Emergency Sports Assessment
This chapter will enable the health care professional to immediately assess a patient before applying first aid or transportation to the hospital. This assessment should be divided into two parts. The first part concerns the primary evaluation or survey, which usually takes place at the location in which the patient is found to ensure that life-threatening situations are handled immediately. The second part of the assessment is performed when the examiner has more time and the patient is not under immediate threat of death or permanent disability.
Pre-Event Preparation
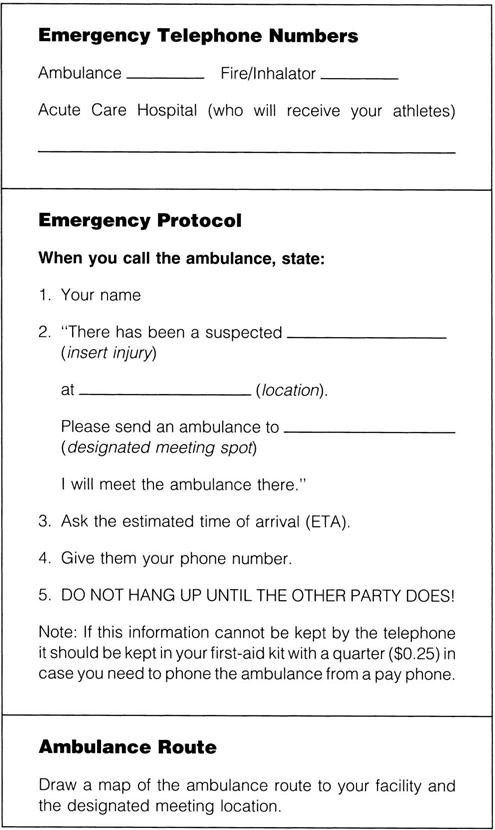
Before any sporting event, the examiner should establish and practice emergency protocols and review sideline preparedness.1–3 This preparation includes designating personnel for specific tasks and establishing emergency vehicle routes and entrances. The examiner and the assistants should know the location of additional medical assistance, emergency equipment (e.g., spinal board, neck supports, sandbags, stretchers, blankets, emergency first-aid kit), and a telephone. The equipment must be compatible with the needs, size, and age of the athletes, and with the equipment of other health care professionals. Near the telephone, the examiner should post emergency telephone numbers (e.g., ambulance, physician, dentist), identify the name and address of the sports facility, specify the entrance to be used, and note any obvious landmarks, because the person making the emergency call may forget information or give inappropriate information when under stress (Figure 18-1). Included in the preparation is a communication plan for on-field or at-site injuries. This plan may involve pre-established hand signals (e.g., crossed arms may mean “send a physician out,” whereas a hand on top of one’s head may signify “send ambulance or emergency medical services [EMS] personnel”) or walkie-talkies to communicate with other professionals working on the sideline.4
The examiner should take the time to give the facility a safety check by looking for potential hazards. Visiting teams should also be informed of emergency protocols. In addition, emergency situations and protocols must be practiced repeatedly to ensure that proper care will be given in an emergency.
Primary Assessment
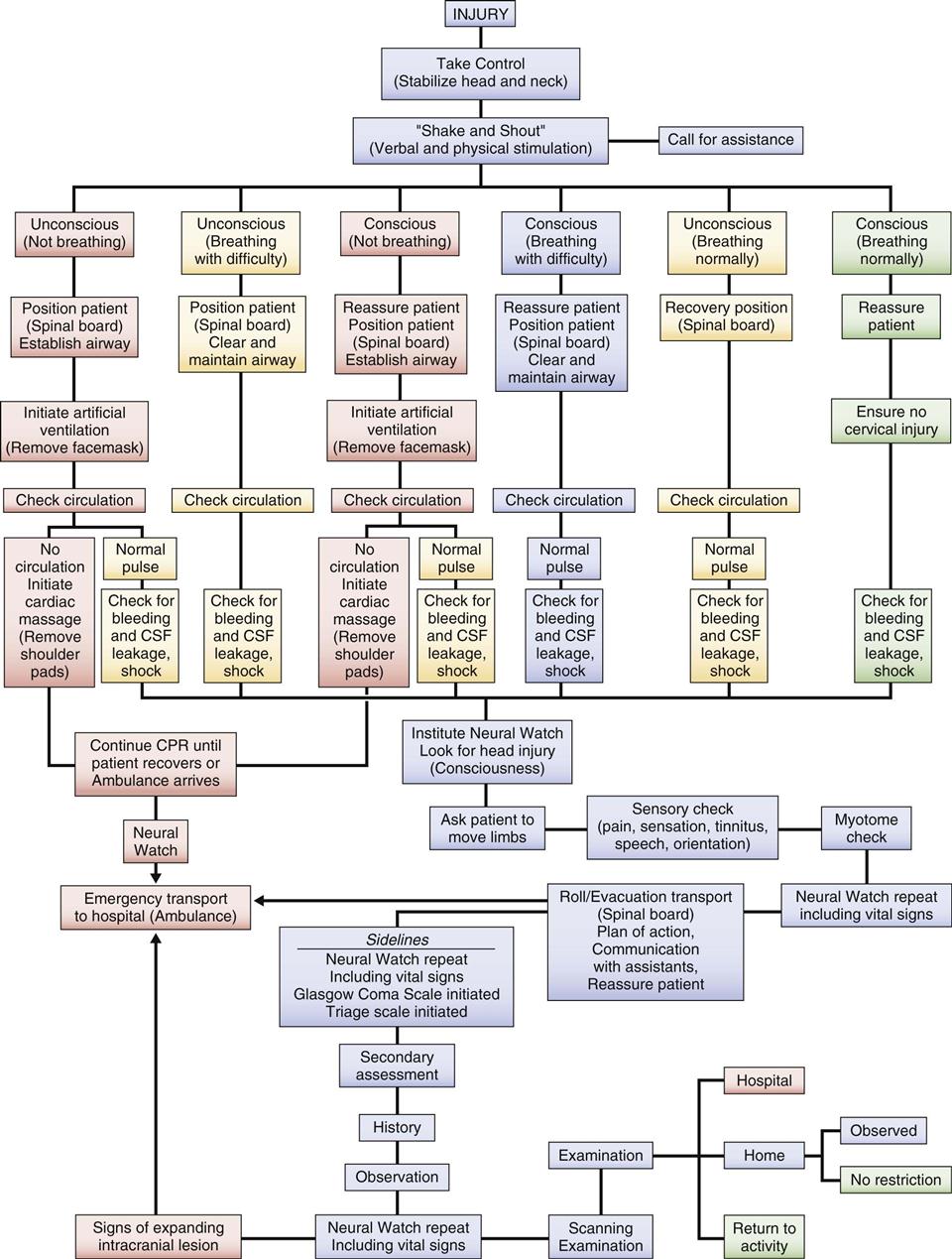
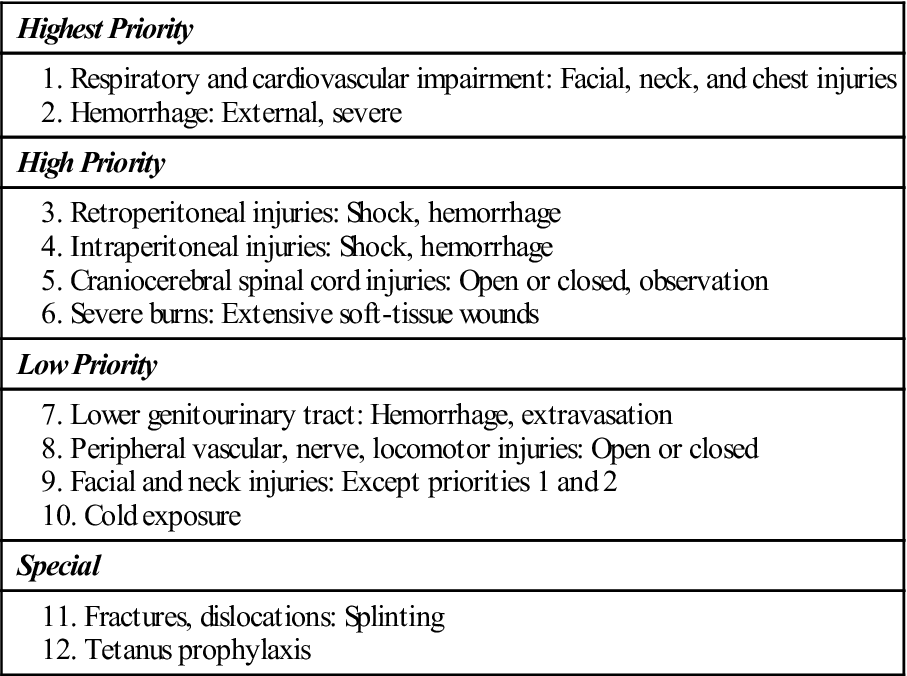
After an injury occurs, the examiner must first take control of the situation and ensure that no additional harm comes to the patient. The primary survey, which takes 30 seconds to 2 minutes with the maximum on-scene time being 10 minutes, is carried out with little or no movement of the patient.5 It is used to determine whether injuries are life threatening, the severity of injury, and how the patient can be moved. With severe injuries, the longer the assessment takes, the higher the mortality rate is likely to be. If, at any time, the examiner finds that a major injury has occurred (Table 18-1), he or she may terminate the assessment process and ensure the patient receives higher levels of care by calling for the ambulance or EMS. The examiner is designated as the charge person, or person in control. The examiner takes control by not allowing the patient to be moved until some type of assessment is made, the spine is supported as much as possible, and, if required, assistance is obtained.
TABLE 18-1
Priorities in the Management of Injuries: Beware of Injury to the Cervical Spine!
From Steichen FM: The emergency management of the severely injured. J Trauma 12:787, 1972.
For the primary emergency assessment, the examiner should call at least one person to provide immediate assistance, relay messages, and obtain additional help, if necessary. This person is designated the call person, and he or she should know the location of the closest telephone (a cell phone would be ideal) and what telephone numbers to call in specific emergencies. This information can be posted on or by the telephone (see Figure 18-1). When telephoning, the call person should state the caller’s name, the number of the telephone being used, the exact emergency (type of injury), the degree of urgency, and the exact location of the facility; ask for an estimated time of arrival; and explain the location of the best entrance to the facility for responding emergency personnel. Other individuals (as many as six or seven) may be called as necessary to act as transporters or help move the patient.
While performing the initial assessment, the examiner must keep in mind that six situations can immediately threaten the life of a patient: airway obstruction, respiratory failure, cardiac arrest, severe heat injury, head (craniocerebral) injury, and cervical spine injury.6 It is for these situations, along with severe bleeding, that the examiner must be most prepared, because they are the most common emergency life-threatening situations. Only practice can ensure proper care in an emergency.
