Electrical and Lightning Injuries
Perspective
The first recorded death caused by electrical current from an artificial source was reported in 1879 when a carpenter in Lyons, France, inadvertently contacted a 250-V alternating-current generator.1 The first U.S. fatality occurred in 1881 when an inebriated man passed out on a similar generator in front of a crowd in Buffalo, New York.
In the United States, electrical burns account for 4 to 6.5% of all admissions to burn units and approximately 1000 fatalities per year.2 Occupational electrical incidents are uncommon but account for nearly 6% of all occupational fatalities annually.3 Children have a predisposition to injuries from low-voltage sources, such as electric cords, because of their limited mobility within a relatively confined environment. During adolescence, a more active exploration of the environment leads to more severe high-voltage injuries or death. At the time of presentation, documentation of injuries is important not only for the immediate resuscitation of the victim but also for medicolegal reasons. Many electrical injuries eventually involve litigation for negligence, product liability, or worker’s compensation.
Lightning Injury
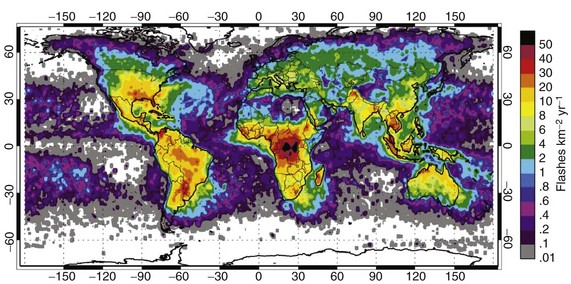
The incidence of injury and death from lightning is unknown because no agency requires the reporting of lightning injuries, and some victims do not seek treatment at the time of their injury. The incidence of lightning-related deaths in the United States has declined to an average of 39 people annually.4 Lightning is fatal in 1 of 10 lightning strike victims. In typical years, lightning kills more people in the United States than any storm phenomenon except floods, and it is consistently among the top four storm-related killers (Fig. 142-1). In 2009-2010, most of those killed in the United States were within 50 to 100 feet of safety, either seeking safe shelter too late or returning to their outdoor activities before the end of the storm.4 In developing countries, particularly those in the tropics, lightning is a much bigger risk both because it is more common and because agricultural, mining, and construction continue to be labor-intensive, resulting in high exposure to the workers.5 The lack of safe housing and metal vehicles expose entire families and schools to injury whenever a thunderstorm occurs.6
Principles of Disease
The exact pathophysiologic mechanism of electrical injury is not well understood because of the numerous variables that cannot be measured or controlled when an electrical current passes through tissue. With high voltage, most of the injury is thermal, and histologic studies reveal coagulation necrosis consistent with thermal injury.7,8 The theory of electroporation is that electrical charges insufficient to produce thermal damage cause protein configuration changes that threaten cell wall integrity and cellular function.9
The nature and severity of electrical burn injury are directly proportional to the current strength, resistance, and duration of current flow (Box 142-1).10 Factors that may determine the severity of an electrical injury are summarized in Box 142-2. Unfortunately, none of these can be used to predict or to explain the damage that any individual may suffer.
Resistance
Resistance is the tendency of a material to resist the flow of electrical current. It varies for a given tissue, depending on its moisture content, temperature, and other physical properties. The higher the resistance of a tissue to the flow of current, the greater the potential for transformation of electrical energy to thermal energy. Nerves, designed to carry electrical signals, and muscle and blood vessels, because of their high electrolyte and water content, have a low resistance and are good conductors. Bone, tendon, and fat, which all contain a large amount of inert matrix, have a high resistance and tend to heat and coagulate rather than to transmit current. The other tissues of the body are intermediate in resistance (Box 142-3).11
Skin is the primary resistor to the flow of current into the body. Skin on the inside of the arm or back of the hand has a resistance of approximately 30,000 Ω/cm2. Thick, hardened skin can have 20 to 70 times greater resistance (Table 142-1).8 This high resistance may result in a significant amount of energy being expended at the skin surface as the current burns its way through deep callus, resulting in greater thermal injury to the skin. As the duration of contact increases, however, the skin begins to blister and offer decreased resistance. A surge of current internally can cause extensive deep tissue destruction. Moisture also lowers resistance. Sweating can decrease the skin’s resistance to 2500 to 3000 Ω/cm2, and immersion in water causes a further reduction to 1200 to 1500 Ω/cm2.
Table 142-1
| TISSUE | RESISTANCE (Ω/cm2) |
| Mucous membranes | 100 |
| Vascular areas | |
| Volar arm, inner thigh | 300-10,000 |
| Wet skin | |
| Bathtub | 1200-1500 |
| Sweat | 2500 |
| Other skin | 10,000-40,000 |
| Sole of foot | 100,000-200,000 |
| Heavily calloused palm | 1-2 million |
Amperage
The physical effects vary with different amperages at 50 to 60 Hz, which is the AC frequency used in European countries and the United States (Table 142-2). A narrow range exists between the threshold of perception of current (0.2-0.4 mA) and let-go current (6-9 mA). Thoracic tetany can occur at levels just above the let-go current and result in respiratory arrest. Ventricular fibrillation may occur at an amperage of 60 to 120 mA. Although the 120-V household source usually causes minimal injury across dry skin, amperage delivered to the heart when the resistance of the skin is decreased by sweat or submersion in water can result in current sufficient to cause electrocution with cardiac arrest but without apparent external injury.
