5 Emergency Cardiac Ultrasound
Evaluation for Pericardial Effusion and Cardiac Activity
• Emergency cardiac ultrasound is performed by the emergency physician to assess for the presence of cardiac activity, determine whether a pericardial effusion is present, and answer other specific questions.
• Echocardiography can be used during cardiac arrest to guide resuscitation decisions.
• Emergency use of echocardiography is indicated for assessment of cardiac ejection fraction, wall motion abnormalities, and other critical findings that will direct acute diagnostic decision making.
Introduction
Echocardiography has been the “gold standard” for cardiologists for decades. Over the past 20 years, emergency physicians have adopted point-of-care (POC) cardiac ultrasound to answer specific questions on the management of critical patients. Assessment for pericardial effusion and for cardiac activity have traditionally been the principal indications for emergency physicians, but indications for bedside echocardiography are growing rapidly.1
What We Are Looking For
The initial and best evidence-based indications include applications for tamponade, cardiac arrest, and acute heart failure. Rapidly developing areas of cardiac ultrasound include eva-luation of hypotension, pulmonary embolism (PE), acute myocardial infarction, diastolic heart failure, and echocardiographically guided resuscitation (Box 5.1).1,2
Literature Review
Estimation of Global Cardiac Function and Ejection Fraction
Multiple studies have shown the ability of emergency phy-sicians to accurately evaluate cardiac function and ejection fraction.3,4 When compared with cardiologists, emergency physicians were found to have a correlation coefficient of 0.86 with cardiologists when assessing ejection fraction. Cardiologists had a similar coefficient of 0.84 among themselves.
How to Scan/Scanning Protocols
Specific Views
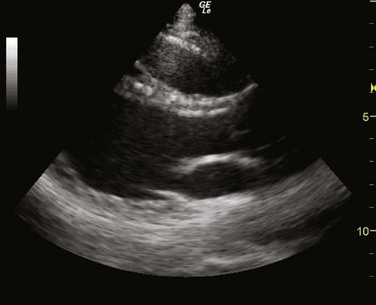
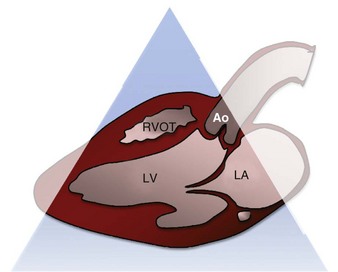
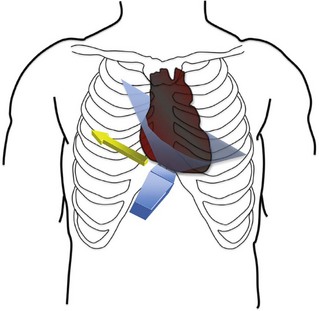
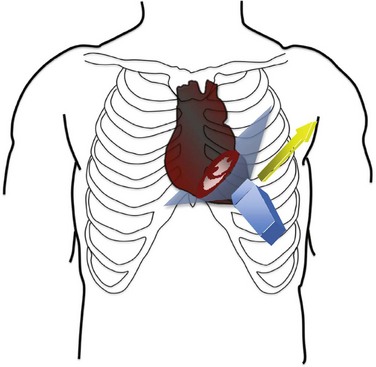
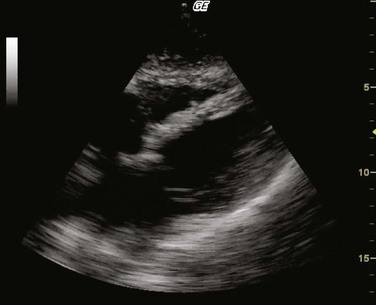
Parasternal Long Axis
The parasternal long-axis view seen in Figure 5.1 is obtained by placing the probe in the third to fourth intercostal space with the probe marker pointed toward the patient’s right shoulder (Figs. 5.2 and 5.3). The long axis of the heart should be horizontal on the screen with the apex pointed to the left. If the apex is pointed up, the probe is too low and should be moved up an interspace. This view allows visualization of the left ventricle, mitral valve, left atrium, right ventricular outflow tract, aortic valve, and aorta. The descending thoracic aorta is often visualized posterior to the left ventricle in transection.
