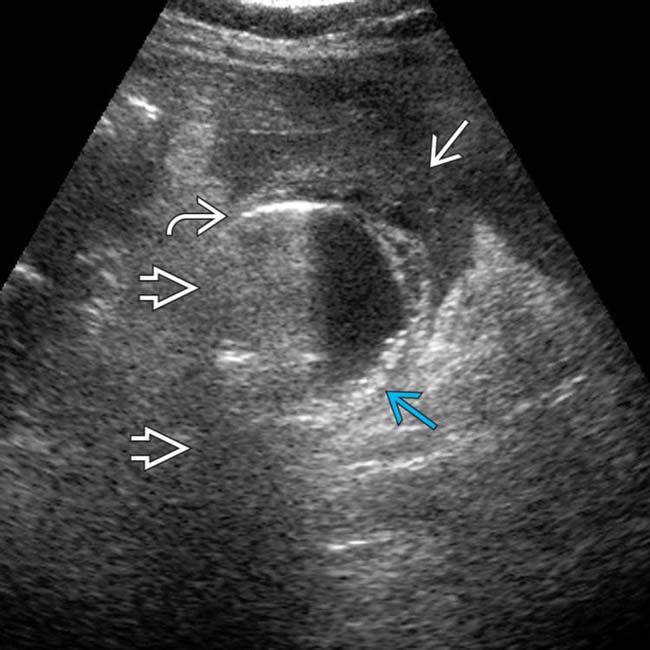
 and posterior “dirty” shadowing
and posterior “dirty” shadowing  . Note the infiltrated omentum
. Note the infiltrated omentum  adjacent to the GB and fine, layering gallstones
adjacent to the GB and fine, layering gallstones  . Gangrenous cholecystitis was confirmed at pathology.
. Gangrenous cholecystitis was confirmed at pathology.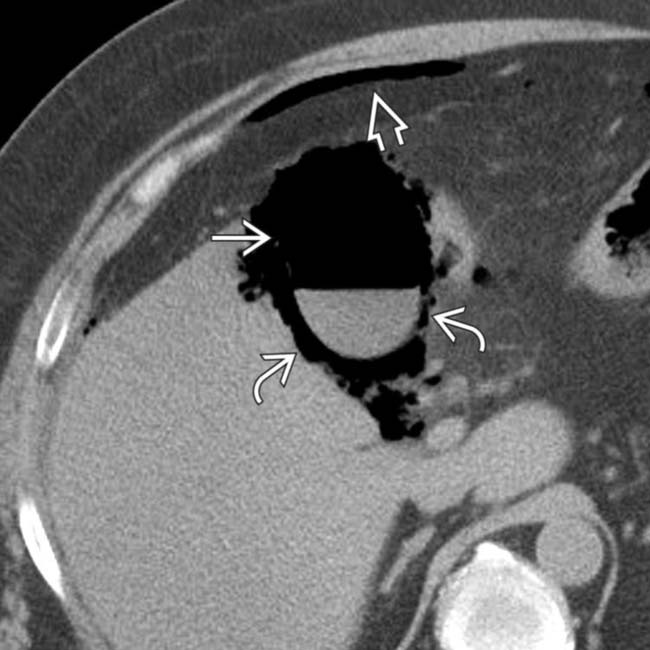
 and intramural
and intramural  GB gas. Note free intraperitoneal gas
GB gas. Note free intraperitoneal gas  , a manifestation of GB perforation. Transmural GB necrosis and gram-negative rods were shown at pathology.
, a manifestation of GB perforation. Transmural GB necrosis and gram-negative rods were shown at pathology.
 and intramural gas
and intramural gas  , characteristic findings in the setting of emphysematous cholecystitis.