Table 142-2
Physical Effects of Different Amperage Levels at 50 to 60 Hz
| PHYSICAL EFFECT | CURRENT (mA) |
| Tingling sensation | 1-4 |
| Let-go current | |
| Children | 4 |
| Women | 7 |
| Men | 9 |
| Freezing to circuit | 10-20 |
| Respiratory arrest from thoracic muscle tetany | 20-50 |
| Ventricular fibrillation | 60-120 |
Pathway
Current density is the amount of current flow per area of tissue.10 As current density increases, any tendency to flow through the less resistant tissues is overcome. Eventually it flows through tissues indiscriminately, as if the body were a volume conductor, with the potential to destroy all tissues in the current’s path. Because the current is often concentrated at the source and ground contact points, current density and the degree of damage are greatest there. Nevertheless, extensive deep destruction of the tissues may exist between these sites with high-voltage injuries, and the surface damage is often only “the tip of the iceberg.” Damage to the internal structures of the body may be noncontiguous, with areas of normal-appearing tissue adjacent to burned tissue and with damage to structures at sites distant from the apparent contact points.
The pathway between contact points is a major determinant of the electrical field strength, which is the voltage per unit of length over which it is applied. For a given current, the shorter the distance between contact points, the greater the electrical field strength. Current from a 20,000-V power line passing from head to toe (approximately 2 m) results in an electrical field strength of 10,000 V/m. Approximately the same electrical field strength is created when “low”-voltage 120-V household current passes between two close contact points on the mouth of a child chewing on a power cord (120 V/0.01 m). Although the electrical field strengths are similar, there is a tremendous difference in the amount of at-risk tissue in the respective pathways.12,13
Although lightning is governed by the same physical laws as artificial electricity is, the rapid rise and decay of the energy complicate predictions of the extent of lightning injury more than with artificial electrical injury. The most important difference between lightning and high-voltage electrical injuries is the duration of exposure to the energy.14
Lightning is neither a direct current nor an alternating current but rather a unidirectional massive current impulse. The cloud-to-ground lightning impulse results from the breakdown of a large electrical field between a cloud and the ground that is measured in millions of volts. When connection is made with the ground, this voltage difference between the cloud and ground disappears, and a large current flows impulsively for a brief instant.14
Mathematical modeling of a lightning flow on the human body, substantiated in animal models, has included only direct strikes that account for only 3 to 5% of lightning injury to people.15,16 After a direct strike meets the body, current is transmitted internally for less than a millisecond before external “flashover” occurs.17 Although lightning current may flow internally for an instant and disrupt electrical systems, it seldom results in significant thermal injury or tissue destruction, and less than one third of lightning survivors have any signs of burns or skin damage. Muscle damage and myoglobinuria from lightning are rare. It is unknown whether the most serious manifestations of lightning injury, cardiac and respiratory arrest, vascular spasm, neurologic damage, and autonomic instability, result from induced electrical changes, current through highly conductive tissues, concussive injury, or other mechanisms.
Lightning tends to cause asystole rather than ventricular fibrillation. Although cardiac automaticity may reestablish a rhythm, the duration of the respiratory arrest may cause secondary deterioration of the rhythm to refractory ventricular fibrillation and asystole.14,18 Other injuries caused by blunt trauma or ischemia from vascular spasms, such as myocardial infarction and spinal artery syndromes, also occur.19–22
Mechanisms of Injury
The primary electrical injury is the burn. Secondary blunt trauma results from falls or being thrown from the electrical source by an intense muscle contraction or the explosive force that may occur with electric flashes from circuit box or transformer accidents. Electrical burns are classified into four different types (Box 142-4).
The most destructive indirect injury occurs when a victim becomes part of an electrical arc. An electrical arc is a current spark formed between two objects of differing potential that are not in contact with each other, usually a highly charged source and a ground. The temperature of an electrical arc is approximately 2500° C, and the electrical arc causes deep thermal burns at the point where it contacts the skin.12 With electrical arcs, burns may be caused by the heat of the arc, electrothermal heating due to current flow, or flames that result from the ignition of clothing.
Burns may occur from radiated thermal injury when an electrical explosion occurs, similar to gas explosions. Instead of becoming part of the arc, current may appear to jump the gap by splashing across a large part of the body. These splash burns are generally only partial thickness because the person did not become part of the arc itself.23
At the time of presentation it is often difficult to determine the mechanism of injury that caused an electrically injured patient’s burns. Electrothermal heating is the main cause of muscle damage and is seen almost exclusively in high-voltage accidents with prolonged (seconds) contact and current flow.23
The histologic change in muscle injury that results from direct contact with an electrical source is coagulation necrosis with shortening of the sarcomere.8,11 Muscle damage can be erratic, so areas of viable and nonviable muscle are often found in the same muscle group. Periosteal muscle damage may occur even though overlying muscle appears to be normal. Similar to muscle damage, serious vascular damage usually occurs only after a high-voltage accident.
Vascular damage is greatest in the media, predisposing to delayed hemorrhage when the vessel eventually ruptures.11 Intimal damage may result in either immediate or delayed thrombosis and vascular occlusion as edema and clots form on the damaged intimal surface of the vessel during a period of days. The injury is usually most severe in the small muscle branches, where blood flow is slower.24 This damage to small muscle arteries combined with mixed muscle viability that is not visible to gross inspection creates the illusion of progressive tissue necrosis. Veins, having more sluggish flow, are more prone to thrombosis than arteries are, and significant distal edema can result.