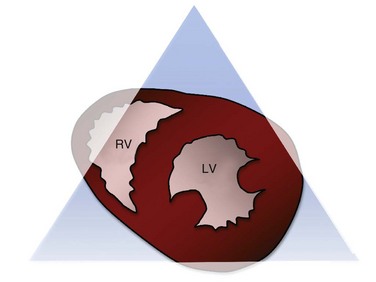
Parasternal Short Axis
The parasternal short-axis view is obtained by rotating the probe 90 degrees from the parasternal long-axis position so that the probe marker is pointed to the patient’s left shoulder (Figs. 5.4 and 5.5). The ultrasound beam is now transecting the heart in its short axis. If the physician tilts the probe so that it is pointing to the base of the heart, the aortic valve is visualized along with the “inflow and outflow” of the right heart. This view includes the right atrium, right ventricular outflow tract, and pulmonic valve. As the probe is tilted more apically, the aortic valve is lost and a cross-sectional view of the mitral valve is obtained (Fig. 5.6). At this point the right ventricle becomes more apparent and takes a position as a crescentic ventricle to the left and superficial to the mitral valve and left ventricle. Finally, as the probe is tilted more toward the apex, the mitral valve is lost and the muscular portion of the left ventricle is visualized. The posterior medial and anterior papillary muscles are visualized at this point, and the circular nature of the left ventricle can be appreciated (Fig. 5.7).
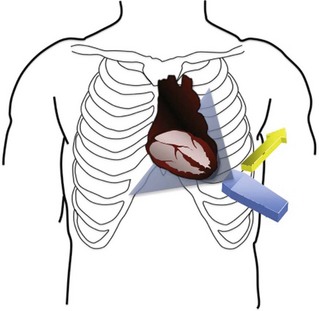
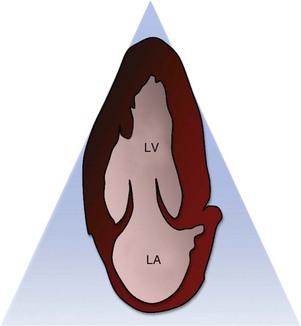
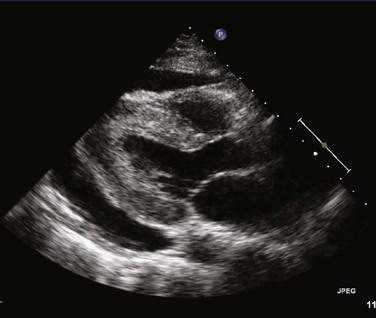
Apical Four- and Two-Chamber Views
The apical window allows visualization of either all four chambers (Figs. 5.8 and 5.9) or just two chambers (the left atrium and ventricle) (Fig. 5.10). The apical windows are difficult to obtain in the emergency setting and often require the patient to be in the left lateral decubitus position, which is often impossible. The window is obtained by placing the probe at the location of maximal impulse with the probe marker pointed to the left axilla. The probe must be tilted so that the probe is pointed to the patient’s right shoulder (Fig. 5.11).
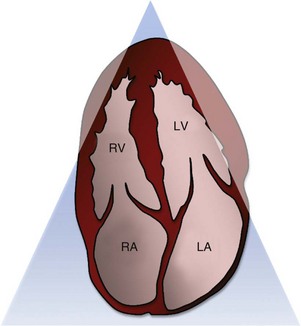
Fig. 5.8 Diagram of the apical four-chamber view.
LA, Left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
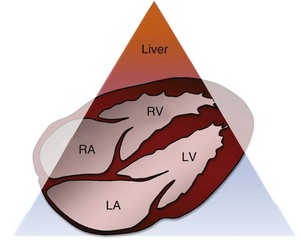
Subcostal Four-Chamber View
The subcostal four-chamber view (Figs. 5.12 to 5.14) is obtained by placing the probe just inferior to the xiphoid and applying pressure downward on the abdomen with the probe horizontal. This view can be performed with either the curvilinear abdominal probe or the phased-array thoracic probe. The probe marker should be toward the patient’s left in cardiac mode and toward the patient’s right when using focused abdominal sonography for trauma (FAST) or abdominal protocols.