Initially, the examiner stabilizes and immobilizes the patient’s head and cervical spine in case the patient has suffered a cervical spine injury (Figure 18-2).7 If the patient has suffered trauma above the clavicles, he or she should be considered to have suffered a spinal injury to the cervical spine until proven otherwise.8 Simultaneously, the examiner talks to the patient. If the patient replies in a normal voice and gives logical answers to questions, the examiner can assume that the airway is patent and the brain is receiving adequate perfusion. The examiner asks the patient what happened to determine how the injury occurred (mechanism of injury). The patient is asked to describe the symptoms (e.g., pain, numbness) and how severe he or she thinks the injury is. The examiner then explains what he or she is going to do and reassures the patient.9 If the patient is unable to speak or is unconscious, the examiner must ask witnesses what happened. If the patient is unconscious (“collapsed athlete”), the examiner must work with the assumption that a neck (cervical spine) injury has occurred until proven otherwise.10
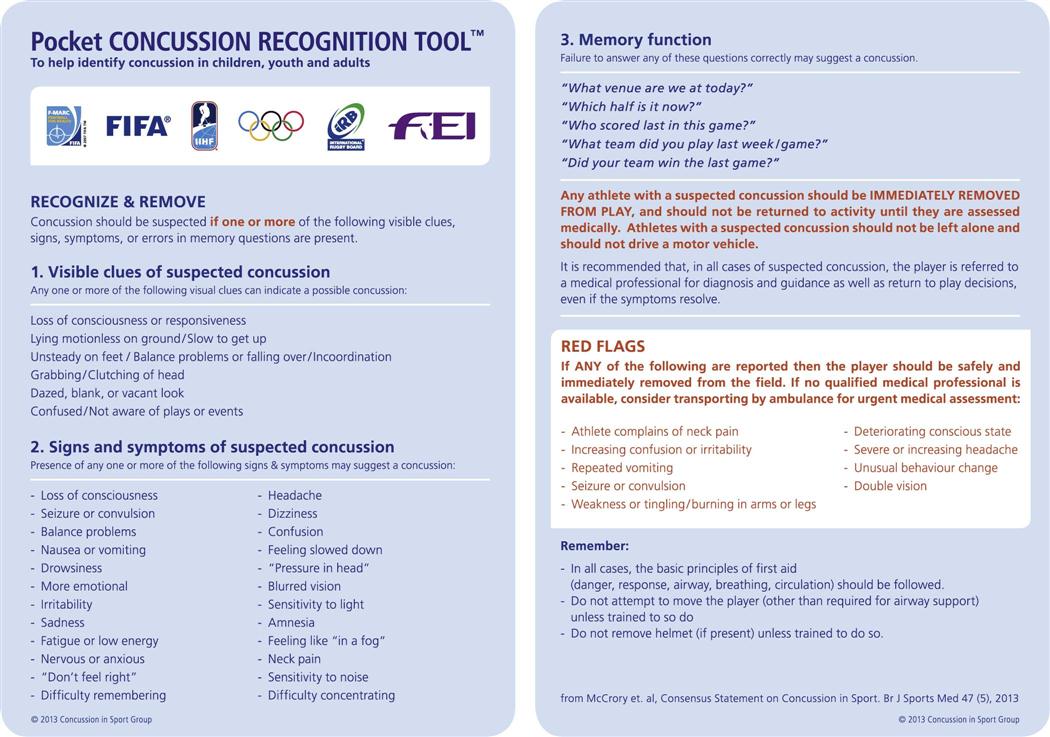
While the examiner is talking to the patient, he or she should be observing whether the patient moves, is still, or is having a seizure. If the patient moves, it means he or she is at least partially conscious, has no apparent neurological dysfunction, and has some cardiopulmonary function. If the patient is still, it means he or she is unconscious, has some neurological dysfunction, or has some other major system failure. A seizure indicates neurological, systemic, or psychological dysfunction. The examiner should also observe the position of the patient (e.g., normal, deformity) and look for altered joint alignment (e.g., fracture, dislocation), swelling, or discoloration.4 In case there is a spinal cord injury, the patient should be left in the original position until the nature and severity of the injury have been determined, except in cases of respiratory or cardiac distress. If the athlete is suspected of having a head injury and is mobile, the examiner can use a Pocket Concussion Recognition Tool™ (Figure 18-3) on the sideline to determine if a concussion has occurred.11 A rapid assessment of the brain and spinal cord can be accomplished by asking the patient to do simple movements, such as sticking out the tongue12 (see the “Assessment for Spinal Cord Injury” section, presented later). If a concussion is suspected, the procedures in the following box should be followed.13
Level of Consciousness
The examiner must quickly determine whether the patient is conscious. At no time during the initial assessment should ammonia inhalants be used to arouse the patient. Inhalants should be used only after the examiner is absolutely sure there is no spinal injury, because the fumes may cause a reflex head jerk, complicating the possible neck injury.8 At this early stage, the examiner simply determines whether the patient is alert (fully conscious), confused (drowsy), in delirium, in obtundation (dulled sensations, especially pain and touch), in a stupor, or in a coma. A patient is classified as alert if he or she is able to carry on an appropriate conversation with no delays and is aware of time, place, and identity. See Chapter 2 for an explanation of the levels of consciousness.
The examiner determines the level of consciousness or arousal by talking to the patient, not by moving the patient. This stage is sometimes referred to as the “shake and shout” stage, in which the examiner tries to arouse the unconscious individual by gentle shaking (without allowing movement of the head and neck) and by shouting into each ear. If the patient does not respond to this verbal stimulus, the examiner can, at least initially, assume that the patient is unconscious or not fully conscious and proceed under that assumption. Further neurological assessment is left until the examiner is sure that the patient has a patent airway, is breathing normally, and has a heartbeat. If the patient is conscious, the examiner should reassure the patient that help has arrived. The patient should be informed of what the examiner is doing and proposes to do in terms of examining and moving the patient. Regardless of the patient’s state of consciousness, he or she should not move or be moved until the examination has been completed.
On the sideline, the examiner can perform a Sideline Concussion Assessment Tool—3rd edition (SCAT3) exam (see Chapter 2) and begin a Neural Watch to provide serial monitoring (see later discussion) for the possibility of an increasingly severe head injury (i.e., progressive deterioration of signs and symptoms). In addition, balance testing may be performed using the Balance Error Scoring System (BESS).14 This is a quantifiable low technology test that uses only a stopwatch and a piece of medium density foam. The athlete is asked to do three different stances (double, single and tandem) twice on two different surfaces (the ground and the foam) (see Figure 2-37) for a total of six trials. The athlete begins in the required stance with the hands on the iliac crests and, while standing quiet and motionless, is asked to close both eyes for 20 seconds. During the single leg stance, the athlete stands on the non-dominant foot and is asked to hold the opposite non–weight-bearing limb in 20o to 30o of hip flexion and 40o to 50o of knee flexion. For tandem stance, the non-dominant foot is placed behind the dominant foot. If the athlete is losing his or her balance, he or she can make any necessary adjustments and returns to the test position as quickly as possible. The athlete is scored by adding one error point for each committed error (see Table 2-22). If the athlete cannot maintain the desired stance for at least 5 seconds of the 20 second test period, the athlete has failed the test. The maximum error score for normal athletes is 10.
Establishing the Airway
While waiting for assistance, the examiner can immediately begin to check for abnormal or arrested breathing, abnormal or arrested pulse, internal and external bleeding, and shock. This initial assessment is called the airway, breathing, and circulation (ABCs) of cardiopulmonary resuscitation (CPR). New guidelines also include the use of automated defibrillators if required.15 The first priority is to maintain an adequate airway, normal ventilation, and hemodynamic stability (see Table 18-1).16,17 Also, obvious bleeding should be controlled by compression.
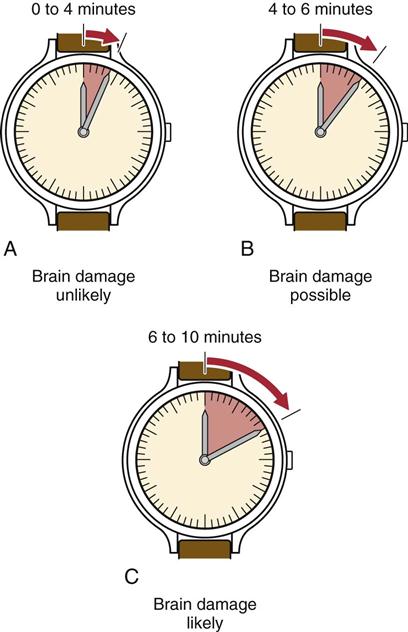
While the cervical spine is protected and immobilized, the examiner quickly assesses the airway for patency by looking, listening, and feeling for spontaneous respirations.5,8 Respirations can be determined by watching for movement of the chest, feeling the breath on the examiner’s cheek, or hearing the air move in and out (Figure 18-4). The normal resting ranges of respirations are 10 to 25 breaths per minute for adults and 20 to 25 breaths per minute for children. An athlete or someone who has been exerting before injury may show a higher rate. If a patient is not breathing and has no heartbeat, clinical death occurs between 0 and 4 minutes (Figure 18-5). If breathing and heartbeat are not restored within 4 to 6 minutes, brain damage is probable. If there is no breathing and no heartbeat for 6 to 10 minutes, biological death occurs, and brain damage is likely.18
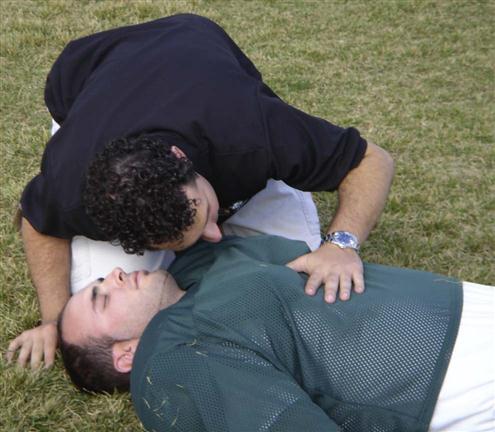
The examiner can feel the breath on the cheek, hear the breath, and watch the chest move.
If the patient is breathing without difficulty, the rate and rhythm of the respirations and their characteristics should be noted. Cheyne-Stokes and ataxic respirations are often associated with head injuries.19 Table 18-2 indicates some of the abnormal breathing patterns that may occur in a patient in an emergency situation.
