30 Electroencephalography
The EEG is an important neurological tool, for three main reasons:
We suggest you review the amino acid transmitters in Chapter 8 before reading about drug therapy in the Clinical Panels.
Neurophysiological Basis of the EEG
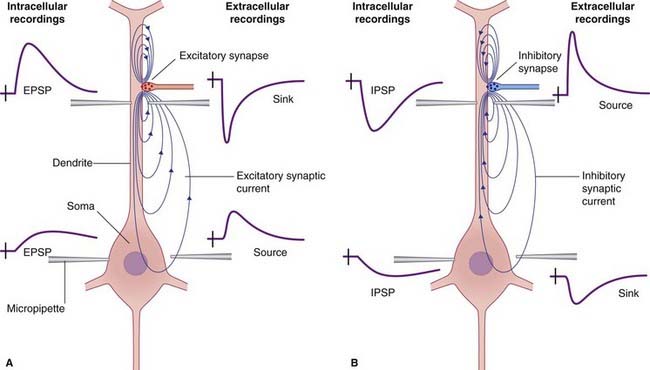
When small metallic disc electrodes are placed on the surface of the scalp, oscillating currents of 20–100 µV can be detected and are referred to as an electroencephalogram (EEG). Their origin is a direct consequence of the additive effect of groups of cortical pyramidal neurons being arranged in radial (outward-directed) columns. The columns relevant here are those beneath the surface of the cortical gyri. As the membrane potentials of these columns fluctuate, an electrical dipole (adjacent areas of opposite charge) develops. The dipole results in an electrical field potential as current flows through the adjacent extracellular space as well as intracellularly through the neurons (Figure 30.1). It is the extracellular component of this current that is recorded in the EEG and variations in both the strength and density of the current loops result in its characteristic sinusoidal waveform.
Technique
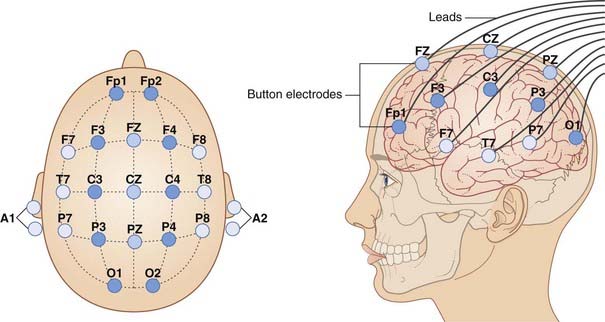
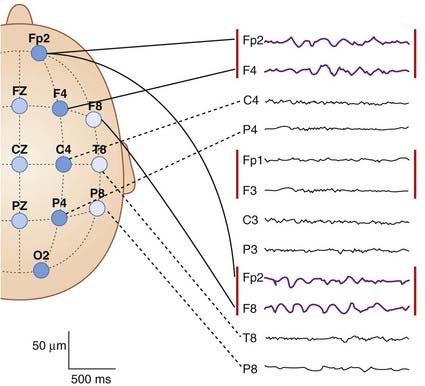
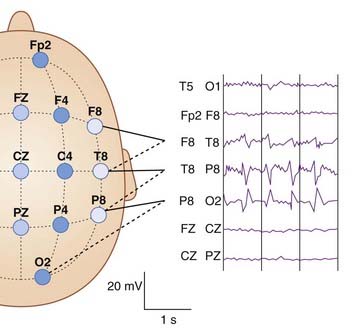
After careful preparation of the skin of the scalp to ensure good contact, electrodes are affixed in a placement that is in conformity with the 10–20 International System of Electrode Placement, when the scalp is divided into a grid in accordance with Figure 30.2.
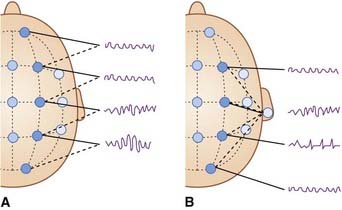
If varying pairs of electrodes are used, the montage (output) is termed bipolar (Figure 30.3A). If they have one recording site in common (auricle, or mastoid area), it is called referential (Figure 30.3B).