The hands, feet, and skull are the most common contact points. Histologic studies of the brain reveal focal petechial hemorrhages in the brainstem, cerebral edema, and widespread chromatolysis (the disintegration of chromophil bodies of neurons).11
Lightning Injury
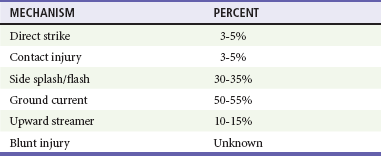
Lightning injury may occur by electrical mechanisms and by secondary concussive or blunt trauma.16,25 Whereas direct strike is most commonly described as the mechanism of injury, studies show that it accounts for a very small proportion of injuries and deaths (Table 142-3).
Table 142-3
Distribution of Lightning Injury Mechanisms
From Cooper MA, Holle RL: Mechanisms of lightning injury should affect lightning safety messages. Presented at the 3rd International Lightning Meteorology Conference, Orlando, Fla, April 2010.
Injury from contact occurs when the person is touching an object that is part of the pathway of lightning current, such as a tree, metal fence, indoor plumbing, or wiring. Side flash or splash occurs as a portion of lightning jumps from its primary strike object to a nearby person on its way to the ground.11,14,16,19,26 Step voltage, a difference in electrical potential between a person’s feet, may occur as lightning current spreads radially through the ground.14,16 A person who has one foot closer than the other to the strike point has a potential difference between the feet so that a portion of the lightning current flows through the legs and body rather than the ground. This ground current is a common killer of large livestock such as cattle and horses because of the greater distance between their hind legs and forelegs, with the heart lying in the pathway.
People may also be injured by upward streamers.25 Cloud-to-ground lightning approaches the earth as a downward stepped leader. As the leader approaches, the large electrical field induces opposite charges that surge through trees, buildings, people, and any other object near the thunderstorm. If one of these upward streamers connects with a downward leader, a completed lightning strike occurs. Individuals in the path of an upward streamer may be injured even in the absence of a completed lightning strike.
Ball lightning is a mobile, luminous, spheroidal, floating or bouncing ball that lasts a few seconds before suddenly vanishing or exploding. These glowing orbs are observed traveling down power lines and aisles of aircraft and even entering buildings through open doors.27 Although ball lightning has been described by multiple reputable observers for many years, the origin, chemical makeup, and physics are still a mystery.
Blunt injury from lightning can occur from at least two mechanisms. First, the person may be thrown a considerable distance by the sudden, massive contraction caused by current passing through the body. Second, a concussive injury caused by explosive or implosive force occurs as the lightning pathway is instantaneously superheated then rapidly cooled after the passage of the lightning.14 This concussive injury or barotrauma is associated with tympanic membrane rupture, contusions of various organs, and pneumothorax.28–33 Blunt or concussive injury can also accompany electrical injury.
Clinical Features
Patients with high-voltage injury commonly present with devastating burns. Patients with lightning injury and low-voltage injury may have little evidence of injury or alternatively may be in cardiopulmonary arrest.14 After the initial resuscitation of lightning and low-voltage injuries, other conditions may be identified. These patients may have significant residual morbidity from pain syndromes or central nervous system dysfunction.
Head and Neck
The head is a common point of contact for high-voltage injuries, and the patient may exhibit burns and neurologic damage. Cataracts develop in approximately 6% of patients with high-voltage injuries, especially whenever electrical injury occurs in the vicinity of the head.34,35 Although cataracts may be present initially or develop soon after the accident, they more typically appear months after the injury. Visual acuity and funduscopic examination should be performed at presentation. Hearing loss is much less common.36
Lightning Injury
Lightning strikes may cause skull fractures and cervical spine injury from associated blunt trauma.14,19,21 Tympanic membrane rupture is commonly found in lightning victims and may be secondary to the shock wave, a direct burn, or a basilar skull fracture. Although most patients recover without serious sequelae, disruption of the ossicles and mastoid, otorrhea, hemotympanum, perilymphatic fistulas, and permanent deafness may occur.28–31
Ocular injuries include corneal lesions, uveitis, iridocyclitis, hyphema, vitreous hemorrhage, optic atrophy, retinal detachment, and macular holes. Dilated, unreactive pupils are not a reliable indicator of death. As with electrical injuries, cataracts may develop in some patients.37,38
Cardiovascular System
Cardiac arrest, either from asystole or from ventricular fibrillation, is common in electrical accidents.39 Other electrocardiographic findings include sinus tachycardia, transient ST segment elevation, reversible QT segment prolongation, premature ventricular contractions, atrial fibrillation, and bundle branch block. Acute myocardial infarction is relatively rare.40
Lightning Injury
There are many proposed mechanisms of cardiac injury from lightning.14,39,41 Numerous dysrhythmias occur in the absence of cardiac arrest.13,14,39,41 Nonspecific ST-T wave segment changes and prolongation of the QT interval may occur, and serum levels of cardiac markers may be elevated. Hypertension is commonly present after lightning injury but usually resolves without treatment within a few hours.14
Skin
Other than cardiac arrest, the most devastating injuries are burns, which are most severe at the source and ground contact points. The most common sites of contact with the source are the hands and the skull. The most common areas of ground contact are the heels. A patient may have multiple source and ground contact points. Burns in severe electrical accidents often appear as painless, depressed, yellow-gray, punctate areas with central necrosis, or the areas may be mummified.11 High-voltage current may flow internally to create massive muscle damage. If contact is brief, minimal flow may have occurred, and the visible skin damage may represent nearly all of the damage. Prediction of the amount of underlying tissue damage from the amount of cutaneous involvement is not possible.