TABLE 18-2
| Term | Description | Location of Possible Neurological Lesions |
| Hyperpnea | Abnormal increase in the depth and rate of the respiratory movements | |
| Apnea | Periods of non-breathing | Pons |
| Ataxic breathing (Biot respiration) | Irregular breathing pattern, with deep and shallow breaths occurring randomly | Medulla |
| Hyperventilation | Prolonged, rapid hyperpnea, resulting in decreased carbon dioxide blood levels | Midbrain, pons |
| Cheyne-Stokes respirations | Periods of hyperpnea regularly alternating with periods of apnea, characterized by regular acceleration and deceleration in depth | Cerebrum, cerebellum, midbrain, pons |
| Cluster breathing | Breaths follow each other in disorderly sequence with irregular pauses between them | Pons, medulla |
Adapted from Hickey JV: The clinical practice of neurological and neurosurgical nursing, Philadelphia, 1986, JB Lippincott, p. 138.
If the conscious patient exhibits abnormal or arrested breathing (asphyxia), the examiner should look for possible causes.20 Causes include compression of the trachea; tongue falling back, blocking the airway; foreign bodies (e.g., mouthguard, gum, chewing tobacco); swelling of the tissues (e.g., anaphylactic shock after a bee sting); fluid in the air passages; presence of harmful gases or fumes; pulmonary and chest wall trauma; and suffocation.20,21
Falling back of the tongue is the most common cause of airway obstruction after a sport injury, especially in the unconscious patient. Normally, the tone of the tongue muscles ensures airway patency. However, the unconscious person, especially one in the supine position, loses muscle tone and the tongue falls back, potentially leading to an obstruction. If the tongue is the cause of obstruction, the examiner can simply pull the chin forward in a chin lift or jaw thrust maneuver to restore the airway, being careful to keep movement of the cervical spine to a minimum. The chin lift maneuver is less likely to compromise the cervical spine.22,23 Either maneuver pulls the retropharyngeal musculature forward, thus opening the airway.20
If the examiner can see an object obstructing the airway, an oral screw and tongue forceps can be used to remove the object. The mouth should be held open with the oral screw or something similar, and the examiner can use a finger to sweep the mouth clear of debris (e.g., broken teeth, dentures, mouthguard, chewing gum, tobacco). If the jaw is not held open and blocked from closing, the examiner should put fingers in the patient’s mouth only with caution. If the cause of the blockage is something other than the tongue (e.g., foreign body), the patient, if conscious, should be asked to cough. If this does not expel the object, the Heimlich maneuver should be performed until the patient expels the object. If the patient loses consciousness, he or she should be placed supine and ventilation attempted. If it is unsuccessful, six to ten subdiaphragmatic abdominal thrusts are applied. This sequence of ventilation and subdiaphragmatic abdominal thrusts is repeated until a physician or EMS personnel arrive to perform a laryngoscopy.24 Other causes of asphyxia may be treated by epinephrine (anaphylaxis) or intubation.24 If the examiner is concerned about maintaining a patent airway, an oropharyngeal airway may be used. As a last resort, a wide-bore needle (18-gauge or larger) may be inserted into the trachea to ensure an airway.20
If the patient is not breathing, artificial ventilation (mouth-to-mouth resuscitation) must be initiated immediately, by using the breathing portion of the CPR techniques or by using a similar artificial breathing method.
If the patient is conscious but obviously in respiratory or cardiac distress, the examiner must deal with the presenting situation immediately (Table 18-3). If the patient does not have a patent airway, an airway must be established, as has been described. If the patient is moving in an attempt to get air into the lungs, the examiner may assume that a severe cervical injury is less likely to have occurred. However, movement of the head in relation to the cervical spine should be kept to a minimum. Keeping in mind the possibility of a cervical injury, the examiner should position the patient so that airway clearance and resuscitation can easily be accomplished. This change in position must be performed carefully to ensure that movement of the cervical spine is kept to a minimum. If the patient is reasonably comfortable in the side-lying or prone position and there is no problem with cardiac function or breathing, it is not necessary to move the patient to the supine position.
TABLE 18-3
| Conscious Athlete | Unconscious Athlete |
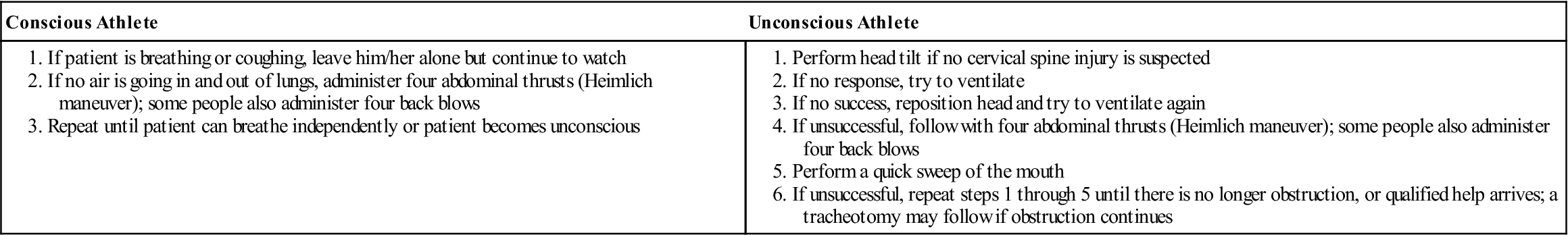
Adapted from American Academy of Orthopaedic Surgeons: Athletic training and sports medicine, Park Ridge, IL, 1984, AAOS, p. 454.
After the airway has been established, whether by the use of an airway device, by proper head or jaw positioning, by the use of tongue forceps, or by a tracheotomy, the examiner must ensure that the airway is maintained and that the patient continues breathing. If respiration is not spontaneous, assisted ventilation (e.g., mouth-to-mouth, bagging) should be instituted. Ventilation can be compromised by a flail chest or pneumothorax (tension or open).8,21 Endotracheal intubation is necessary if nasopharangeal bleeding, laryngeal trauma, secretions, or aspirations prevent maintenance of an adequate airway or end-ventilation.16,20,25 Transtracheal ventilation is the treatment of choice for patients with breathing problems caused by brain, cervical spine, or maxillofacial injuries. An endotracheal tube may cause straining and venous hypertension, leading to increased brain edema, and extension of the head and neck to open upper airways may aggravate cervical spine injuries. Also, hemorrhage in maxillofacial injuries prevents the effective use of a breathing mask and does not allow adequate visualization.17
Establishing Circulation
While the examiner is determining whether breathing is normal, the patient’s circulation should be checked for 10 or 15 seconds using the carotid (preferred), brachial, radial, or femoral pulse (Figure 18-6). For a sedentary adult, the normal heart rate is 60 to 90 beats per minute. For children, the rate is 80 to 100 beats per minute. In the highly trained athlete of either sex, the rate may be as low as 40 beats per minute. With activity, the heart rate will be above these levels, and the examiner should take this fact into account when taking the pulse. Depending on the type and level of the individual’s activity, the heart rate for a fit person should decrease to slightly above normal values within 5 minutes. The examiner should note whether the pulse is absent, rapid and rebounding, or weak and diminishing.
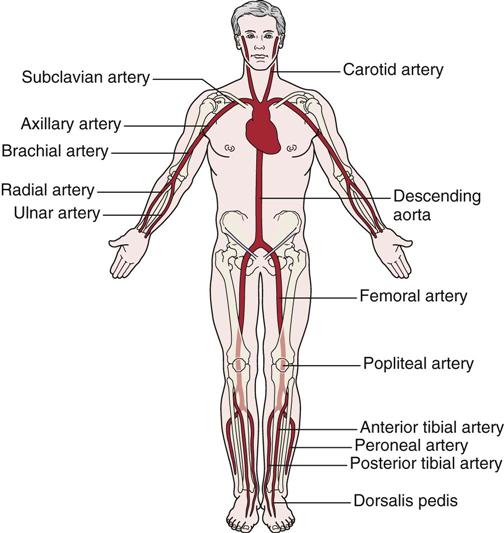
Pressure applied to any of the arteries (pressure points) can decrease bleeding if applied proximal to the bleeding.
The pulse is most often checked at the carotid artery, because this artery is large and easy to locate. Therefore, the examiner has less chance of missing the pulse and does not have to move from the area of the patient’s head to perform palpation. If a pulse cannot be detected, it should be assumed that the patient does not have a heartbeat, and CPR should be initiated using either manual methods or an automated external defibrillator. The use of the defibrillator increases the chance of survival in cardiac arrest.26 Although cardiac arrest is rare in athletes, sudden death or commotio cordis resulting from low-impact blunt trauma is always a possibility in sports.27 When the pulse is assessed, the examiner should estimate its rate, strength, and rhythm to obtain an indication of the cardiac output. Circulatory sufficiency may also be determined by squeezing the nail bed or hypothenar eminence. Capillary refill is delayed if the pink color does not return to the nail bed or hypothenar eminence within 2 seconds after release of the pressure.28 Squeezing the hypothenar eminence is a better indicator if the patient is hypothermic.
The pulse may also be used to determine the patient’s blood pressure. If a carotid pulse can be palpated, systolic blood pressure is 60 mm Hg or higher. If the femoral pulse is palpable, systolic blood pressure is 70 mm Hg or higher. If the radial pulse can be palpated, the systolic blood pressure is 80 mm Hg or higher.12,19,28 Like heart rate, blood pressure should drop to almost normal levels within 5 minutes following termination of exercise.
A weak or rapid pulse usually indicates shock, heat exhaustion, hypoglycemia, fainting, or hyperventilation. A slowing pulse is sometimes seen when there is a large increase in intracranial pressure, which usually indicates a severe lower brain stem compression.29 A pulse that is rebounding and rapid is often the result of hypertension, fright, heat stroke, or hyperglycemia.
If the pulse rate is beginning to weaken, the patient may be going into shock (Figure 18-7). Shock is characterized by signs and symptoms that occur when the cardiac output is insufficient to fill the arterial tree and the blood is under insufficient pressure to provide organs and tissues with adequate blood flow. It should be noted, however, that patients who maintain pink skin, especially in the face and extremities, are seldom hypovolemic after injury. If the skin of the face or extremities turns ash-gray or white, this usually indicates blood loss of at least 30%.8 Common types of shock and their causes are shown in Table 18-4. A patient going into shock becomes restless and anxious. The pulse slowly becomes weak and rapid, and the skin becomes cold and wet, often clammy. Sweating may be profuse, and the face is initially pale and later cyanotic (blue) around the mouth. Respirations may be shallow, labored, rapid, or possibly irregular and gasping, especially if a chest injury has occurred. The eyes usually become dull and lusterless, and the pupils become increasingly dilated. The patient may complain of thirst and feel nauseated or vomit. If shock develops quickly, the patient may lose consciousness. To prevent or delay the onset of shock, the examiner may cover the patient, elevate the patient’s legs, or attempt to eliminate the cause of the problem.