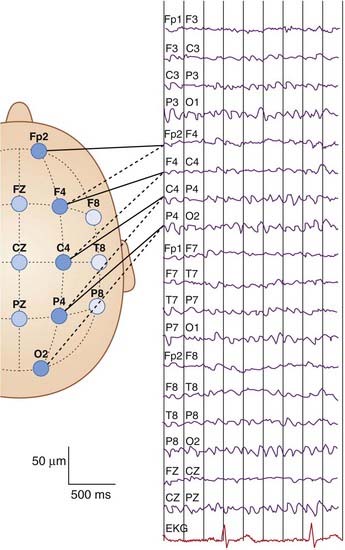
Figure 30.4 provides a complete set of normal tracings.
Types of Pattern
Normal EEG rhythms
Awake state EEG
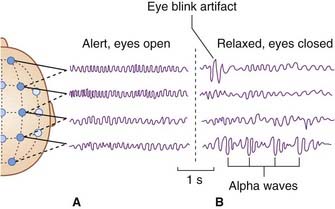
In the alert awake state (Figure 30.5A), the pattern is described as desynchronized because the waveforms are quite irregular. The background frequency is usually around 9.5 Hz. A beta frequency of more than 14 Hz may be superimposed over anterior head regions.
In a relaxed state with the eyes closed, rhythmic waveforms appear in the alpha frequency (8–14 Hz), notably over the parieto-occipital area (Figure 30.5B).
Normal sleep EEG
Glossary
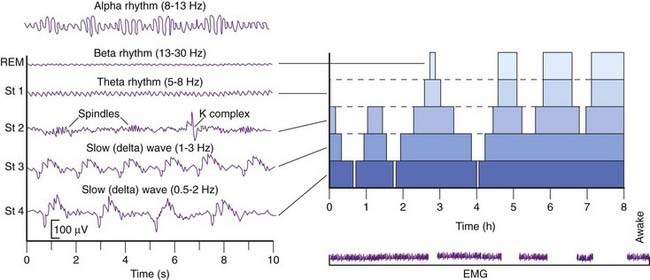
People normally pass through three to five sleep cycles per night. The sequence of events is summarized in Figure 30.5. Alpha rhythm becomes apparent (on occipital leads) during quiet rest with eyes closed.
By general agreement, sleep proper is associated with slow-wave patterns in the EEG. There is a rapid descent through stage 1, characterized by a steady theta rhythm, into stage 2, characterized by theta waves interrupted by sinusoidal waveforms called sleep spindles, and by occasional K complex spikes. Stage 3 is characterized by slow, delta waves – hence the term slow wave sleep for that stage (Figure 30.6).
As described in Chapter 27, thalamocortical projections pass through an inhibitory shell in the form of the thalamic reticular nucleus, with reciprocal connections to parent relay cells as shown in Figure 27.4. Burst firing excites the reticular nucleus, which in turn causes the relay neurons to become hyperpolarized by opening the GIRK potassium channels (Figure 8.11).
In the clinic, because of the brief time that an EEG is recorded, a patient does not often cycle through REM sleep patterns. It should be noted that in normal circumstances REM sleep almost never occurs during the first descent into sleep. Should it do so, the strange sleep disorder called narcolepsy should come to mind (Clinical Panel 30.1).
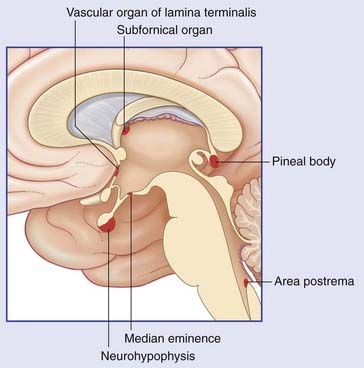
Clinical Panel 30.1 Narcolepsy
The key problem is a diminution of gray matter in the walls of the hypothalamus associated with scant production of the excitatory peptide orexin (hypocretin) by a group of neurons in the lateral hypothalamus. Orexin receptors are normally present on the histaminergic neurons of the tuberomammillary nucleus (TMN). As mentioned in Chapter 26, the TMN projects widely to the cerebral cortex and maintains the awake state by activating H1 receptors on cortical neurons. The drug modafinil is now a medication used to treat narcolepsy, perhaps by decreasing GABA-mediated neurotransmission. The current conventional approach is to reduce sleep attacks by means of noradrenergic drugs such as amphetamine in low dosage, and/or monoamine oxidase inhibitors; both of these prolong the action of norepinephrine released by the cerulean nucleus, and reduce REM sleep.