A peculiar type of burn associated with electrical injury is the “kissing burn,” which occurs at the flexor creases (Fig. 142-2).11 As the current causes flexion of the extremity, the skin of the flexor surfaces at the joints touches. Combined with the moist environment that often occurs at the flexor areas, the electrical current may arc across the flexor crease, causing arc burns on both flexor surfaces and extensive underlying tissue damage.

Figure 142-2 Kissing burn. (Courtesy Mary Ann Cooper, MD.)
The most common electrical injury seen in children younger than 4 years is the mouth burn that occurs from sucking on a household electrical extension cord. These burns usually represent local arc burns, may involve the orbicularis oris muscle, and are especially worrisome when the commissure is involved because of the likelihood of cosmetic deformity. A significant risk of delayed bleeding from the labial artery exists when the eschar separates. Damage to developing dentition and facial bones can occur, and referral to an oral surgeon familiar with electrical injuries is recommended.42
Lightning Injury
Deep burns occur in less than 5% of lightning injuries.14,18,43 Patients may exhibit one or more of the following four types of superficial burns or skin changes: linear, punctate, feathering, or thermal burns.9,14,18 Linear burns tend to occur in areas where sweat or water accumulates, such as under the arms or down the chest. These are superficial burns that appear to be caused by steam production from the flashover phenomenon. Punctate burns appear as multiple, small cigarette-like burns, often with a heavier central concentration in a rosette-like pattern. They range from a few millimeters to 1 cm in diameter and seldom require grafting. Feathering burns are not true burns because there is seldom significant damage to the skin.14 These transient lesions are rare but when present are pathognomonic for lightning injury (Fig. 142-3) and seldom require any therapy.14 Thermal burns occur if the clothing is ignited or may be caused by metal that the person is wearing or carrying during the flashover.14,23

Figure 142-3 Feathering burn. (Courtesy Mary Ann Cooper, MD.)
Extremities
Vascular damage from the electrical energy may become evident at any time.24 Neurovascular checks should be assessed frequently in all extremities. Because the arteries are a high-flow system, heat may be dissipated and cause little initial apparent damage but result in subsequent deterioration. In contrast, the veins are a low-flow system, allowing the heat energy to heat blood rapidly, with resulting thrombosis. Consequently, an extremity may initially appear edematous or ischemic; with severe injuries, the entire extremity may appear mummified when all tissue elements, including the arteries, experience coagulation necrosis.
Damage to the vessel wall at the time of injury may result in delayed thrombosis and hemorrhage, especially in the small arteries to muscle.24 These ongoing vascular changes can cause a partial-thickness burn to progress into a full-thickness burn as the vascular supply diminishes to the area. Progressive loss of muscle because of vascular ischemia downstream from damaged vessels may require repeated deep débridement.21
Nervous System
In high-voltage injuries, loss of consciousness is usually transient unless there is a significant concomitant head injury. Prolonged coma with eventual recovery also occurs. Patients may exhibit confusion, flat affect, and difficulty with short-term memory and concentration. Electrical injury to the central nervous system may cause a seizure, either as an isolated event or as part of a new-onset seizure disorder. Other possible causes of seizures, such as hypoxia and traumatic brain injury, should be considered. Neurologic symptoms may improve, but long-term disability is common. Even with low voltage, electrical injury may result in neurologic and psychological sequelae, many of which are nonspecific and delayed in onset.46–48
In high-voltage exposures, spinal cord injury may result from fractures or ligamentous disruption of the cervical, thoracic, or lumbar spine.49–52 Patients with immediate damage have symptoms of weakness, and paresthesias develop within hours of the insult. Lower extremity findings are more common than upper extremity findings. These patients have a good prognosis for partial or complete recovery. Delayed neurologic damage may be manifested days to months after the insult.50–52 Clinical presentations include ascending paralysis and transverse myelitis.49–52 Motor findings predominate. Sensory findings are also common and may be patchy and not match motor levels of impairment. Although recovery is reported, the prognosis is usually poor. Significant autonomic system dysfunction may complicate the postinjury recovery.51–53
Lightning Injury
Whereas high-energy electrical injury is primarily a burn injury, lightning is primarily a nervous system injury. On initial presentation, two thirds of seriously injured lightning patients have keraunoparalysis, which is a unique temporary paralysis secondary to lightning strike. It is characterized by lower and sometimes upper extremities that are blue, mottled, cold, and pulseless. These findings are secondary to vascular spasm and sympathetic nervous system instability.18,45 In general, this condition clears within a few hours, although some patients may be left with permanent paresis or paresthesias.
Paraplegia, intracranial hemorrhages, seizures, and electroencephalographic changes may occur after lightning injuries.45,51,52,54–56 Loss of consciousness for varying periods is common, and confusion and anterograde amnesia are almost universal findings. Peripheral nerve damage is also common, and recovery is usually poor. A lightning strike to the head can cause a visual cortex defect that results in complex visual hallucinations.57
Other Viscera
Lightning Injury
Pulmonary contusion, pneumothorax, and hemorrhage are seen with lightning injury.18,32,33 Blunt abdominal injuries occur rarely. None of the other intra-abdominal catastrophes commonly associated with high-voltage electrical injury, such as gallbladder necrosis or mesenteric thrombosis, is seen with lightning injury.
