Elbow
The elbow’s primary role in the upper limb complex is to help an individual position his or her hand in the appropriate location to perform its function. Once the shoulder has positioned the hand in a gross fashion, the elbow allows for adjustments in height and length of the limb, allowing one to position the hand correctly. In addition, the forearm rotates, in part at the elbow, to place the hand in the most effective position to perform its function.
Applied Anatomy
The elbow consists of a complex set of joints that require careful assessment for proper treatment. The treatment must be geared to the pathology of the condition, because the joint responds poorly to trauma, harsh treatment, or incorrect treatment.
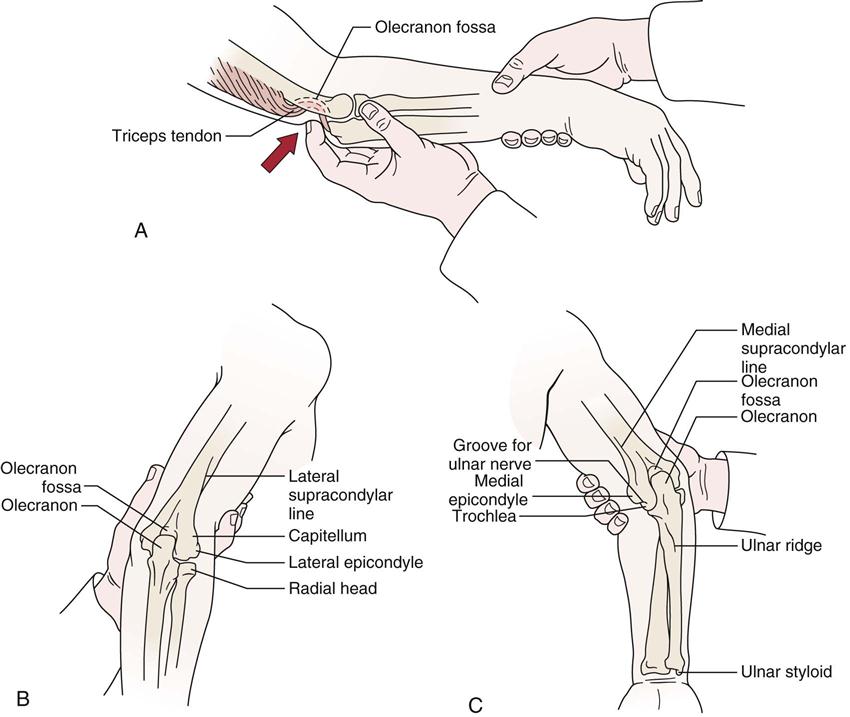
Because they are closely related, the joints of the elbow complex make up a compound synovial joint with injury to any one part affecting the other components as well (Figure 6-1). In addition, the ulnar and humeral articulations “fit” together rather intimately, which does not allow much “give” as compensation when an injury occurs. Thus, this joint often does not respond well to trauma. The elbow articulations are made up of the ulnohumeral joint and the radiohumeral joint. In addition, the complexity and intricate relation of the elbow articulations are further increased by the superior radioulnar joint, which has continuity with the elbow articulations. These three joints make up the cubital articulations. The capsule and joint cavity are continuous for all three joints. The combination of these joints allows 2° of freedom at the elbow. The trochlear joint allows 1° of freedom (flexion-extension), and the radiohumeral and superior radioulnar joints allow the other degree of freedom (rotation).
The ulnohumeral or trochlear joint (see Figure 6-1) is found between the trochlea of the humerus and the trochlear notch of the ulna and is classified as a uniaxial hinge joint. The bones of this joint are shaped so that the axis of movement is not horizontal but instead passes downward and medially, going through an arc of movement. This position leads to the carrying angle at the elbow (Figure 6-2). The resting position of this joint is with the elbow flexed to 70° and the forearm supinated 10°. The neutral position (0°) is midway between supination and pronation in the thumb-up position (Figure 6-3). The capsular pattern is flexion more limited than extension, and the close packed position is extension with the forearm in supination. On full extension, the medial part of the olecranon process is not in contact with the trochlea; on full flexion, the lateral part of the olecranon process is not in contact with the trochlea. This change allows the side-to-side joint play movement necessary for supination and pronation. A small amount of rotation occurs at this joint. In early flexion, 5° of medial rotation occurs; in late flexion, 5° of lateral rotation occurs.

The radiohumeral joint is a uniaxial hinge joint between the capitulum of the humerus and the head of the radius (see Figure 6-1). The resting position is with the elbow fully extended and the forearm fully supinated. The close packed position of the joint is with the elbow flexed to 90° and the forearm supinated 5°. As with the trochlear joint, the capsular pattern is flexion more limited than extension.
The ulnohumeral and radiohumeral joints are supported medially by the ulnar collateral ligament, a fan-shaped structure, and laterally by the radial collateral ligament, a cordlike structure (Figure 6-4).1 These ligaments, along with the ulnohumeral articulation, are the primary restraints to instability in the elbow.2 The lateral (radial) collateral ligament is the primary restraint to posterolateral instability (most common instability), whereas the medial (ulnar) collateral ligament is the primary restraint to valgus instability.2 The ulnar collateral ligament has three parts, which along with the flexor carpi ulnaris muscle form the cubital tunnel through which passes the ulnar nerve (see Figure 6-4). Any injury or blow to the area or injury that increases the carrying angle puts an abnormal stress on the nerve as it passes through the tunnel. This can lead to problems such as tardy ulnar palsy, the symptoms of which can occur many years after the original injury and may be caused by the “double crush” phenomena of a cubital tunnel problem combined with a cervical spine problem.