, characteristic findings in the setting of emphysematous cholecystitis.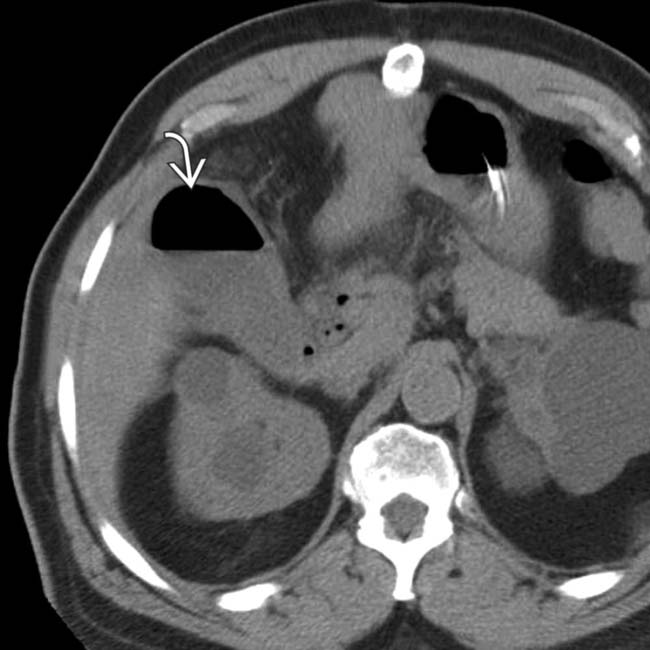
 , in keeping with emphysematous cholecystitis.
, in keeping with emphysematous cholecystitis.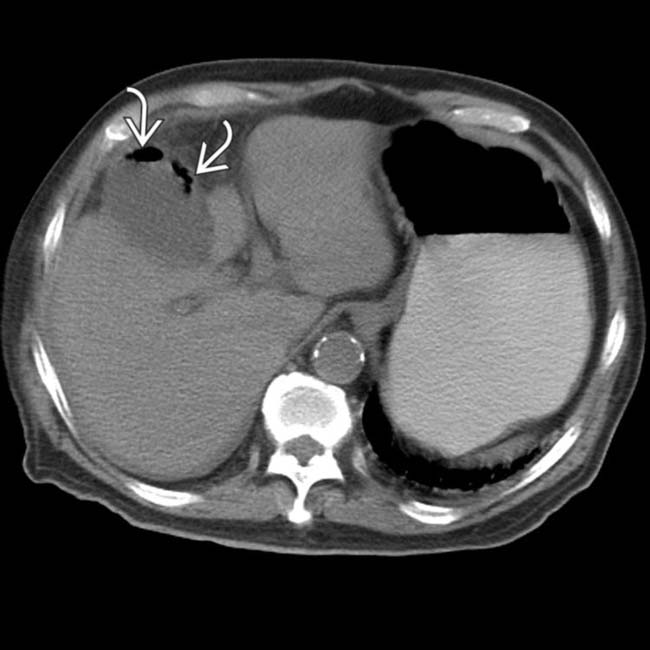
 within the wall of a distended GB, in keeping with emphysematous cholecystitis. A perforated gangrenous GB was found at surgery.
within the wall of a distended GB, in keeping with emphysematous cholecystitis. A perforated gangrenous GB was found at surgery.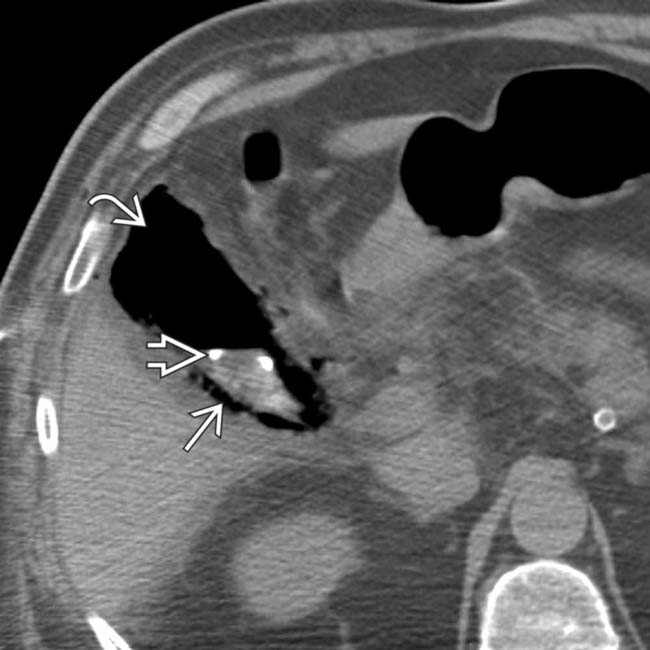
 and wall
and wall  of the GB. At the request of the referring physicians, a percutaneous pigtail catheter
of the GB. At the request of the referring physicians, a percutaneous pigtail catheter  was placed into the GB lumen with no benefit to the patient, who subsequently had an open cholecystectomy.