Other Low-Voltage Injuries
Conducted electrical weapons (such as the Taser and stun guns) are now commonly used by law enforcement. These devices deliver brief pulses of electrical energy that incapacitate the target subject. The majority of people subdued with these devices do not receive medical evaluation. When they present, the evaluation should focus on the patient’s organic or psychiatric conditions that prompted the officers’ use of the device, wounds or retained fragments caused by the probes, and secondary injuries associated with the severe muscle spasm and induced fall.58
Complications
Cardiac arrest generally occurs only at the initial presentation or as a final event after a long and complicated hospital course.39–41 Many of the complications are similar to those of thermal burns and crush injuries, including myoglobinuria, infection, and clostridial myositis.23,59 The incidence of acute myoglobinuric renal failure has decreased since the widespread adoption of aggressive alkalinized fluid resuscitation. Fasciotomies or carpal tunnel release may be necessary for the treatment of compartment syndromes.23,60 Tissue loss and major amputations are common with severe high-voltage injuries and result in the need for extensive rehabilitation.
Neurologic complications, such as loss of consciousness, peripheral nerve damage, and delayed spinal cord syndromes, may occur.49–52,61 Damage to the brain may result in a permanent seizure disorder. Long-term neuropsychiatric complications include depression, anxiety, inability to continue in the same profession, aggressive behavior, and suicide.47,48,51,52 Stress ulcers are the most common gastrointestinal complication after burn ileus.
Lightning Injury
Complications of lightning injury fall into three categories: (1) those that could be reasonably predicted from the presenting signs, such as hearing loss from tympanic membrane rupture or ossicular disruption, and paresthesias and paresis from neurologic damage; (2) long-term neurologic deficits and endocrine dysfunction similar to those associated with blunt head injury and chronic pain syndromes; and (3) iatrogenic complications that are secondary to overaggressive management.44,49–52,54–56,62
In the past, patients with lightning injuries were often treated similarly to patients with high-voltage electrical injuries. These injuries, however, are distinctly different.14,18 The acute treatment of lightning victims almost never requires massive fluid resuscitation, fasciotomies for compartment syndromes, alkalinization of the urine and diuresis, amputations, or repeated débridement of large areas.14,18,59
Differential Considerations
Lightning Injury
The differential diagnosis of lightning injury is more complex, especially if the incident is unobserved.14,18,63,64 It includes many of the causes of unconsciousness, paralysis, or disorientation of unclear etiology. Evidence of a thunderstorm or a witness to the lightning strike may not be available, particularly when victims are alone when they are injured. The presence of typical burn patterns, such as feathering, may be helpful.65 The most helpful sign is often the damage to the clothes as they are burst off or singed and have punctate holes, or brass zippers and grommets may show signs of melting with cuprification as the zinc component is evaporated.11,14,63,64
Management
Securing the Scene
During lightning incidents, nonhospital medical personnel are at risk of lightning injury if thunderstorms remain active in the area.14,66 Counter to folklore belief, lightning can strike the same place twice.14,66
Triage Considerations
Field evaluation of patients may involve triage of multiple victims. Traditional rules of mass casualty triage do not apply to lightning victims.14,66 Cardiorespiratory arrest is the major cause of death in lightning injuries.14,18 In the absence of cardiopulmonary arrest, victims rarely die in the field or afterward.14,66 Triage of lightning victims should concentrate on victims who appear to be in cardiorespiratory arrest and delay the evaluation of victims who are breathing as their survival is likely. Although intrinsic cardiac automaticity may ensue, the respiratory arrest caused by central nervous system injury often persists.14,18,66 If the victim is adequately ventilated during the interval, perfusion may be maintained.
Emergency Department
Cardiac arrest and airway compromise, including burns, are the most serious initial complications. For patients suffering circumferential burns to the chest that limit chest excursion or to the extremities causing compartment syndromes, fasciotomy and escharotomy may be necessary.23,60
The history obtained from bystanders and the nonhospital medical personnel regarding the type of electrical source, duration of contact, or environmental factors may be helpful. An electrical injury should be treated similarly to a crush injury rather than a thermal burn because of the large amount of tissue damage that is often present under normal-appearing skin. As a result, none of the formulae for intravenous fluids based on percentage of burned body surface area are reliable.14,66 Standard crystalloid resuscitation in anticipation of myoglobinuria should be maintained. Cardiac monitoring is indicated for severely injured patients and those who have the indications listed in Box 142-5.13,61,62 All patients with high-voltage injury and also patients with low-voltage injury and cardiorespiratory complaints should have an electrocardiogram (ECG) and cardiac biomarker determinations. Although electrocardiographic changes and dysrhythmias are common with electrical injuries, anesthesia and surgical procedures performed in the first 48 hours of care can be accomplished without cardiac complications.61
Most lightning victims behave as though they have had electroconvulsive therapy or a severe concussion, with confusion and amnesia for several days. If any altered mentation or neurologic deterioration occurs after an electrical injury, a computed tomography (CT) scan is indicated to assess for intracranial hemorrhage.14,18
Lightning victims who do not experience cardiopulmonary arrest at the time of the strike generally do well with supportive therapy. Patients who have cardiopulmonary arrest may have a poor prognosis, particularly if there is hypoxic brain damage.14,44,51,52,54–56
Ancillary Tests
Electrical Injury: Patients sustaining an electrical injury should receive cardiac monitoring in the emergency department (ED) and an ECG despite the source voltage.39–41,67–69 The following laboratory tests may be considered in patients with evidence of conductive injury or significant surface burns: complete blood count; electrolyte levels; serum myoglobin, blood urea nitrogen, and serum creatinine concentrations; and urinalysis. Patients with severe electrical injury or suspected intra-abdominal injury should also have pancreatic and hepatic enzymes measured and a coagulation profile obtained. Arterial blood gas analysis is indicated if the patient needs ventilatory intervention or alkalinization therapy. Patients should be evaluated for myoglobinuria, a common complication of high-voltage electrical injury. If new urine is pigmented or the dipstick examination of the urine is positive for blood and no red blood cells are seen on microscopic analysis, the patient should be assumed to have myoglobinuria.