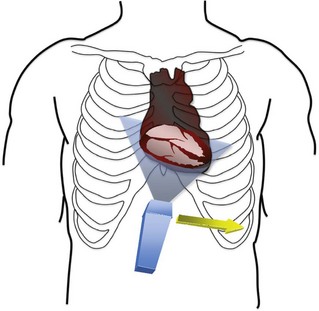
Fig. 5.13 Probe orientation for the subcostal four-chamber window.
The probe is placed in the subxiphoid space with the probe marker oriented to the patient’s left (cardiac mode) or to the patient’s right (abdomen/focused abdominal sonography for trauma mode). The apex of the heart should be pointing to the right of the screen as seen in Figures 5.8 and 5.7.
Normal and Abnormal Findings
Pericardial Effusion
Evaluation of pericardial effusion is one of the first indications for cardiac ultrasound.6 Identification of pericardial effusion (Fig. 5.15) is achieved by visualization of the heart in multiple views. The subcostal window is the most commonly taught site because of the FAST examination. An effusion will appear as an anechoic stripe of fluid surrounding the heart. This stripe is most commonly located between the right ventricle and the liver. Ideally, all three acoustic windows should be used when attempting to rule out pericardial effusion.
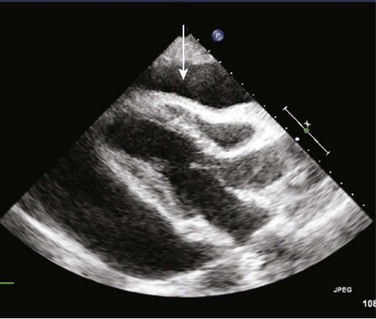
The critical complication of pericardial effusion is cardiac tamponade (Fig. 5.16). Physiologically, cardiac tamponade occurs when the pressure inside the pericardial sac becomes elevated above right ventricular diastolic filling pressure. This leads to decreased filling of the right ventricle in diastole and reduced preload and cardiac output. Echocardiographic signs of cardiac tamponade are the presence of right ventricular free wall collapse as seen in Figure 5.16. Alternatively, a more sensitive, but less specific finding is the presence of right atrial collapse during ventricular systole (atrial diastole).
Cardiac Arrest
POC cardiac echocardiography can be invaluable during cardiac arrest. Typical uses include evaluation for tamponade, hypovolemia, and suggestions of PE (clot, right ventricular dilation); detection of aortic dissection; monitoring for pacer capture and the adequacy of compressions; and most important, evaluation for cardiac activity in patients with pulseless electrical activity (PEA) and asystole. Studies have shown cardiac standstill during arrest to be 100% predictive of mortality.7 Furthermore, cardiac ultrasound has been used in place of a pulse check in pediatric populations because of the inherent difficulty of finding a pulse.8 Typical algorithms use cardiac ultrasound to evaluate PEA and asystolic rhythms.9 If cardiac standstill is present, further resuscitation is futile.7
Acute Heart Failure
Emergency physicians have been shown to be accurate in estimating left ventricular ejection fraction (LVEF).3 LVEF is most easily separated into three categories: reduced, normal, and hyperdynamic. Although echocardiographers often report actual percentages, we can think of normal LVEF as 55% to 75%, reduced as less than 55%, and hyperdynamic as greater than 75%. Some authors add a fourth category in which severely reduced LVEF is less than 30%. This distinction can be useful when discussing cardiac function with consultants.