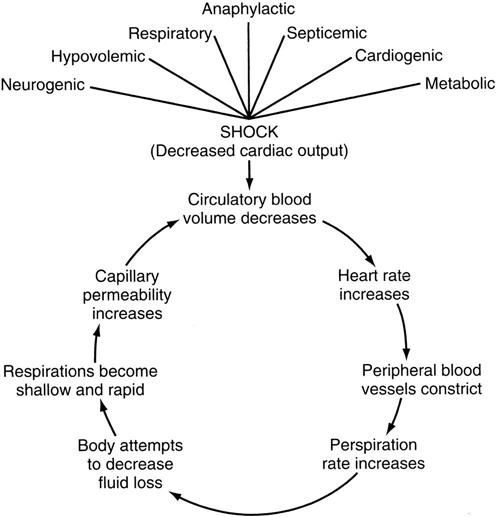
TABLE 18-4
Types of Shock and Their Causes
| Type | Cause |
| Hemorrhagic (hypovolemic) | Blood loss |
| Respiratory | Inadequate blood supply |
| Neurogenic | Loss of vascular control by nervous system |
| Psychogenic | Common fainting |
| Cardiogenic | Insufficient pumping of blood by the heart |
| Septic | Severe infection and blood vessel damage |
| Anaphylactic | Allergic reaction |
| Metabolic | Loss of body fluid |
Circulatory collapse in trauma patients is caused primarily by blood loss from vascular damage or fracture, or hypovolemic shock, but the examiner must remember that shock in trauma may also be caused by tension pneumothorax, central nervous system injury, or pericardial tamponade (heart compression resulting from blood in the pericardium)—all emergency conditions that require physician intervention.30 By the time hypovolemic shock becomes evident, blood loss may be as high as 20% to 25%. The normal range of blood pressure is 100 to 120 mm Hg for systolic pressure and 60 to 80 mm Hg for diastolic pressure. With shock, the blood pressure gradually decreases. If the blood pressure can be measured, it is best to assume that shock is developing in any injured adult whose systolic blood pressure is 100 mm Hg or less.
If the examiner is caring for a dark-skinned person, it may be difficult to determine from observation whether the patient is going into shock. A healthy person with dark skin usually has a red undertone and shows a healthy pink color in the nail beds, lips, and mucous membranes of the mouth and tongue. A dark-skinned patient in shock, however, has a gray cast to the skin around the nose and mouth, especially if experiencing respiratory shock. The mucous membranes of the mouth and tongue, the lips, and the nail beds have a blue tinge. If the shock is caused by hypovolemia, the mucous membranes of the mouth and tongue will not be blue; rather they will have a pale, graying, waxy pallor.31
If no pulse is present, then the cardiac portion of CPR techniques should be initiated. Sports equipment (such as, shoulder pads or rib pads) should be removed, at least anteriorly, to give the examiner clear access to the anterior chest wall. CPR provides only approximately 25% of normal cardiac output, so it is imperative that it is performed properly by knowledgeable persons.32 CPR is maintained until the patient recovers or EMS personnel arrive. If a cervical spine injury is suspected, CPR must be done with care, because compression to the heart can cause repeated flexion-extension of the cervical spine.17
Assessment for Bleeding, Fluid Loss, and Shock
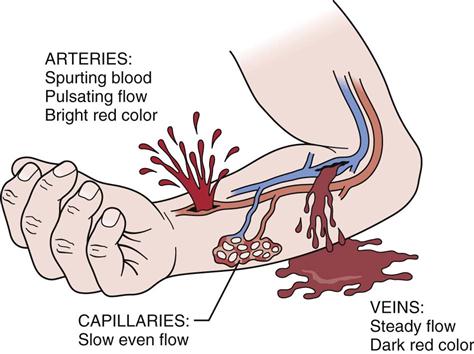
The examiner should look for any signs of external bleeding or hemorrhage (Table 18-5). The types of wounds in which external bleeding or hemorrhage may be seen are incisions, which are clean cuts, or lacerations that have jagged edges. A contusion may produce internal bleeding, whereas a puncture or abrasion may also show bleeding or oozing on the surface. Major traumatic injuries, such as fractures (e.g., pelvis, femur), can cause a great deal of internal bleeding. Of the five types of wounds, the puncture wound is probably the most difficult to treat, because it has the highest probability of infection. The examiner should watch for bleeding from the lungs, the stomach, the upper bowel, the lower bowel, the kidneys, or the bladder. If the liver, spleen, or kidney is injured, serious internal bleeding may result; the blood will not be visible because it is contained within the abdominal cavity. In this case, the patient may experience abdominal rigidity, pain, and difficulty breathing (pressure on diaphragm).
TABLE 18-5
Bleeding Characteristics and Their Source
| Source | Bleeding Characteristics |
| Artery | Bright red, spurting or pulsating flow |
| Vein | Dark red, steady flow |
| Capillary | Slow, even flow |
| Lungs | Bright red, frothy |
| Stomach | “Coffee grounds” vomitus |
| Upper bowel | Tarry black stools |
| Kidneys | Smoky, red urine |
| Bladder | Red urine, difficulty urinating |
| Abdomen | Blood not visible; abdominal rigidity, pain, difficulty breathing |
When inspecting a bleeding structure, the examiner should note the type of vessel affected. For example, an artery spurts blood, whereas a vein provides an even flow. Capillaries tend to ooze bright blood (Figure 18-8).18 Because arterial bleeding is of greatest concern, the examiner must be aware of the pressure points in the body (see Figure 18-6) so that he or she will know where to apply proper treatment. The examiner chooses the pressure point closest to the area of bleeding and applies pressure to the artery to slow or stop the bleeding. Tourniquets should be used only with extreme caution and in selected instances (e.g., accidental amputation of a limb, very severe bleeding from a major artery, or the need to apply CPR with no assistance available) and then only with enough pressure to stop bleeding. If a tourniquet is used, the time of tourniquet application should be noted carefully to prevent unnecessary tissue damage. Hemodynamic stability is best maintained by applying direct pressure to an open wound, keeping the patient in a recumbent position, and minimizing the number of times the patient is moved.16
If signs and symptoms of shock are present but visible bleeding is minimal, the examiner should suspect hidden bleeding within the abdomen, chest, or extremities.19,33 If bleeding is suspected in the abdomen, the examiner should palpate the abdominal wall for shape and distention. To check for bleeding in the chest or extremities, the examiner should look for deformities (e.g., fractures). The fingers may be used to percuss the chest area, noting any loss of hollow sounds, to help locate the presence of fluid or blood. Hyporesonance may indicate a solid organ or the presence of fluid or blood; hyperresonance usually indicates air- or gas-filled spaces.19
After the ABCs systems have been assessed and controlled, the examiner can proceed to the remainder of the primary assessment. The examiner should check the ears and nose for the presence of cerebrospinal fluid. If blood or cerebrospinal fluid leaks from the ear, this may indicate a skull fracture. The examiner should incline the head toward the affected side to facilitate drainage, unless a cervical injury is suspected. The examiner can place a gauze pad over the patient’s ear or nose where the bleeding is occurring to collect the fluid on the gauze (Figure 18-9). The examiner should look for an orange halo forming on the pad (see Figure 2-42). The halo is cerebrospinal fluid, the presence of which is a good indication of a skull fracture.34
Pupil Check
The examiner checks the pupils for shape and for response to light by using a penlight or by covering the eye with one hand and then taking it away. The pupil normally reacts to the intensity of light or focal distance. The pupils dilate in a dark environment or with a long focal distance, and they constrict in a light environment or with a short focal distance. Normally, the pupils are equally or almost equally dilated (diameter range, 2 to 6 mm; mean of 3.5 mm), but injury to the central nervous system (e.g., head injury) may cause the pupils to dilate unevenly. Some people normally have unequal pupil sizes, and the health care professional must be aware of this possibility. In a fully conscious, alert person who has sustained a blow near the eye, a dilated, fixed pupil is most likely the result of trauma to the short ciliary nerves of that eye rather than the result of third cranial nerve compression caused by brain herniation.16 Drugs may also affect the pupillary size. For example, opiate drugs cause pinpoint pupils, whereas amphetamines may cause dilated pupils.19
To test pupil reaction, the examiner holds one hand over one eye and then moves the hand away quickly, or shines the light from a penlight into the eye, and observes the pupil’s reaction when the light is shone on the eye (normal reaction: constriction) or when the light source is removed (normal reaction: dilation). The examiner tests the other eye in a similar fashion and compares the results. The pupillary reaction is classified as brisk (normal), sluggish, nonreactive, or fixed. An ovoid or slightly oval pupil or a fixed and dilated pupil indicates increasing intracranial pressure.19 If both pupils are midsize, midposition, and nonreactive, midbrain damage is usually indicated. The fixation and dilation of both pupils is a terminal sign of anoxia and ischemia to the brain.19,35
Assessment for Spinal Cord Injury
Spinal cord injuries can have catastrophic and irreversible neurologic consequences, so early recognition of the problem is essential.36 If the athlete walks off the field before notifying the medical staff of a potential neck injury, he or she should be examined using a regular cervical assessment (see Chapter 3). If the player appears to have or communicates a neck injury on the field or is unconscious, then a neck or head injury should be assumed, and he or she is treated as indicated below. The cervical assessment is modified so as much of the examination as possible is done without moving the athlete. After examination, the athlete is immobilized and transported to a medical facility.37
An upper spinal cord injury should be suspected, at least initially, if the patient has neck pain; the patient’s head position is asymmetric or abnormal; the patient is having respiratory difficulty, especially if the chest is not moving (absence of abdominal or diaphragmatic breathing); the patient is demonstrating priapism (erection of the penis); or the patient is unconscious after a fall or other contact activity. Other indications of neurological injuries in the conscious patient include numbness, tingling, or burning, especially below the clavicles; muscle weakness; twitching; or paralysis of the arms or legs, especially bilaterally (flaccid paralysis).19
The examiner may ask the patient to stick out the tongue, wiggle the toes, move the feet or arms, or squeeze the examiner’s fingers.12 This quick test provides a rapid assessment of the brain and spinal cord by showing whether the patient can follow instructions and can do the activity.
If the patient is unconscious (Table 18-6), the examiner should reassess the level of unconsciousness if possible and treat the patient as though a spinal injury has occurred. In the unconscious patient, the examiner should watch for spontaneous limb movement, especially after the application of a painful stimulus, because movement indicates that the patient is less likely to have suffered a severe cervical injury.19 In addition, the examiner should look for tonic posturing that indicates a severe head injury. The fencing response may occur at the time of impact with one limb extending and the other flexing regardless of position or gravity (Figure 18-10).38 Decerebrate rigidity is evidenced by all four extremities being in extension. With decorticate rigidity, the lower limbs are in extension and the upper limbs are in flexion (see Figure 2-33).