Creatine kinase (CK) levels and isoenzyme analysis should be performed. Whereas high CK levels may be gross indicators of muscle injury, need for amputation, and length of hospitalization, CK elevations are not linear and the clinical value of a single level in the acute setting is not established. Less specific cardiac biomarkers should be interpreted with care in the diagnosis of myocardial infarction in the setting of electrical injury. The peak CK level is not indicative of myocardial damage in electrical injury because of the large amount of injured skeletal muscle cells, which can contain a 20 to 25% CK-MB fraction. CK-MB fractions, electrocardiographic changes, and angiography correlate poorly in acute myocardial infarction after electrical injury. Elevations in the more specific cardiac biomarkers (e.g., troponin) may indicate myocardial injury and should prompt further monitoring and evaluation.39,62,63
Radiographs of the spine should be obtained if spinal injury is clinically suspected or when patients cannot be assessed adequately because of altered mentation or the presence of other painful injuries. Angiography is not routinely indicated to plan débridement or amputations. CT or magnetic resonance imaging (MRI) may be useful in the evaluation of associated trauma and is essential for evaluation of possible intracranial injuries.14,44,51,52,54–56
Lightning Injury: In patients injured by lightning, an ECG should be obtained.39,41 Serum biomarkers for cardiac injury are indicated only in patients with chest pain, abnormal ECGs, or altered mentation. The severity or nature of the injuries may require other laboratory studies. Radiographic studies, particularly cranial CT or MRI evaluation, may be indicated, depending on the patient’s level of consciousness at presentation and throughout the evaluation and treatment.*
Specific Therapies
Burn Wound Care
Cutaneous burns should be dressed with antibiotic dressings, such as sulfadiazine silver. Electrical burns are especially prone to tetanus, and patients should receive tetanus toxoid and tetanus immune globulin on the basis of their immunization history. Prophylactic administration of high-dose penicillin to prevent clostridial myonecrosis is controversial.23,59
Extremity Injuries
Management of electrical injuries of the extremities entails surgical management, which includes early fasciotomy, carpal tunnel release, or amputation of an obviously nonviable extremity. Extremities should be splinted in a functional position to minimize edema and contracture formation.23,60
Disposition
Admission
Indications for admission for electrocardiographic monitoring are listed in Box 142-5.13,61,62 In general, when truncal conduction is suspected, the patient should be admitted for 12 to 24 hours of cardiac monitoring. Most patients with significant electrical burns should be stabilized and transferred to a regional burn center for burn care and extensive occupational and physical rehabilitation.
Outpatient Management
Asymptomatic patients with normal physical examination findings after low-voltage exposure can be reassured and discharged without any ancillary tests being performed.47 Patients with cutaneous burns or mild persistent symptoms can be discharged if they have a normal ECG and no urinary heme pigment. Outpatient referral should be provided in the event that current symptoms persist or new symptoms develop.
Electrical injury during pregnancy from low-voltage sources may result in fetal demise. A prospective cohort study of electric shock in pregnancy suggested that electric shock usually does not pose a major fetal risk.13,69 Nevertheless, obstetric consultation is advisable for all pregnant patients reporting electrical injury, regardless of symptoms at the time of presentation. Placental abruption, the most common cause of fetal death after blunt trauma, may result from even minor trauma, such as may be associated with electrical injuries. Patients in the last half of pregnancy should receive fetal monitoring if there is even minor blunt trauma and be considered high-risk patients for the remainder of their pregnancy.13 First-trimester patients should be informed of the remote risk of spontaneous abortion and, if no other indications for admission exist, may be discharged with instructions for threatened miscarriage and close obstetric follow-up evaluation. The prognosis for fetal survival after lightning strike is most dependent on the extent of the mother’s injuries. Fetal demise occurs in 50% of cases.71
Pediatric patients with oral burns may be safely discharged if close adult care is ensured.42 There is no evidence that an isolated oral burn correlates with cardiac injury or myoglobinuria. In general, these patients require surgical and dental consultation for oral splinting, eventual débridement, and occasionally reconstructive surgery. After appropriate consultation, if hospitalization is not deemed necessary, the child’s parents should be warned about the possibility of delayed hemorrhage and receive instructions to apply direct pressure by pinching the bleeding site and to return immediately to the ED.
Lightning Injuries
Most lightning survivors who appear well can be safely discharged. In reality, many survivors never seek emergency care, and overall mortality is only about 10%.14,18,72 Many of the more severe signs of lightning injuries, such as lower extremity paralysis and mottling, confusion, and amnesia, resolve with time.14,18 Spinal cord and intracranial processes should be excluded.