Pulmonary Embolism
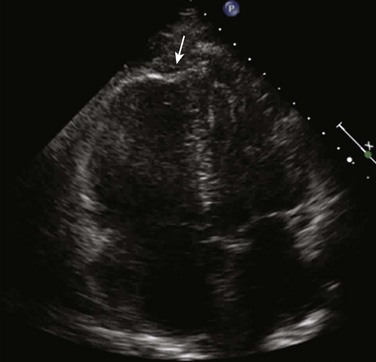
Although cardiac ultrasound cannot identify a pulmonary embolus,10 several findings are suggestive of this diagnosis. Right ventricular dysfunction and dilation are typically visualized in the apical four-chamber window. Right ventricular dilation has been described in reference to the relative areas of the right and left ventricles at end-diastole. A right-to-left ventricular area ratio of greater than 0.66 has been shown to be 85% specific for PE.11 Another finding is described as retained apical function in the setting of right ventricular free wall hypokinesis. This is called the McConnell sign and can be fairly specific for PE. McConnell et al. described this particular finding as being 94% specific for PE11 (Fig. 5.17). An additional finding in acute PE is flattening of the interventricular septum. This is seen in the parasternal short-axis view and is due to either volume or pressure overload of the right heart (Fig. 5.18).12
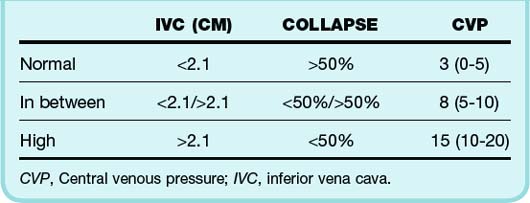
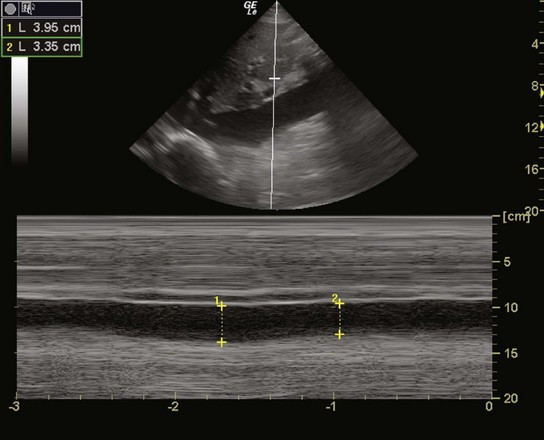
Volume Status
Additionally, a body of research has led to evaluation of the inferior vena cava as a surrogate marker for central venous pressure and thus volume status.13 The current recommendations are summarized in Table 5.1. The inferior vena cava should measured during both inspiration and expiration from the subcostal long-axis view as seen in Figure 5.19.
Blaivas M, Fox J. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside emergency department echocardiogram. Acad Emerg Med. 2001;8:616–621.
Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and the American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225–1230.
Mandavia D, Hoffner R, Mahaney K, et al. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38:377–382.
Moore C, Rose GA, Tayal VS, et al. Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med. 2002;9:186–193.
Perera P, Mailhot D, Riley D, et al. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically ill. Emerg Med Clin North Am. 2010;28:29–56.
1 Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and the American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225–1230.
2 Perera P, Mailhot D, Riley D, et al. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically ill. Emerg Med Clin North Am. 2010;28:29–56.
3 Moore C, Rose GA, Tayal VS, et al. Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med. 2002;9:186–193.
4 Jones AE, Tayal VS, Sullivan DM, et al. Randomized controlled trial of immediate vs. delayed goal-directed ultrasound to identify the etiology of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32:1703–1708.
5 Mandavia D, Hoffner R, Mahaney K, et al. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38:377–382.
6 Plummer D, Brunnette D, Asinger R, et al. Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992;21:709–712.
7 Blaivas M, Fox J. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside emergency department echocardiogram. Acad Emerg Med. 2001;8:616–621.
8 Tsung JW, Blaivas M. Feasibility of correlating the pulse check with focused point-of-care echocardiography during pediatric cardiac arrest: a case series. Resuscitation. 2008;77:264–269.
9 Breitkreutz R, Walcher F, Seeger F. Focused echocardiographic evaluation in resuscitation management: concept of an advanced life support–conformed algorithm. Crit Care Med. 2007;35:S150–S161.
10 Ladato J, Ward R, Lang R. Echocardiographic predictors of pulmonary embolism in patients referred for helical CT. Echocardiography. 2008;25:584–590.
11 McConnell MV, Solomon SD, Rayan ME, et al. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78:469–473.
12 Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
13 Jones AE, Tayal VS, Sullivan DM, et al. Randomized controlled trial of immediate vs. delayed goal-directed ultrasound to identify the etiology of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32:1703–1708.