Emergency Thoracotomy for Trauma
Introduction
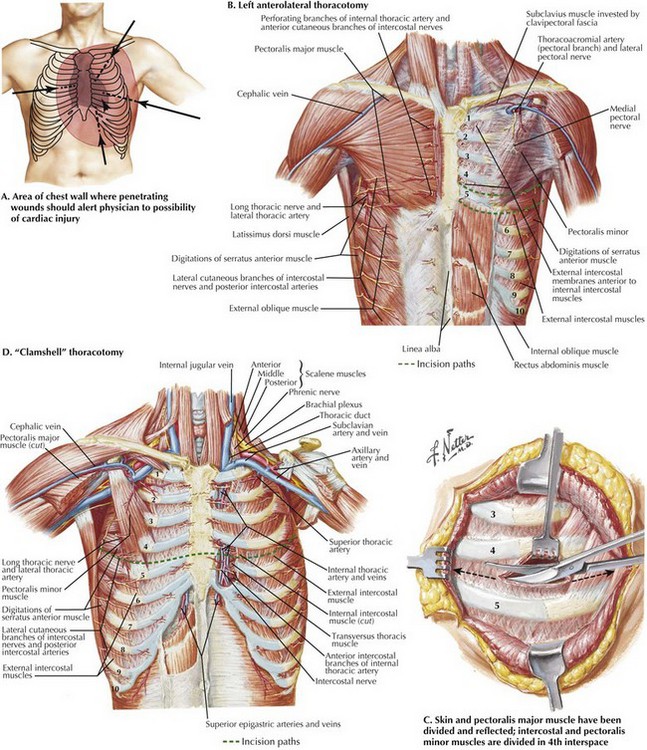
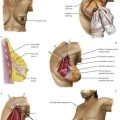
Injury to the thoracic cavity is second only to brain injury as a leading cause of trauma deaths. Most thoracic injuries are managed with nonsurgical therapies. Emergency thoracotomy is a lifesaving procedure only used in select circumstances. Knowledge of the appropriate indications for thoracotomy and thoracic anatomy are paramount. The American College of Surgeons (ACS) Committee on Trauma has summarized indications for use of thoracotomy in the ED as follows (Fig. 44-1, A):
Surgical Principles
The most expeditious entry into the thoracic cavity is through a left anterolateral thoracotomy incision performed in the 4th or 5th intercostal space (Fig. 44-1, B). This incision can be performed easily with a scalpel and then Mayo scissors, if available. A right anterolateral thoracotomy incision does not provide adequate exposure for control of most cardiac injuries but is useful for penetrating injuries to the right chest cavity.
The patient should be placed in the supine position with the arms stretched out. If time allows, a wedge should be placed under the left side of the chest, creating an approximately 15-degree tilt for better exposure. The 4th or 5th intercostal space is located just below the nipple in men and, with the breast retracted, at the inframammary fold in women. The incision should extend from the left sternal edge to the midaxillary line. The inferior portion of the pectoralis major and minor, serratus anterior, and intercostal muscles are divided (Fig. 44-1, C).
If necessary, the incision can be extended across the sternum to the right midaxillary line as a “clamshell” thoracotomy. Dividing the sternum transversely also will divide the internal mammary arteries, which can lead to troublesome bleeding if they are not ligated (Fig. 44-1, D).
Thoracotomy Technique
1. Mobilization of the left lung
2. Relief of cardiac tamponade and control of the cardiac defect
3. Performance of open cardiac massage
Control of Cardiac Injury
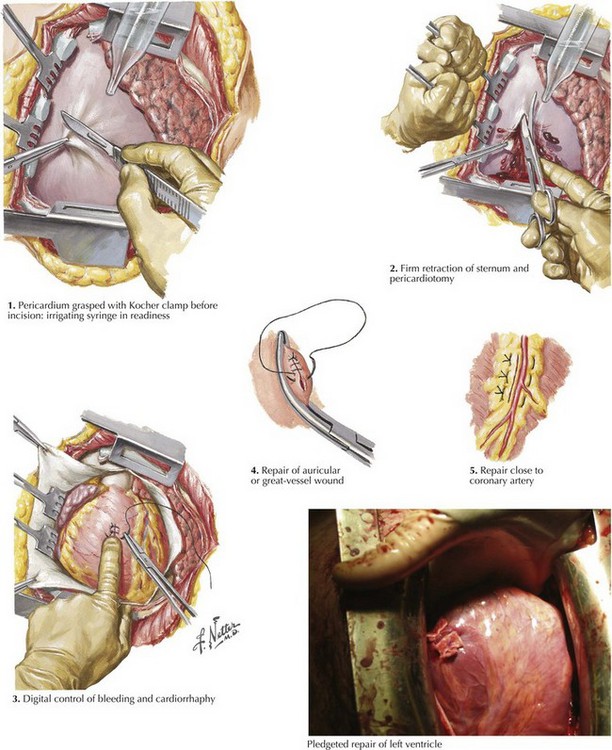
Definitive control of cardiac injury is best managed in the operating room. The thin walls of the atria should be reapproximated with atraumatic vascular clamps (i.e., Satinsky clamps), followed by closure with a running suture (Fig. 44-2). The muscular left ventricle is usually repaired with pledgeted sutures.