TABLE 18-6
Some Common Causes of Unconsciousness in Patients
| Category | Problem | Cause | Pathophysiology | Management |
| General | Loss of consciousness | Injury or disease | Shock, head injury, other injuries, diabetes, arteriosclerosis | Need for CPR, triage |
| Disease | Diabetic coma | Hyperglycemia and acidosis | Inadequate use of sugar, acidosis | Complex treatment for acidosis |
| Insulin shock | Hypoglycemia | Excess insulin | Sugar | |
| Myocardial infarct | Damaged myocardium | Insufficient cardiac output | Oxygen, CPR, transport | |
| Stroke | Damaged brain | Loss of arterial supply to brain or hemorrhage within brain | Support, gentle transport | |
| Injury | Hemorrhagic shock | Bleeding | Hypovolemia | Control external bleeding, recognize internal bleeding, CPR, transport |
| Respiratory shock | Insufficient oxygen | Paralysis, chest damage, airway obstruction | Clear airway, supplemental oxygen, CPR, transport | |
| Anaphylactic shock | Acute contact with agent to which patient is sensitive | Allergic reaction | Intramuscular epinephrine, support, CPR, transport | |
| Cerebral contusion, concussion, or hematoma | Blunt head injury | Bleeding into or around brain, concussive effect | Airway, supplemental oxygen, CPR, careful monitoring, transport | |
| Emotions | Psychogenic shock | Emotional reaction | Sudden drop in cerebral blood flow | Place supine, make comfortable, observe for injuries |
| Environment | Heatstroke | Excessive heat, inability to sweat | Brain damage from heat | Immediate cooling, support, CPR, transport |
| Electric shock | Contact with electric current | Cardiac abnormalities, fibrillation | CPR, transport; do not treat until current controlled | |
| Systemic hypothermia | Prolonged exposure to cold | Diminished cerebral function, cardiac arrhythmias | CPR, rapid transport, warming at hospital | |
| Drowning | Oxygen, carbon dioxide, breath holding, water | Cerebral damage | CPR, transport | |
| Air embolism | Intravascular air | Obstruction to arterial blood flow by nitrogen bubbles | CPR, recompression | |
| Decompression sickness (“bends”) | Intravascular nitrogen | Obstruction to arterial blood flow by nitrogen bubbles | CPR, recompression | |
| Injected or ingested agents | Alcohol | Excess intake | Cerebral depression | Support, CPR, transport |
| Drugs | Excess intake | Cerebral depression | Support, CPR, transport (bring drug) | |
| Plant poisons | Contact, ingestion | Direct cerebral or other toxic effect | Support, recognition, CPR, identify plant, local wound care, transport | |
| Animal poisons | Contact, ingestion, injection | Direct cerebral or other toxic effect | Recognition, support, CPR, identify agent, local wound care, transport | |
| Neurological | Epilepsy | Brain injury, scar, genetic predisposition, disease | Excitable focus of motor activity in brain | Support, protect patient, transport in status epilepticus |
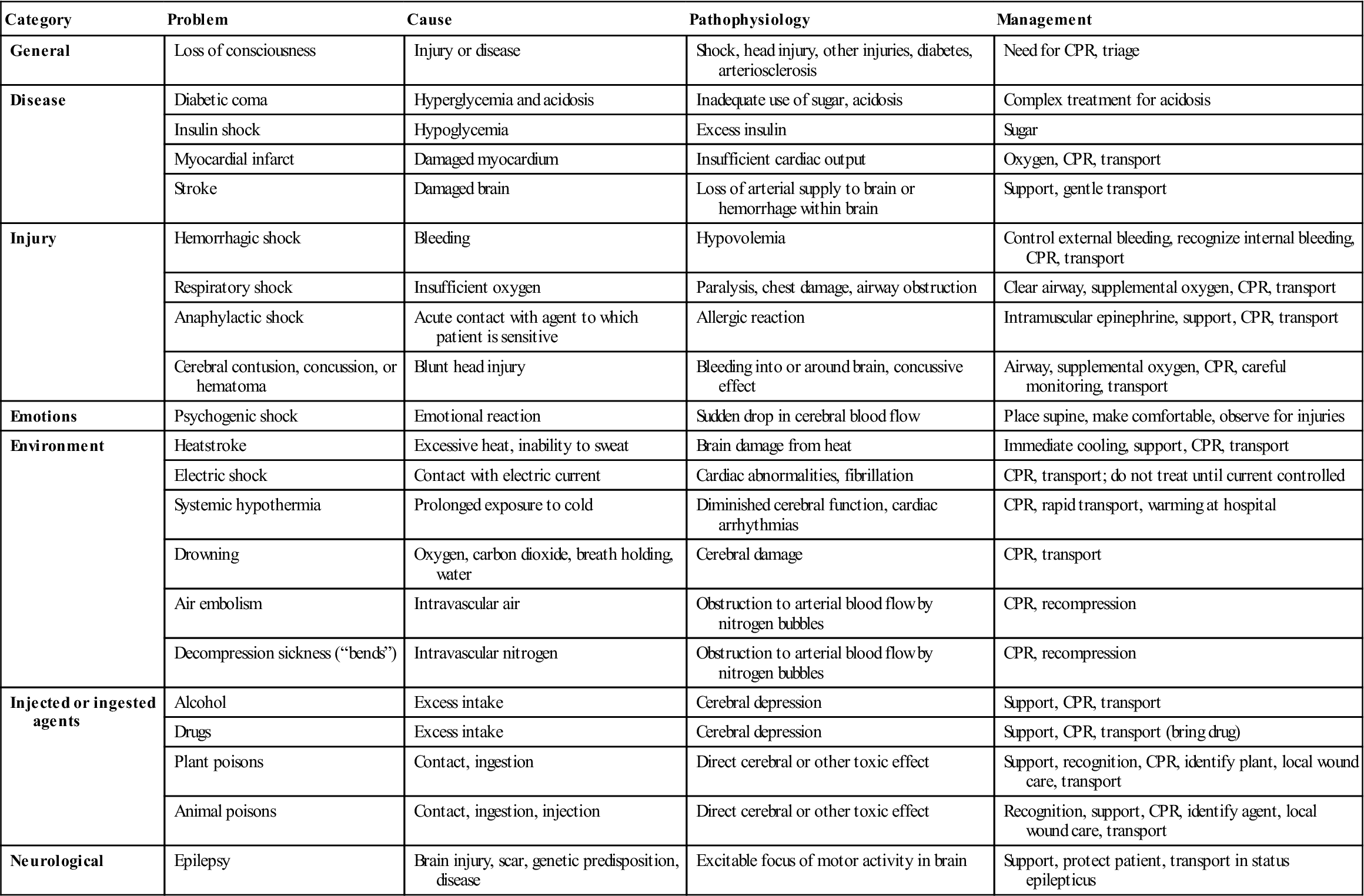
CPR, Cardiopulmonary resuscitation.
From the American Academy of Orthopaedic Surgeons: Athletic training and sports medicine, ed 2, Park Ridge, IL, 1991, AAOS, pp. 618–619.
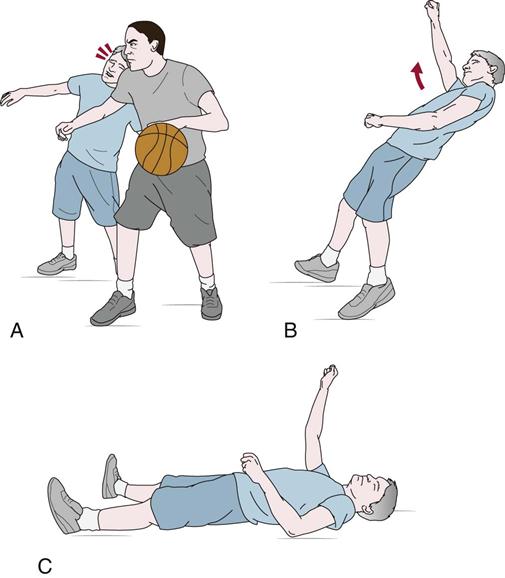
A, Athlete receives a blow to the head. B, After the traumatic blow to the head, the unconscious athlete immediately exhibits extension in one arm and contralateral flexion while falling to the ground. C, During prostration, the rigidity of the extended and flexed arms is retained for several seconds as flaccidity gradually returns.38
Assessment for Head Injury (Neural Watch)
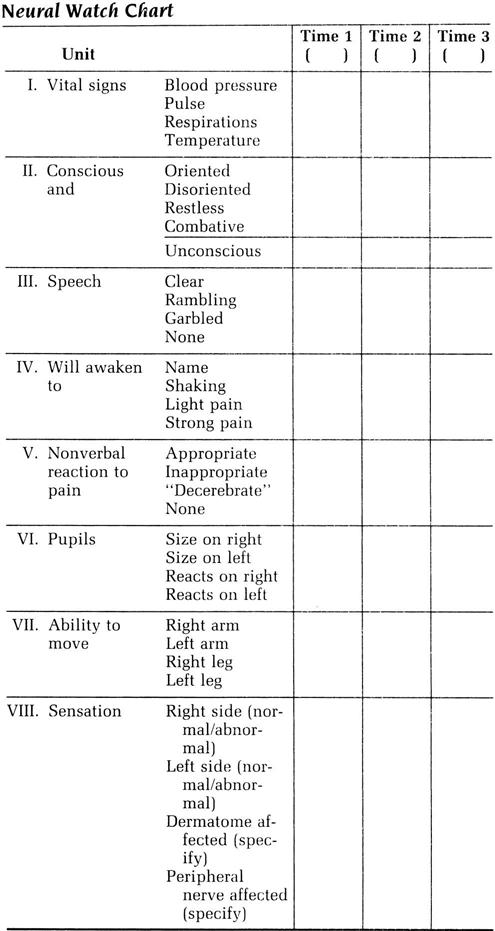
The patient’s level of consciousness is then reassessed. The examiner should now institute a Neural Watch (Figure 18-11) or a similar observation scheme to note any changes in the patient over time. The Neural Watch should initially be performed every 5 to 15 minutes, because it also facilitates monitoring of the patient’s vital signs.19 After the patient has stabilized, Neural Watch recordings may be made every 15 to 30 minutes.29 If possible, reassessment by the same examiner allows the detection of subtle changes.
The examination should include an evaluation of the patient’s facial expression; a determination of the patient’s orientation to time, place, and person; and the presence of both posttraumatic amnesia and retrograde amnesia. Signs and symptoms that demand emergency action in a patient who has sustained a blow to the head are increased headache, nausea and vomiting, inequality of pupils, disorientation, progressive or sudden impairment of consciousness, gradual increase in blood pressure, and diminution of pulse rate.