was placed into the GB lumen with no benefit to the patient, who subsequently had an open cholecystectomy.
 . Note peripheral portal venous gas
. Note peripheral portal venous gas  , a rare complication of emphysematous cholecystitis. The patient recovered after open cholecystectomy.
, a rare complication of emphysematous cholecystitis. The patient recovered after open cholecystectomy.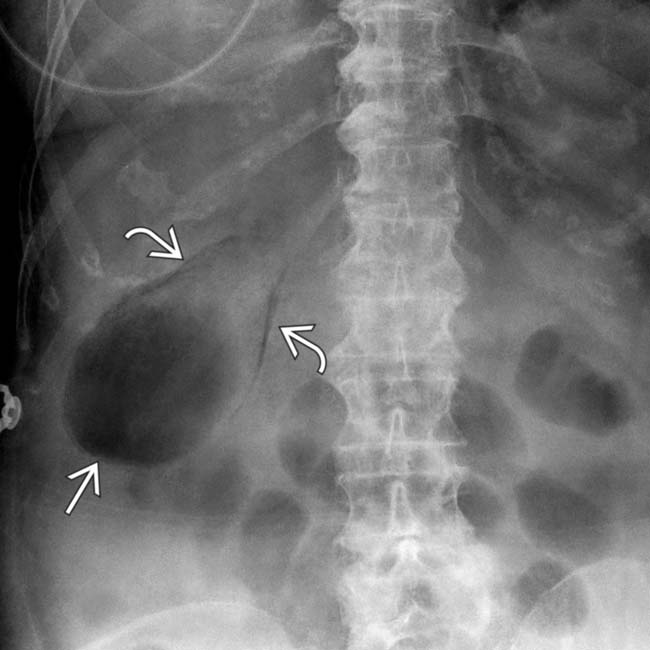
 and lumen
and lumen  of the GB.
of the GB.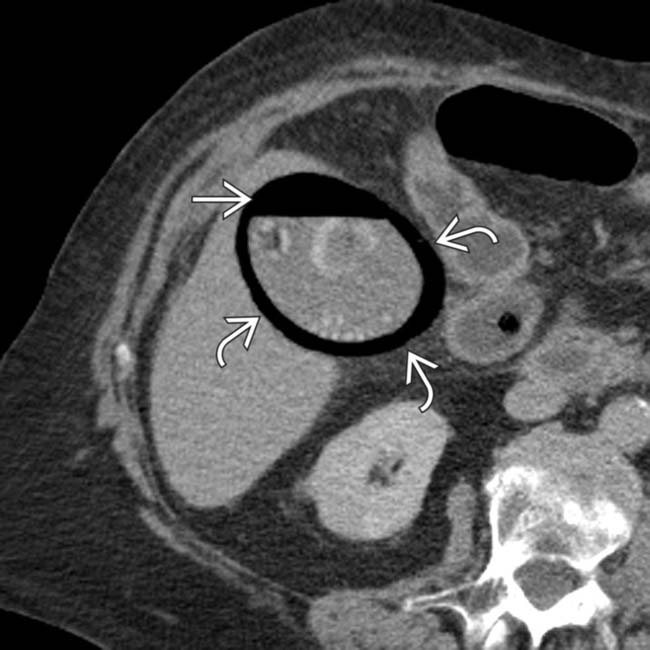
 and lumen
and lumen  of the GB.