References
1. Jex-Blake, A. The Gulstonian lectures on death from electricity in the late nineteenth century. Med Instrum. 1975;9:267.
2. Lee, R. Injury by electrical forces: Pathophysiology, manifestations, and management. Curr Probl Surg. 1997;34:677.
3. Fordyce, T. Thermal burn and electrical injuries among electric utility workers, 1995-2004. Burns. 2007;33:209.
4. NOAA, National Weather Service, Office of Climate, Water, and Weather Services. Weather fatalities. www.nws.noaa.gov/om/hazstats.shtml.
5. NOAA, National Weather Service, Office of Climate, Water, and Weather Services. Lightning safety. www.lightningsafety.noaa.gov.
6. Cooper, MA, Ab Kadir, MZA. Lightning injury continues to be a public health threat internationally. www.vaisala.com/Vaisala%20Documents/Scientific%20papers/5.Cooper,%20Zainal.pdf.
7. Childbert, M, et al. Measure of tissue resistivity in experimental electric burns. J Trauma. 1985;25:209.
8. Puschel, K, Brinkman, B, Lieske, K. Ultrastructural alteration of skeletal muscles after electrical shock. Am J Forensic Med Pathol. 1985;6:246.
9. Lee, R, et al. Role of cell membrane rupture in the pathogenesis of electrical trauma. J Surg Res. 1998;44:709.
10. Barkana, BD, Gupta, N, Hmurcik, LV. Two case reports: Electrothermal (aka contact) burns and the effects of current density, application time and skin resistance. Burns. 2010;36:e91.
11. Wright, RK, Gantner, GE. Electrical injuries and lightning. In: Froede RC, ed. Handbook of Forensic Pathology. Northfield, Ill: College of American Pathologists, 1990.
12. Capelli-Schellpfeffer, M, et al. Advances in the evaluation and treatment of electrical and thermal injury emergencies. IEEE Trans Ind Appl. 1995;31:1147.
13. Fish, R. Electric injury: Part III. Cardiac monitoring indications, the pregnant patient, and lightning. J Emerg Med. 2000;18:181.
14. Cooper, MA, Andrews, CJ, Holle, RL, Blumenthal, R. Lightning injuries. In Auerbach PS, ed.: Wilderness Medicine, 6th ed, Philadelphia: Elsevier/Mosby, 2012.
15. Ishikawa, T, et al. Experimental study on the lethal threshold value of multiple successive voltage impulses to rabbits simulating multi-stroke lightning flash. Int J Biometeorol. 1986;29:157.
16. Cooper, MA, Holle, RL. Mechanisms of lightning injury should affect lightning safety Messages. www.vaisala.com/Vaisala%20Documents/Scientific%20papers/11.Cooper,%20Holle.pdf.
17. Ohashi, M, Kitagawa, N, Ishikawa, T. Lightning injury caused by discharges accompanying flashover: A clinical and experimental study of death and survival. Burns. 1986;12:496.
18. Cooper, MA. Lightning injuries: Prognostic signs for death. Ann Emerg Med. 1980;9:134.
19. Woods, J. Spinal atrophic paralysis following lightning stroke. S Afr Med J. 1952;26:92.
20. Buechner, H, Rothbaum, J. Lightning stroke injury: A report of multiple casualties from a single lightning bolt. Mil Med. 1961;126:775.
21. Leys, K. Spinal atrophic paralysis case following lightning stroke. Edinburgh Med J. 1942;49:657.
22. Zack, F, Hammer, U. Myocardial injury due to lightning. Int J Legal Med. 1997;110:326–328.
23. ten Duis, H. Acute electrical burns. Semin Neurol. 1995;15:381.
24. Hunt, J, et al. Vascular lesions in acute electrical injuries. J Trauma. 1974;14:461.
25. Cooper, MA. A fifth mechanism of lightning injury. Acad Emerg Med. 2002;9:172.
26. Arden, G, et al. Lightning accident at Ascot. BMJ. 1956;1:1453.
27. Fox, MR, Gubler, C. Struck dysphagic. Gastroenterology. 2009;137:9.
28. Offiah, C, et al. Lightning strike: A rare cause of bilateral ossicular disruption. Am J Neuroradiol. 2007;28:974.
29. Sun, G, et al. Bilateral perilymphatic fistulas from a lightning strike: A case report. Laryngoscope. 2006;116:1039.
30. Glunci , I, Roje, Z, Glunci
, I, Roje, Z, Glunci , V, Poljak, K. Ear injuries caused by lightning: Report of 18 cases. J Larnygol Otol. 2001;115:4.
, V, Poljak, K. Ear injuries caused by lightning: Report of 18 cases. J Larnygol Otol. 2001;115:4.
31. Wright JW: Acoustic and vestibular defects in lightning survivors. Presented at the meeting of the Middle Section of the American Laryngological, Rhinological and Otological Society, Kansas City, Mo, January 19, 1974.