Reaction to pain and the level of consciousness can be determined by the use of physical and verbal stimuli. If there is no cervical injury, the verbal stimuli may include calling the patient’s name and shaking and shouting at the patient. Physical stimuli (see Figure 2-32) include squeezing the Achilles tendon, squeezing the trapezius muscle, squeezing the soft tissue between the patient’s thumb and index finger, squeezing an object (pen or pencil) between the patient’s fingers, squeezing a fingertip, or applying a knuckle to the sternum. (This must be done with caution because it may cause bruising.) In comatose patients, a motor response to a painful stimulus to an extremity may indicate intact pain appreciation from that site, especially if it is accompanied by a more remote response, such as a grimace or a change in respiration or pulse.16
The level of consciousness can best be determined with the use of the Glasgow Coma Scale (GCS) (see Table 2-20).39–41 The sooner the patient is tested with the scale, the better, because the initial assessment can be used as a baseline for improvement or deterioration in the patient. The GCS is often used in conjunction with the Neural Watch. For a description of the test, see Chapter 2.
Deterioration of consciousness may result from many conditions, such as increased intracranial pressure caused by an expanding intracranial lesion, hypoxia (which can aggravate cerebral edema and increase the intracranial pressure), epilepsy, meningitis, or fat embolism. The examiner should always look for signs of expanding intracranial lesions (see Chapter 2), especially if the patient is conscious. These lesions are emergency conditions that must be attended to immediately because of their potentially high mortality rate (up to 50%).
If the patient experiences loss of consciousness or appears to have disturbed senses, is seeing stars or colors, is dizzy, or has auditory hallucinations or a severe headache, the patient should not be left alone or allowed to return to activity (Table 18-7). In addition, nausea, vomiting, lethargy, increasing blood pressure, disturbed sensation of smell, or a diminished pulse should lead the examiner to the same conclusion. Amnesia, hyperirritability, an open wound, unequal pupils, or leaking of cerebrospinal fluid or blood from the ears or nose also indicates an emergency condition. Numbness on one side of the body or a large contusion in the head area should likewise lead the examiner to handle the patient with care. If the frontal area of the brain is affected, the patient may experience lapses of memory, personality changes, or impairment of judgment. If the temporal lobe has been affected, the patient may experience feelings of unreality, déjà vu, or hallucinations involving odors, sounds, or visual disturbances, such as macropsia (seeing objects as larger than they really are) or micropsia. The literature indicates that head injury depends not only on the magnitude and direction of impact and the structural features and physical reactions of the skull but also on the state of the head/brain at the moment of impact.6,42,43
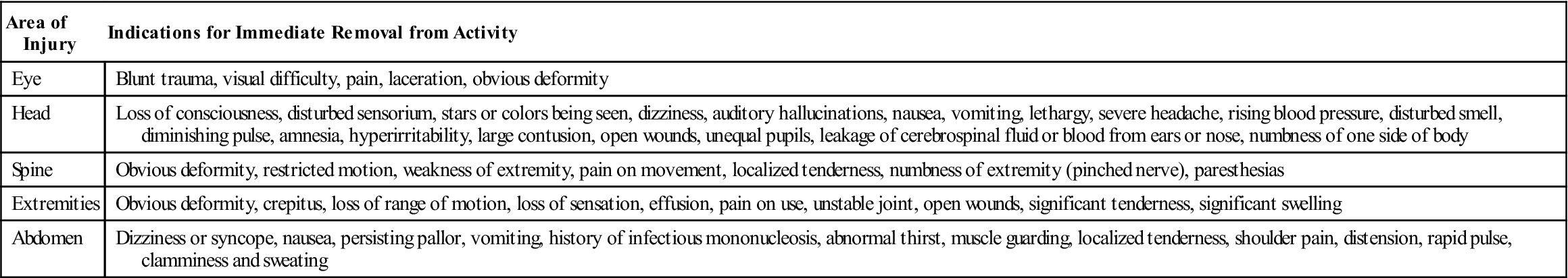
TABLE 18-7
Indications for Immediate Removal from Activity
| Area of Injury | Indications for Immediate Removal from Activity |
| Eye | Blunt trauma, visual difficulty, pain, laceration, obvious deformity |
| Head | Loss of consciousness, disturbed sensorium, stars or colors being seen, dizziness, auditory hallucinations, nausea, vomiting, lethargy, severe headache, rising blood pressure, disturbed smell, diminishing pulse, amnesia, hyperirritability, large contusion, open wounds, unequal pupils, leakage of cerebrospinal fluid or blood from ears or nose, numbness of one side of body |
| Spine | Obvious deformity, restricted motion, weakness of extremity, pain on movement, localized tenderness, numbness of extremity (pinched nerve), paresthesias |
| Extremities | Obvious deformity, crepitus, loss of range of motion, loss of sensation, effusion, pain on use, unstable joint, open wounds, significant tenderness, significant swelling |
| Abdomen | Dizziness or syncope, nausea, persisting pallor, vomiting, history of infectious mononucleosis, abnormal thirst, muscle guarding, localized tenderness, shoulder pain, distension, rapid pulse, clamminess and sweating |
If the patient has received a head injury and has been checked by a physician and it has been determined that it is not necessary to send the patient to the hospital, the clinician should ensure that the patient and whoever lives with the patient understands what to look for in terms of signs and symptoms that may indicate increasing severity of head injury. Figure 2-34 demonstrates typical home health care guidelines.
Assessment for Heat Injury
If the examiner suspects a heat-type injury with no cervical injury, only heat exhaustion and heat stroke need be considered as life-threatening.10,44 Heat fatigue or exhaustion occurs when a person is exposed to high environmental temperature or humidity and perspires excessively without salt or fluid replacement. Heat stroke can occur when a non-acclimatized person is suddenly exposed to high environmental temperature or humidity. The thermal regulatory mechanism fails, perspiration stops, and the body temperature increases. Above 42° C oral body temperature, brain damage occurs, and death follows if emergency measures are not instituted. The diagnostic keys in this situation are the high body temperature and the absence of sweating. Initial signs of heat injury include muscle cramps, excessive fatigue or weakness, loss of coordination, decreased reaction time, headache, decreased comprehension, dizziness, and nausea and vomiting.
The body temperature varies according to the site at which the measurement is taken. The oral body temperature is 37° C (98.6° F). Taken in the armpit or axilla, the temperature is 36.4° C to 36.7° C (97.5° F to 98.1° F), and in the rectum, it is 37.3° C to 37.6° C (99.1° F to 99.7° F).
The examiner may palpate the skin to get some idea of the external temperature of the body and possible pathology (Table 18-8). Hot and dry skin is often caused by heat stroke, high fever, or hyperglycemia. Cold and clammy skin is caused by hypoglycemia, shock, fainting, or hyperventilation. Cool and moist skin is often caused by heat exhaustion, whereas cool and dry skin is caused by exposure to cold.
TABLE 18-8
| Skin Change | Cause |
| Hot and dry | Heat stroke, high fever, hyperglycemia |
| Cold and clammy | Fainting, hypoglycemia, hyperventilation, shock |
| Cool and moist | Heat exhaustion |
| Cool and dry | Cold |
| White pallor | Decreased circulation |
| Cyanosis (blue pallor) | Respiratory distress |
| Red pallor | Fever, heat stroke, inflammation, exercise |
Skin color can also play a significant role. Pallor, or whitish skin, indicates circulatory disturbance or decreased circulation and is most often associated with trauma and shock. Cyanosis, or a blue tint to the skin, indicates respiratory distress, as does a gray tint. Redness indicates an increase in blood flow as a result of fever, heat stroke, or exercise.
Assessment for Movement
While doing the initial assessment, the examiner should also be considering how the patient will be moved and immobilized (e.g., self-ambulation, stretcher, spinal board) depending on the severity of the injury, and whether the patient can move him or herself or can move only with assistance.45
If the patient has not already done so, the examiner asks the patient to move the limbs to reassess for a cervical spine injury and look for major trauma (e.g., fracture, dislocation, third-degree strain, third-degree sprain). At the same time, the examiner may palpate the areas of potential injury, noting any pain, abnormal bone or joint alignment, swelling, hypersensitive or hyposensitive areas, or palpable defect (third-degree strain).4 If movement is relatively normal, the examiner quickly checks the myotomes of the upper or lower body for any possible motor involvement or motor impairment. Changes in limb power may be caused by a contractile tissue injury, a neurological injury, or an expanding intracranial lesion, which will be displayed as progressive weakness in the contralateral arm or leg.29 Decreased limb power can also be caused by reflex inhibition as a result of previously unrecognized limb injury. In these cases, contractions are weak and painful. These types of injuries are placed in the low-priority group (see Table 18-1) because they represent a threat to the limb rather than to the life of the patient.17
Positioning the Patient
Normally, a patient is left in the position in which he or she is found until the primary assessment is completed. However, if the patient is having difficulty breathing or there is no pulse, the patient must be positioned to do CPR. If the conscious patient is prone and in respiratory difficulty, the examiner, with assistance, should log-roll the patient (Figure 18-12) onto a spinal board so that an attempt can be made to restore the airway. During any movement of the patient, the examiner should apply traction of about 4.5 kg (10 lbs) to the cervical spine to maintain stability. The patient should be reassured that others are going to carefully move the patient while he or she remains still. Before any movement is attempted, the patient and those who are going to assist the examiner should know what the examiner plans to do and what their jobs are. This requires frequent practicing of emergency procedures. The sequence of movement and positioning of the extremities and body of the patient should be thought out beforehand so that everyone is aware of what is going to happen and in what order. The proper procedure for moving the patient should be practiced often to ensure competency.
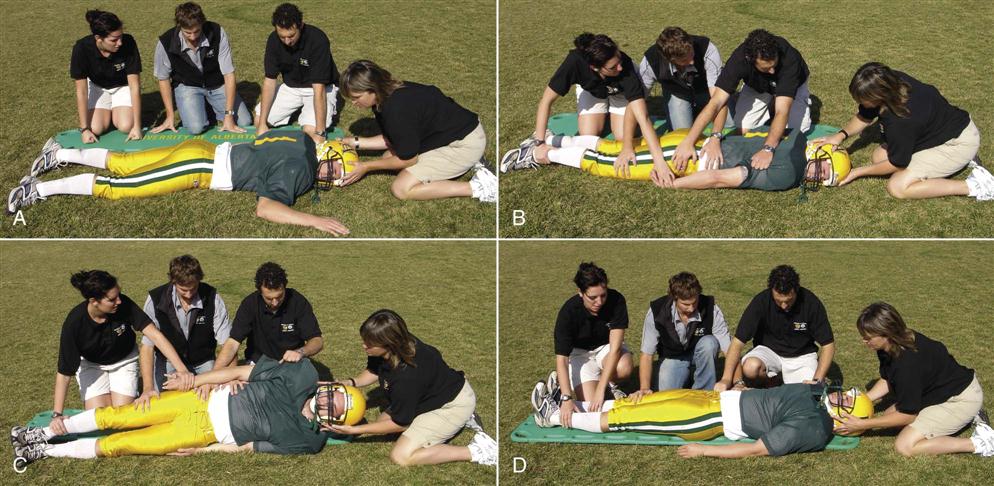
Note that the head and neck are stabilized throughout the movement. A, Patient prone, examiner stabilizes head and gives instruction to helpers. B through D, Patient is log-rolled onto spinal board.