EEG activation procedures
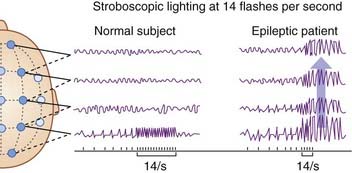
In order to check for susceptibility to seizures, a routine EEG includes a brief period of hyperventilation and another of photic stimulation using strobe (flickering) light at varying frequencies (Figure 30.7).
Abnormal EEG rhythms
Focal abnormalities without seizures
Focal slowing
Focal slowing, in the form of delta waves (Figure 30.8), indicates presence of a mass or lesion of some kind.
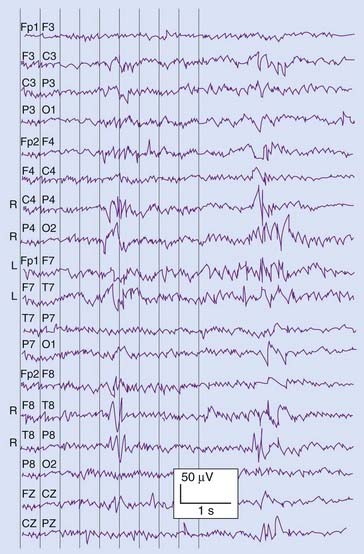
Focal spike or sharp wave discharges may show a patch of phase reversal between adjacent electrodes (Figure 30.9). In the frontal or parietal regon, this is suggestive of an ictal focus; in the occipital it is associated with visual impairment.
Phase reversal
Focal spike or sharp wave discharges are occasionally seen over localized areas of the cortex. Both appear as abrupt events, individual spikes lasting 80–100 ms and sharp waves 100–200 ms. Such discharges project to the surface with a negative polarity and the point of phase reversal between adjacent electrodes defines their EEG localization (Figure 30.9). In anterior temporal and frontal areas they may be indicative of an ictal focus, a term denoting a locus of origin of seizures. In the occipital region any correlation is usually with visual impairment.
Seizures
Clinical Panel 30.2 Seizures
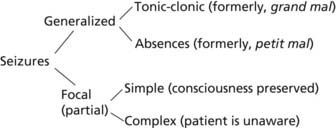
Seizures are categorized as follows:
Generalized seizures
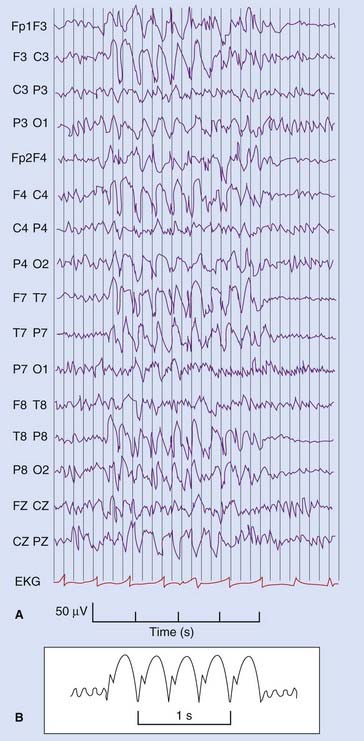
Generalized, tonic–clonic seizures (formerly known as grand mal seizures) are characterized by sudden onset of unconsciousness. The individual is ‘struck down’. The body stiffens, for up to a minute (tonic stage), and then exhibits jerky movements of all four limbs, and chewing movements of the mouth for about another minute (clonic stage). Usually, a third minute is spent in more relaxed unconsciousness. EEG recordings taken at the onset of this kind of ictus (attack) show simultaneous bilateral burst-firing all over the cortex (Figure CP 30.2.1).
In those at risk, hyperventilation, or photic stimulation by strobe lighting (Figure 30.7), can precipitate tonic-clonic attacks.
Absence seizures (formerly, petit mal) are characterized by a generalized, 3 Hz spike-and-wave activity (Figure CP 30.2.2). These seizures usually occur between the ages of 4 and 14.