Cardiac Massage
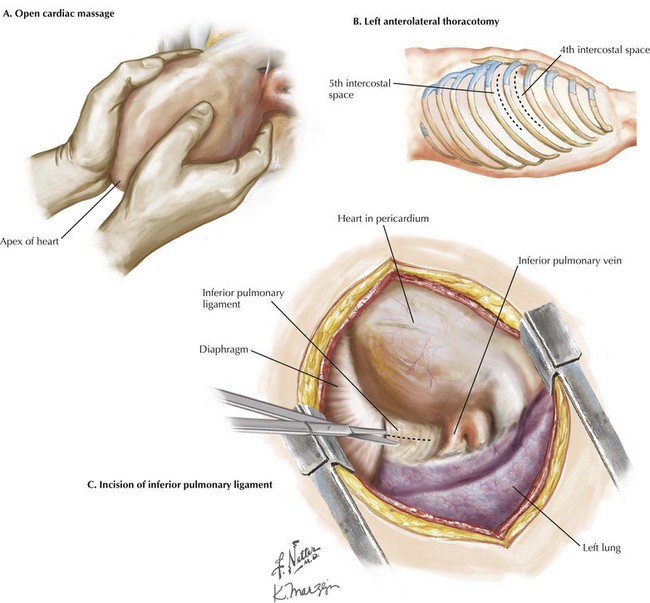
Delivery of the heart upward through the pericardial incision is helpful in performing massage. Open cardiac massage is best performed with two hands by using a hinged clasping motion with the proximal palms as the fulcrum. The heart is compressed from the apex to the base (Fig. 44-3, A).
Control of a major pulmonary or pulmonary hilar injury is facilitated by incising the inferior pulmonary ligament. Care must be taken not to lacerate the inferior pulmonary vein during this maneuver (Fig. 44-3, B).
Control at Hilum and Injury Repair
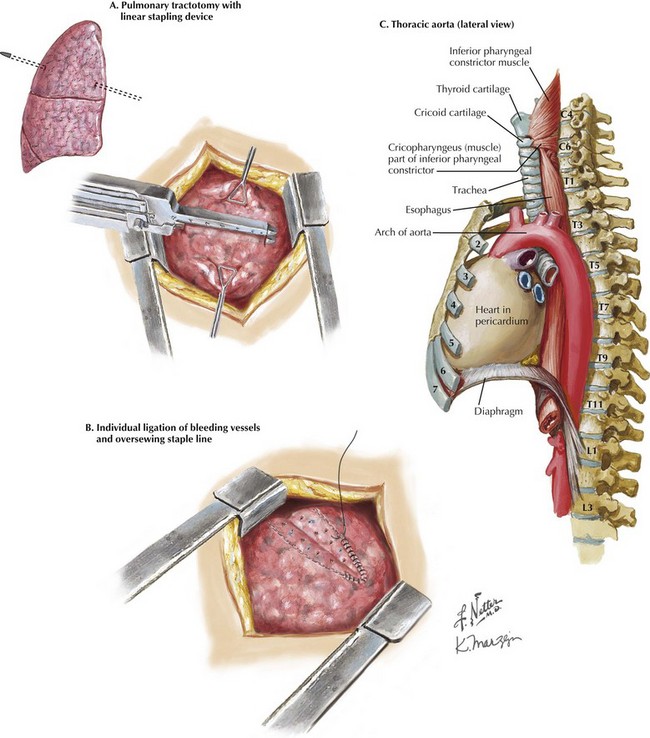
Pulmonary injuries are best treated by nonanatomic resection, direct suture repair, or pulmonary tractotomy. Pulmonary tractotomy is especially suitable for through-and-through injuries. The injury tract is opened with a linear stapling device or between clamps (Fig. 44-4, A). Bleeding vessels are then oversewn within the tract (Fig. 44-4, B).
Aortic Clamping
Placement of a nasogastric or orogastric tube can facilitate identification of the aorta (Fig. 44-4, C). The mediastinal pleura is opened anteriorly and the parietal pleura posteriorly by using either blunt or sharp dissection. A cross-clamp is then placed. The aorta is not completely encircled because injury to the intercostal vessels may occur. The aortic cross-clamp should be removed as soon as practical to prevent ongoing cardiac strain and visceral ischemia.
American College of Surgeons. Practice management guidelines for emergency department thoracotomy. Committee on Trauma Working Group, Ad Hoc Subcommittee on Outcomes. J Am Coll Surg. 2001;193:303–309.
Cothren, CC, Moore, EE. Emergency department thoracotomy for the critically injured patient: objectives, indications, and outcomes. World J Emerg Surg. 2006;24:1–4.
Hunt, PA, Greaves, I, Owens, WA. Emergency thoracotomy in thoracic trauma: a review. Injury. 2006;37:1–19.
Morgan, BS, Jordan, JP. Emergency thoracotomy: the indications, contraindications and evidence. J Army Med Corps. 2009;155:87–93.