To roll the patient, at least three assistants are needed. There should be two-way communication between the examiner and the patient at all times to continually evaluate the patient’s comfort level and neurological signs. The assistants should place the spinal board beside the patient and then kneel beside the spinal board and patient (see Figure 18-12, A). They should reach over the patient and hold the patient’s shoulder, hip, and knees (see Figure 18-12, B). On command from the examiner, the assistants roll the patient toward them while the examiner stabilizes the head (see Figure 18-12, C) until the patient is lying supine on the spinal board (see Figure 18-12, D). Only rolling—not lifting—should occur. With the patient in the supine position, proper CPR techniques may be applied, or the patient may be transported. The patient may also be covered with a blanket to provide warmth.
If a spinal injury is suspected and the conscious patient is in the prone position but has no difficulty breathing, the patient is log-rolled halfway toward the assistants while another assistant slides the spinal board as close as possible to the patient’s side. The patient is then rolled directly onto the spinal board in the prone position. Similarly, if a spinal injury is suspected and the patient is in the supine position and breathing normally, the patient is rolled toward the assistants while another assistant slides the spinal board under the patient as far as possible. The patient is then rolled back onto the spinal board in the supine position. If a spinal injury is suspected and the patient is in side lying, the patient is log-rolled directly onto the spinal board and into the supine position. In each of these cases, the examiner controls the head, applies traction, and instructs the assistants. The patient’s head is then stabilized and immobilized with sandbags, a head immobilizer, or triangular bandages, and the patient is strapped to the spinal board with restraining belts. If a collar is used to stabilize the spine, it must do so during movement as well as when the patient is stationary; it must not hinder access to the carotid pulse, airway, or performance of CPR; it must be easy to assemble and apply; it must be adaptable to patients of all ages and sizes; and it must allow radiological examination without removal.46,47 Any major injury (such as, a head injury, a spinal injury, or a fracture) requires appropriate handling, slow and deliberate management, and proper transportation to provide a satisfactory outcome. These techniques must be practiced repeatedly.
If possible and if time permits, especially if the assistants are not used to working together, a simulated roll and transport using an uninjured person should be attempted before moving the patient to ensure that all involved know what they are doing in terms of patient positioning, movement sequence, and specific handling (e.g., head, hands, feet) so that any transfer or movement of the patient is effective and organized.
During the emergency assessment, if the patient is nauseated, is vomiting, or has fluid draining from the mouth, and provided breathing and circulation are normal, the patient should be placed in the recovery position (Figure 18-13) as long as there is no suspicion of a spinal injury. This side lying position enables the patient to be continually monitored (ABCs) and allows the examiner to easily observe any change in condition while waiting for emergency personnel. The patient’s head should be positioned to keep the airway open and to allow drainage from the throat and mouth. If the blood flow to the heart and brain has diminished, circulation can be improved by elevating the lower limbs, provided that the position change can be accomplished without causing further pain or breathing problems or aggravating an injury. If the patient has breathing difficulties or a chest injury or has experienced a heart attack or stroke, it may be desirable to lower blood pressure in the injured parts by elevating the upper part of the body slightly, if the position change can be accomplished without causing further pain or breathing problems.

If the patient is unconscious and the cardiac and circulatory functions are not compromised, the patient should be left in the original position until consciousness is regained. However, if the patient is unconscious and lying supine, the examiner should always watch for the possibility that the patient may “swallow” the tongue and obstruct the airway. Also, an unconscious patient loses the cough reflex, and if vomiting or bleeding occurs, vomitus, mucus, or blood may enter and obstruct the airway. Therefore, the examiner may elect to put the patient in the recovery position.
If the patient is unconscious and in respiratory or cardiac distress, the examiner must quickly assess the patient and attempt to restore respiratory and cardiac function. This patient is then treated the same as the conscious patient.
If the patient’s spine is twisted or flexed and the patient is reasonably comfortable, the patient should be stabilized in that position until a spinal injury is ruled out. If there has been a loss of breathing or cardiac function, the examiner must carefully correct the deformity, place the patient in the supine lying position, and perform the appropriate measures to deal with the problem.
If a cervical spine injury has occurred to a child of 7 years of age or younger, the examiner should realize that in these children, the head is normally larger in proportion to the rest of the body. If the child is positioned on a spinal board without modification, the neck will be forced into some flexion. To alleviate this problem, the spinal board should have a cutout for the head, or a pad for the chest or rest of the body should be added to elevate it in relation to the head.48
If the patient is in the water and unconscious, he or she must be reached as quickly as possible. The rescuer should not jump into the water, because this action creates waves that may rock the victim’s head and could cause severe consequences if a neck injury has occurred. The examiner should approach the patient head-on and place an extended arm down the middle of the patient’s back with the patient’s head in the examiner’s axilla. The examiner then grasps the patient’s biceps with the forearm around the patient’s forehead, slowly lifts the arm, and turns the patient face up. The examiner’s forearm locks the patient’s head in the examiner’s axilla during the turn. Once the patient is supine, both of the examiner’s arms support the patient’s head and spine in the water. An assistant then slides the spinal board under the patient in the water and blocks the patient’s head with towels. The patient is next strapped to the spinal board with restraining straps and is lifted out of the water.49 If a spinal board is not available and a cervical injury is suspected, the patient should be supported in the water until emergency personnel arrive.
In some sports (e.g., ice hockey, lacrosse, motor car or motorcycle racing, football), the athletes wear helmets. Whether the helmet should be removed to institute emergency procedures is a controversial issue and often depends on the type of training (EMS versus sports therapy) and experience of the health care professional.2,45,50–53 Generally, if the patient is unconscious, the helmet should not be removed unless the examiner is absolutely certain that there has not been a neck injury. In the patient who wears both helmet and shoulder pads, both should be left on the patient, because they help to maintain the cervical sagittal alignment close to normal. Ideally, the helmet and shoulder pads should be removed in a controlled setting, such as the emergency department.2,54,55 Helmets should be removed only if the facemask or visor interferes with adequate ventilation;54,56 if the facemask interferes with the clinician’s ability to restore an adequate airway;54,56 if the helmet is so loose that it does not provide adequate immobilization of the head when secured to the spinal board;54,56 if life-threatening hemorrhage under the helmet cannot be controlled;54,56 if, in children, the helmet is too large and causes flexion of the neck when used as part of the immobilization;48,54,56 or if it is necessary to defibrillate the patient. In the last case, the shoulder pads must be removed, so the helmet should be removed to maintain spinal position.4 If the patient is in respiratory distress, facemasks can usually be easily removed with the use of an X-Acto knife or similar device to release the restraining straps while holding the mask in place.
If, for whatever reason, the decision is made to remove the headgear, the neck and head must be held as rigid as possible. Therefore, at least two people are needed: one to stabilize the head and neck and one to remove the facemask. One person, usually the assistant, first applies in-line traction is to the helmet to ensure initial stability. A second person, usually the examiner, then stands at the side of the patient and employs in-line traction by applying a traction force through the patient’s chin and occiput. The assistant stops applying traction and, if the helmet is a football helmet, first removes the cheek pads by sliding a flat object (e.g., scissors handle) between the cheek pad and helmet, twisting the object to cause the pads to unsnap. After the pads are removed, the assistant applies bilateral expansion to the helmet so that the ears are cleared as the helmet is removed.4 After the helmet has been removed, the assistant reapplies in-line traction from the head, and the examiner then releases the traction and continues the primary examination.43 If desired, the examiner may apply a cervical collar, such as the Stifneck collar, but this should be done with caution because cervical collars do not completely eliminate movement in the cervical spine.57
If the helmet is removed and the patient is wearing shoulder pads, the person holding the head must ensure that the head does not fall back into extension, and a modification must be made to the spinal board. The shoulder pads should be removed only if it is impossible to do this or if defibrillation is necessary.
If the patient is conscious and there appears to be no cervical injury or other severe injury, the patient may be moved to another area for a more appropriate and complete secondary assessment. If the injury is in the upper limb and the injured part is immobilized, the patient may first be moved from a supine to a sitting or kneeling position, then from sitting or kneeling to supported standing, to unsupported standing, and finally the person may walk off the field. During these changes in position, the examiner or assistants are positioned to provide support and assistance if the patient feels dizzy or unsteady. If the injury is in the lower limb, the athlete may be helped off the field by teammates, stretcher, or cart. Spinal injuries require greater care and the use of a spinal board and cervical collar with support. Again, assistance may be required, and everyone, including the patient and assistants, should be aware of the movement sequence before it is attempted.
Injury Severity
During the primary assessment, the examiner must use some method of determining the severity of injury. There are several scales that may be used to test the severity of injury or to triage the patient, including the Galveston Orientation and Amnesia Test,58 which tests for posttraumatic amnesia; the Abbreviated Injury Scale;59 the Injury Severity Score;59–61 the Trauma Score;62 the Triage Index;63,64 the Circulation, Respiration, Abdomen, Motor, and Speech (CRAMS) Scale;65,66 and the Trauma Index.67 Of these, the Trauma Score illustrates the ease of scoring (Figure 18-14) and the survival probabilities (Table 18-9) that can be expected in trauma patients. This tool provides a dynamic score that monitors changes in the patient’s condition and is useful in making triage decisions. The CRAMS scale illustrates a similar scoring pattern (Table 18-10).