Focal (partial) seizures
Simple focal seizures are almost always motor or sensory. Loci of origin are as shown in Table CP 30.2.1.
Benign rolandic epilepsy, a relatively common disorder in childhood, has an ictal focus of origin in front of or behind the fissure of Rolando (central sulcus). Motor attacks originate in front of the rolandic fissure and usually involve only the contralateral arm or leg or face, although some become jacksonian. Somatosensory attacks (Figure CP 30.2.3) originate behind the fissure and are described in Table CP 30.2.1.
Complex focal seizures are synonymous with temporal lobe epilepsy. They will be taken up in Chapter 34 following a description there of the relevant areas of the temporal lobe.
Drug therapy
Dichter MA. Emerging concepts in the pathogenesis of epilepsy and eleptogenesis. Arch Neurol. 2009;66:443-447.
Oliviero A, Della Marca G, Tonali PA, Pilato E, Saturno E, Dileone M, Versace V, Mennuni G, Di Lazzaro V. Functional involvement of the cerebral cortex in human narcolepsy. J Neurol. 2005;252:56-61.
Smith SJM. EEG in the diagnosis, classification, and management of patients with epilepsy. J Neurol Neurosurg Psychiatry. 2005;76(Suppl II):ii2-ii7.
Steriade M. Sleep, epilepsy and thalamic reticular nucleus. Trends Neurosci. 2005;28:317-324.
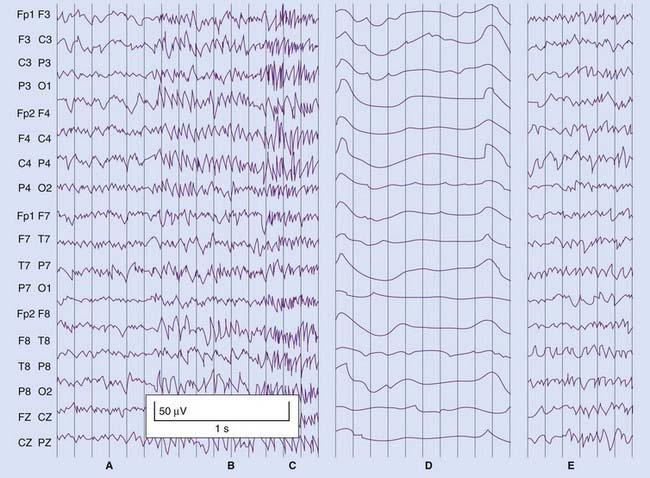
Figure CP 30.2.1 Characteristic ‘frenzied’ pattern of a tonic-clonic seizure.
(B) Generalized seizure pattern involving all electrode positions.
(C) In less than 1 second, the seizure pattern is ‘scribbled’ by generalized tonic muscle spasm.
(D) Immediate postictal period, with slow waveform pattern throughout.
| Motor | Movement of any part of the motor homunculus, sometimes with aphasia |
|---|---|
| Somatosensory | Contralateral nunbness/tingling of face, fingers or toes |
| Primary visual cortex | Flashes of light or patches of darkness in contralateral visual field |
| Visual association cortex | Twinkling-light images in contralateral visual field |
| Basal occipitotemporal junction | Formed visual images of people or places, sometimes accompanied by sounds |
| Superior temporal gyrus (unusual) | Tinnitus, sometimes garbled word sounds |
Binnie CD. Electroencephalography. In: Laidlaw J, Richins A, Oxley J, editors. A textbook of epilepsy. Edinburgh: Churchill Livingstone; 1988:236-306.
Grigg-Damberger M. Normal sleep: impact of age, circadian rhythms, and sleep debt. Continuum: Lifelong Learning in Neurology. 2007;13:31-84.
Nestler EJ, Hyman SE, Malenka RC. Sleep, arousal and attention. In: Molecular neuropharmacology: a foundation for clinical neuroscience. New York: McGraw-Hill; 2001:409-432.
Siegel JM. The neurobiology of sleep. Semin Neurol. 2009;29:277-296.
Smith PE. The bare essentials: epilepsy. Neurology in Practice. 2008;8:195-202.
Staunton H. Mammalian sleep. Naturwissenschaften. 2005;92:203-220.