32. Soltermann, B, Frutiger, A. Lightning injury with lung bleeding in a tracheotomized patient. Chest. 1991;99:240.
33. Halldorsson, A, Couch, MH. Pneumomediastinum caused by a lightning strike. J Trauma. 2004;57:196.
34. Benlier, E, et al. Isolated uveitis: A rare complication of electrical injury. J Burn Care Res. 2008;29:856.
35. Lakosha, H, Tremblay, F, De Becker, I. High-voltage electrical trauma to the eye. Can J Ophthalmol. 2009;44:605.
36. Liew, L, Morrison, G. Bilateral hearing loss following electrocution. J Laryngol Otol. 2006;120:65.
37. Cazabon, S, Dabbs, TR. Lightning-induced cataract. Eye (Lond). 2000;14(Pt 6):903.
38. Dinakaran, S, Desai, SP, Elsom, DM. Ophthalmic manifestations of lightning strikes. Surv Ophthalmol. 2002;47:292.
39. Cooper, MA, Holle, R, Andrews, C. Electrical current and lightning injury. In: Field J, ed. The Textbook of Emergency Cardiovascular Care and CPR. Philadelphia: Lippincott Williams & Wilkins; 2009:498–511.
40. Celebi, A, et al. Myocardial infarction after an electric shock: A rare complication. Cardiol J. 2009;16:362.
41. Johnson, SA, Cooper, MA. Cardiopulmonary resuscitation and early management of the lightning strike victim. In: Ornato JP, Peberdy MA, eds. Cardiopulmonary Resuscitation. Totowa, NJ: Humana Press, 2005.
42. Alexander, W. Composite dysplasia of a single tooth as a result of electrical burn. J Am Dent Assoc. 1961;69:589.
43. Bartholome, C, Jacoby, W, Ramchand, S. Cutaneous manifestations of lightning injury. Arch Dermatol. 1975;111:1466.
44. Cherington, M. Neurologic manifestations of lightning strikes. Neurology. 2003;60:182.
45. ten Duis, H, Klasen, H, Reenalda, PE. Keraunoparalysis, a “specific” lightning injury. Burns. 1985;12:54.
46. Singerman, J, Gomez, M, Fish, JS. Long-term sequelae of low-voltage electrical injury. J Burn Care Res. 2008;29:773.
47. Ramati, A, et al. Alteration in functional brain systems after electrical injury. J Neurotrauma. 2009;26:1815.
48. Ramati, A, et al. Prevalence of psychiatric morbidity following electrical injury and its effects on cognitive functioning. Gen Hosp Psychiatry. 2009;31:360.
49. Levine, N, et al. Spinal cord injury following electrical accidents: Case reports. J Trauma. 1975;15:459.
50. Erkin, G, et al. Delayed cervical spinal cord injury after high voltage electrical injury: A case report. J Burn Care Res. 2007;28:905.
51. Cherington, M. Central nervous system complications of lightning and electrical injuries. Semin Neurol. 1995;15:233.
52. Cherington, M. Neurorehabilitation of the multifaceted and complicated neurologic problems associated with lightning and electrical injuries. Neurorehabilitation. 2005;20:1.
53. Kanjwal, K, et al. Postural orthostatic tachycardia syndrome: A rare complication following electrical injury. Pacing Clin Electrophysiol. 2010;33:e59.
54. Baker, R. Paraplegia as a result of lightning injury. BMJ. 1978;2:1464.
55. Cherington, M. Spectrum of neurologic complications of lightning injuries. Neurorehabilitation. 2005;20:3.
56. Cherington, M, Yarnell, P, Lammereste, D. Lightning strikes: Nature of neurological damage in patients evaluated in hospital emergency departments. Ann Emerg Med. 1992;21:575.
57. Kleiter, I, et al. A lightning strike to the head causing a visual cortex defect with simple and complex visual hallucination. J Neurol Neurosurg Psychiatry. 2007;78:423.
58. Strote, J, et al. Conducted electrical weapon use by law enforcement: An evaluation of safety and injury. J Trauma. 2010;68:1239.
59. Yost, J, Holmes, F. Myoglobinuria following lightning stroke. JAMA. 1974;228:1147.
60. Pannucci, CJ, et al. Early fasciotomy in electrically injured patients as a marker for injury severity and deep venous thrombosis risk: An analysis of the National Burn Repository. J Burn Care Res. 2010;31:882.
61. Purdue, G, Hunt, J. Electrocardiographic monitoring after electrical injury: Necessity or luxury? J Trauma. 1986;26:166.
62. Orbak, Z, Kara, IS. Unusual complication in a child with lightning strike: Cerebral salt wasting. Childs Nerv Syst. 2010;22:1125.
63. Blumenthal, R. “When thunder roars—go indoors!” Lightning autopsy guidelines. S Afr Med J. 2006;96:38.
64. Wetli, CV. Keraunopathology—an analysis of 45 fatalities. Am J Forensic Med Pathol. 1996;17:89.
65. Cherington, M, Olson, S, Yarnell, PR. Lightning and Lichtenberg figures. Injury. 2003;34:367.
66. Cooper, MA. Myths, miracles, and mirages. Semin Neurol. 1995;15:358.
67. Rivera, J, et al. Severe stunned myocardium after lightning strike. Crit Care Med. 2007;35:280.
68. Garcia, C, et al. Electrical injuries in a pediatric emergency department. Ann Emerg Med. 1995;26:604.
69. Einarson, A, et al. Accidental electric shock in pregnancy: A prospective cohort study. Am J Obstet Gynecol. 1997;176:678.
70. Cherington, M, Yarnell, P, Hallmark, D. MRI in lightning encephalopathy. Neurology. 1993;43:1437.
71. Gutierrez, J, et al. Lightning injuries in a pregnant woman: A case report and review of the literature. Burns. 2005;31:1045.
72. Cherington M, et al: Closing the gap on the actual numbers of lightning casualties and deaths. American Meteorological Society 11th Conference on Applied Climatology, Dallas, Texas, January 10-15, 1999.