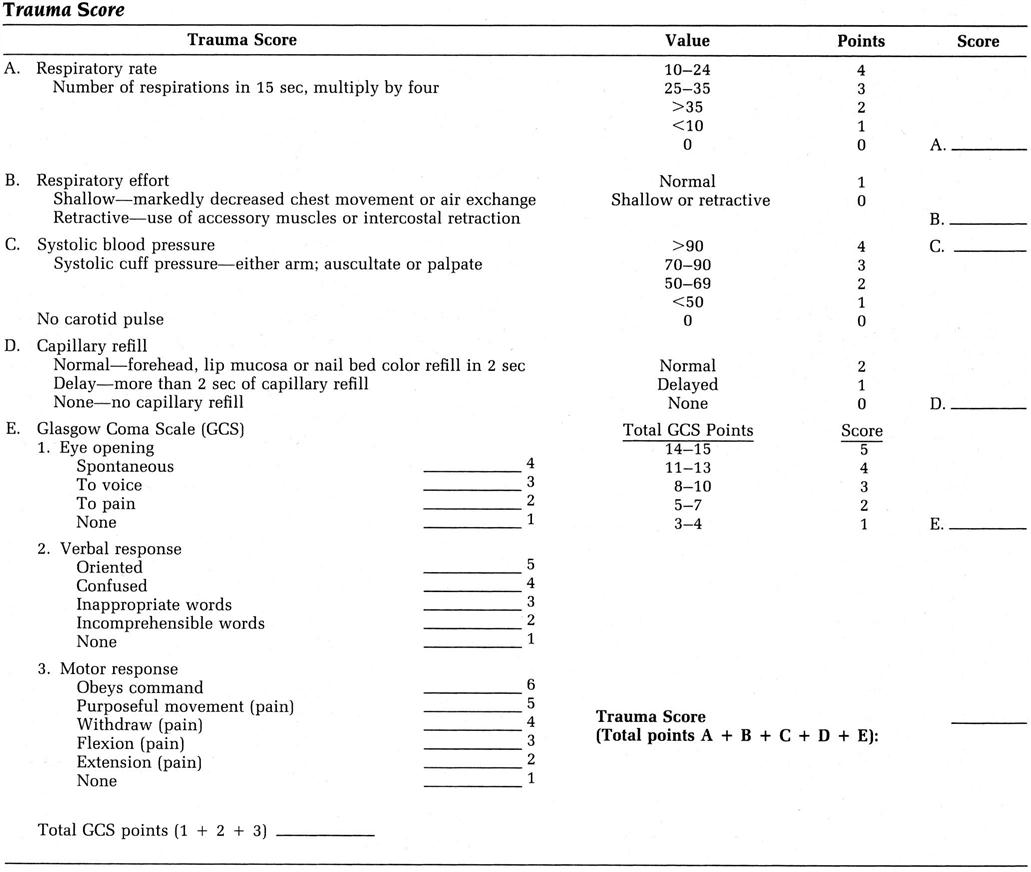
TABLE 18-9
Trauma Score and Probability of Survival Based on the Score
| Trauma Score | Probability |
| 16 | 0.99 |
| 15 | 0.98 |
| 14 | 0.95 |
| 13 | 0.91 |
| 12 | 0.83 |
| 11 | 0.71 |
| 10 | 0.55 |
| 9 | 0.37 |
| 8 | 0.22 |
| 7 | 0.12 |
| 6 | 0.07 |
| 5 | 0.04 |
| 4 | 0.02 |
| 3 | 0.01 |
| 2 | 0.00 |
| 1 | 0.00 |
From Champion HR, Sacco WJ, Carnazzo AJ, et al: Trauma score. Crit Care Med 9:674, 1981.
TABLE 18-10
| Circulation | |
| 2: Normal capillary refill and BP over 100 mm Hg systolic | |
| 1: Delayed capillary refill or BP 85 to 99 systolic | |
| 0: No capillary refill or BP less than 85 systolic | ____ |
| Respiration | |
| 2: Normal | |
| 1: Abnormal (labored, shallow, or rate over 35) | |
| 0: Absent | ____ |
| Abdomen | |
| 2: Abdomen and thorax not tender | |
| 1: Abdomen or thorax tender | |
| 0: Abdomen rigid, thorax flail, or deep penetrating injury to either abdomen or thorax | ____ |
| Motor | |
| 2: Normal (obeys commands) | |
| 1: Responds only to pain—no posturing | |
| 0: Posturing or no response | ____ |
| Speech | |
| 2: Normal (oriented) | |
| 1: Confused or inappropriate | |
| 0: No sounds or unintelligible sounds | ____ |
| (Score of 6 or less indicate referral to trauma center should be initiated) | |
| TOTAL | ____ |
BP, Blood pressure; CRAMS, circulation, respiration, abdomen, motor, and speech.
From Hawkins ML, Treat RE, Mansberger AR: Trauma victims: Field triage guidelines. South Med J 80:564, 1987. Reprinted by permission from the Southern Medical Journal.
Secondary Assessment
The examiner can proceed to the secondary assessment if the patient is conscious, is able to respond by talking coherently, shows minimal or no distress in terms of breathing, and displays normal circulation. However, the examiner must keep in mind that the patient may still have suffered a catastrophic injury (e.g., cervical spine injury) that, although not life-threatening at the present time, could lead to significant problems. For the most part, the secondary survey is predicated on the patient’s being clinically stable.8
If the patient is conscious, the examiner must constantly reassure the patient to reduce potential anxieties. By the time the secondary assessment begins, the examiner should have eliminated any possible life-threatening situations and can then complete the injury assessment. In the case of a sudden injury, the examiner should remember that the patient has had no time to prepare psychologically or practically for the injury. Therefore, the injury can represent a sudden and frightening change in the patient’s physical state. Other concerns experienced by the patient may be related to the patient’s job, financial situation, family, or prognosis, and these concerns, suddenly magnified, may affect the patient’s behavior, especially in later secondary or “sideline” assessments.
The secondary assessment is a head-to-toe rapid physical examination68 and can be performed after the examiner has ascertained that there is no threat to the patient’s life. The patient must be conscious for the examiner to perform the secondary assessment properly. The secondary survey involves a complete body survey to detect other injuries that may cause serious complications or lead to a patient’s not being allowed to return to activity. The patient should be instructed not to move unless requested by the examiner, who should also explain to the patient what is being done while the examination is being performed. It is important to maintain communication with the patient throughout the examination. During this time, the examiner is testing for possible spinal injuries, fractures, dislocations, or soft-tissue injuries. Care must be taken that injuries are not missed.69
While performing the secondary assessment, the examiner is considering whether the patient should be allowed to return to activity. The examiner must decide whether further evaluation is required on-site or whether the patient should be taken to some other venue (e.g., training room, hospital). In addition, the examiner should keep in mind that home monitoring may be necessary and therefore should determine whether a responsible person is at home to watch for changing signs and symptoms in the patient (see Figure 2-34).
When progressing to the secondary assessment, the examiner must continue to do the Neural Watch or the GCS and watch for signs of an expanding intracranial lesion or other complications. Advanced cerebral edema may further reduce the perfusion of an already damaged hemisphere of the brain, and compression of the descending motor tracts may decrease limb power. Also, the patient’s level of consciousness can reveal a deficit previously overshadowed by other evidence of severe brain injury.
During the secondary assessment, there is time to carry out a more thorough assessment for head injury or perform other tests in addition to the Neural Watch and GCS. The patient’s abilities to assimilate information and act with split-second timing are more likely to be impaired after a concussion than are strength and endurance. If a head injury is suspected, it is important to determine the patient’s reasoning and processing ability (see Chapter 2).
The examiner also checks coordination or motor neurological function.70 When testing for proper neurological function, the examiner should palpate the neck and back for any pain or tenderness.71 There are a number of tests for eye-hand coordination (see Chapter 2). Balance and motor coordination can be tested by determining whether the patient can maintain balance through unsupported standing, the Romberg test, standing with eyes closed, being pushed from side to side, balancing on one leg, or normal walking. Motor neurological function is tested by checking the patient’s grip strength or the various myotomes.
Eye coordination and peripheral vision can be checked by asking the patient to follow the examiner’s fingers up and down, side to side, diagonally, and in circles, noting any wandering eye movements. To test visual disturbance, the patient is asked to read or observe something from a short distance (e.g., eye chart, how many fingers the examiner is holding up). To test for vision at distance, the patient can be asked to read the score clock, as an example.
After brain function has been tested, the remainder of the secondary assessment is similar to the “clearing,” or scanning, assessments performed for the cervical or lumbar spine. The examiner clears the different areas of the body so that a detailed assessment of the specifically injured joints or structures can be performed. At this stage, the assessment follows the same basic protocol as in the detailed assessment of specific joints—that is, a more detailed history of the injury is taken, the patient is observed for obvious or potential problems, and the entire body is quickly scanned for injury. This is followed by a detailed examination of the specifically injured structures, including active, passive, and resisted isometric movements, special tests, testing of reflexes and cutaneous sensory distribution, joint play movement tests (if applicable), and, finally, palpation and other diagnostic tests, such as imaging and laboratory tests (see Chapters 3 to 13).
Because the examiner is one of the first persons to talk to the patient, the examiner will probably obtain the most accurate history. Simple non-leading questions should be asked, and information should be clarified in an attempt to find out what happened and what injury or injuries the patient believes have occurred. Appropriate questions related to specific joints or areas of the body can be found elsewhere in this text. The patient often can provide the examiner with the diagnosis if the examiner listens carefully. After the patient has been thoroughly questioned, others who witnessed the accident or injury may also be questioned to complete the history. Informed conversation with other persons sometimes helps the examiner to detect abnormal behavior that may not be noticed initially. If the patient has a previous medical file, it may also prove beneficial to review the contents for information regarding preexisting conditions, previous trauma, and medications.
While obtaining the patient’s history, the examiner continues to observe the patient and notes levels of consciousness, developing symptoms, pain patterns, and altered functional abilities. In addition, the examiner should carefully watch for developing signs and symptoms of an expanding intracranial lesion by noting changes in facial expression, the pupils, and the level of consciousness and by performing the Neural Watch and GCS several times. The basic observation is the same as that performed during joint assessment and includes observation of bony and soft-tissue contours, scars, deformities, the ability to move, and body alignment.
The next part of the secondary assessment is the scanning examination, in which the examiner quickly scans the entire body through observation, by asking the patient to make particular movements (depending on where the suspected injury has occurred), and by testing myotomes, dermatomes, and reflexes. During this phase, the examiner should explain what is being done and why, not only to reassure the patient but also to ensure cooperation and relaxation. This part of the examination may be done without removing the patient’s clothes, although it is better to do so because clothing may obstruct the view of the injured area. However, if the examination is being performed in the presence of other people, clothing removal should be left to a later time, or the patient should be moved to a more appropriate location. If the clothes need to be removed, the patient should be warned, especially if in a public place, and every effort should be made to maintain the patient’s dignity.
After the specific area or areas of injury have been narrowed down through the scanning examination, the examiner can perform a detailed assessment of the appropriate parts of the body, as specified in other chapters. Failure to perform a proper examination may lead to a missed assessment and more problems than originally anticipated.
The patient must be immediately sent to a hospital or trauma center if at any time during the primary or secondary evaluation the following signs are exhibited: pupillary or extraocular movement abnormality, facial or extremity weakness, amnesia, confusion or lethargy, sensory or cranial nerve abnormality, positive Babinski sign, deep tendon reflex asymmetry, or posttraumatic seizures.35,72 Proper care for the patient must always be uppermost in the mind of the examiner.
After the assessment has been completed and the patient has been stabilized, has returned to competition, or has been referred for further medical care by ambulance, the examiner should be sure to document what happened and the subsequent care that was given, noting any potential difficulties. These notes, if taken at the sideline, should be transferred to the patient’s medical record as soon as possible.