of the GB.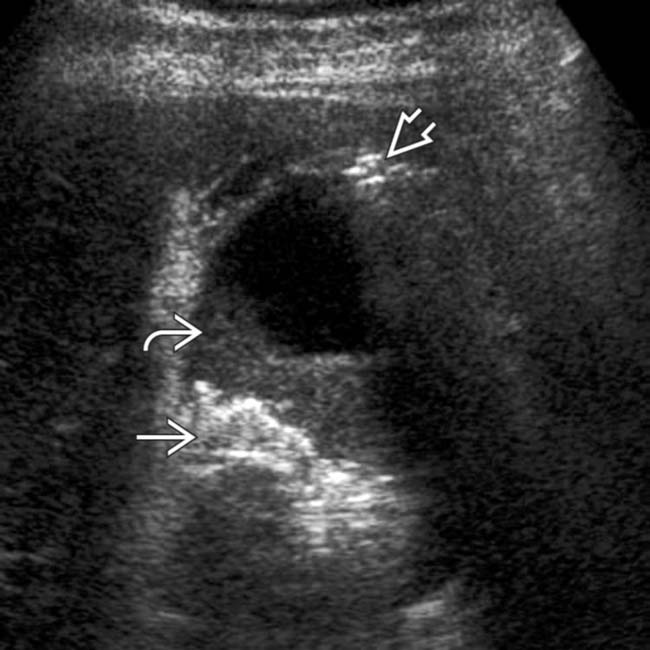
 and sludge
and sludge  in the GB, as well as intramural gas
in the GB, as well as intramural gas  , which appears as “dirty” shadowing in the fundus.
, which appears as “dirty” shadowing in the fundus.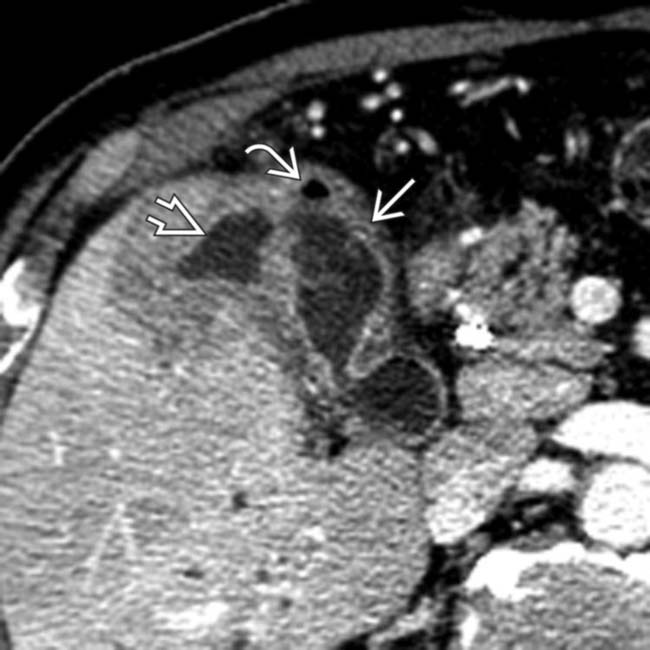
 and gas bubble
and gas bubble  in the GB wall. There is also an adjacent fluid collection
in the GB wall. There is also an adjacent fluid collection  , consistent with a pericholecystic abscess.
, consistent with a pericholecystic abscess.
































































 and gas in the GB wall
and gas in the GB wall  . GB perforation was confirmed at surgery.
. GB perforation was confirmed at surgery.
 and layering high-attenuation clot
and layering high-attenuation clot  within the GB lumen. Hemorrhagic, gangrenous cholecystitis was confirmed at laparotomy.
within the GB lumen. Hemorrhagic, gangrenous cholecystitis was confirmed at laparotomy.