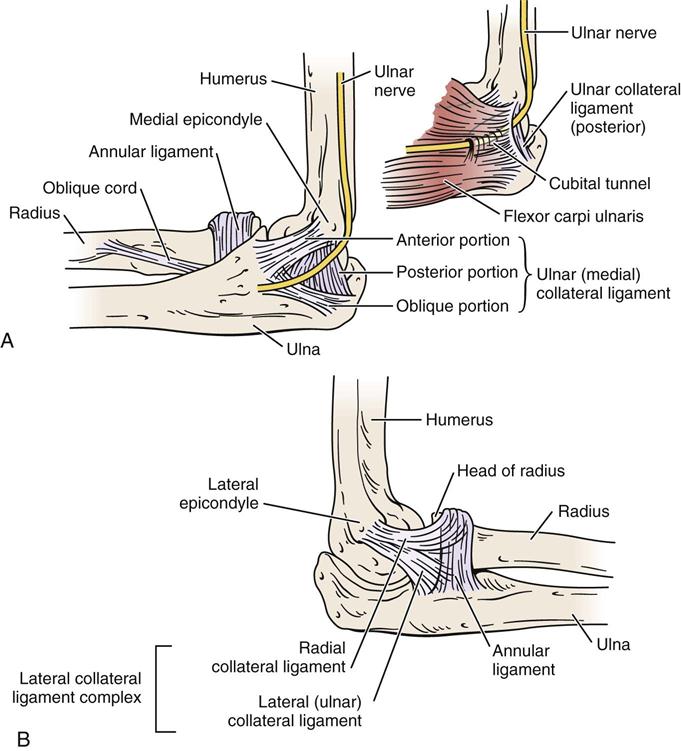
A, Ligaments on medial side of elbow. Note the passage of the ulnar nerve through the cubital tunnel. B, Ligaments on the lateral side of elbow.
The superior radioulnar joint is a uniaxial pivot joint. The head of the radius is held in proper relation to the ulna and humerus by the annular ligament (see Figures 6-1 and 6-4), which makes up four fifths of the joint.3 The resting position of this joint is supination of 35° and elbow flexion of 70°. The close packed position is supination of 5°. The capsular pattern of this joint is equal limitation of supination and pronation.
The three elbow articulations are innervated by branches from the musculocutaneous, median, ulnar, and radial nerves. The middle radioulnar articulation is not a true joint but is made up of the radius and ulna and the interosseous membrane between the two bones. The interosseous membrane is tense only midway between supination and pronation (neutral position). Although this “joint” is not part of the elbow joint complex, it is affected by injury to the elbow joints; conversely, injury to this area can affect the mechanics of the elbow articulations. The interosseous membrane prevents proximal displacement of the radius on the ulna. The displacement is most likely to occur with pushing movements. The oblique cord connects the radius and ulna, running from the lateral side of the ulnar tuberosity to the radius slightly below the radial tuberosity. Its fibers run at right angles to those of the interosseous membrane (see Figure 6-1). The cord assists in preventing displacement of the radius on the ulna, especially during movements involving pulling.
Patient History
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. How old is the patient? What is the patient’s occupation? Tennis elbow (lateral epicondylitis) problems usually occur in persons 35 years of age or older and in those who use a great deal of wrist flexion and extension in their occupations or activities, requiring wrist stabilization in slight extension (functional position). If the patient is a child who complains of pain in the elbow and lacks supination on examination, the examiner could suspect a dislocation of the head of the radius. This type of injury is often seen in young children. A parent may give the child a sharp “come-along” tug on the arm, or the child may trip while the parent is holding the hand, dislocating the head of the radius. Between the ages of 15 and 20, osteochondritis dissecans may be found.4
2. What was the mechanism of injury? Did the patient experience a fall on out-stretched hand (FOOSH) injury or on the tip of the elbow? Catching oneself from falling (Figure 6-5) or repetitive stress in sports (e.g., throwing) can create a severe valgus force to the elbow causing a medial side traction injury (e.g., sprain of the medial collateral ligament) and a lateral side compression injury. This can lead to injury at the radiohumeral joint, abnormal stress at the medial epicondyle (“little leaguer’s elbow”—if from repetitive stress from throwing), and osteochondral damage either on the olecranon process or olecranon fossa. Were any repetitive activities involved? Does the patient’s job involve any repetitive activities? Did the patient perform any unusual activities in the previous week? Did the patient feel a “pop” when throwing or doing other activity? If the pop was followed by pain and swelling on the medial side of the elbow, it may indicate an ulnar collateral ligament sprain.5 A centralized “pop” and weakness of elbow flexion may be the result of a distal biceps rupture. Such questions help determine the structure injured and the degree of injury.
5. Are there any activities that increase or decrease the pain? Does pulling (traction), twisting (torque), or pushing (compression) alter the pain? For example, writing, twisting motions of the arm (e.g., turning key, opening door), ironing, gripping, carrying, and leaning on forearm all stress the elbow.6 Such questions may indicate the tissues being stressed or the tissues injured.
7. Is there any indication of deformity, bruising (Figure 6-6), wasting, or muscle spasm?
11. Does the patient complain of any abnormal nerve distribution pain? The examiner should note the presence and location of any tingling or numbness for reference when checking dermatomes and peripheral nerve distribution later in the examination. Snapping on the medial side may indicate recurrent dislocation of the ulnar nerve or the medial head of the triceps dislocating over the medial epicondyle.4
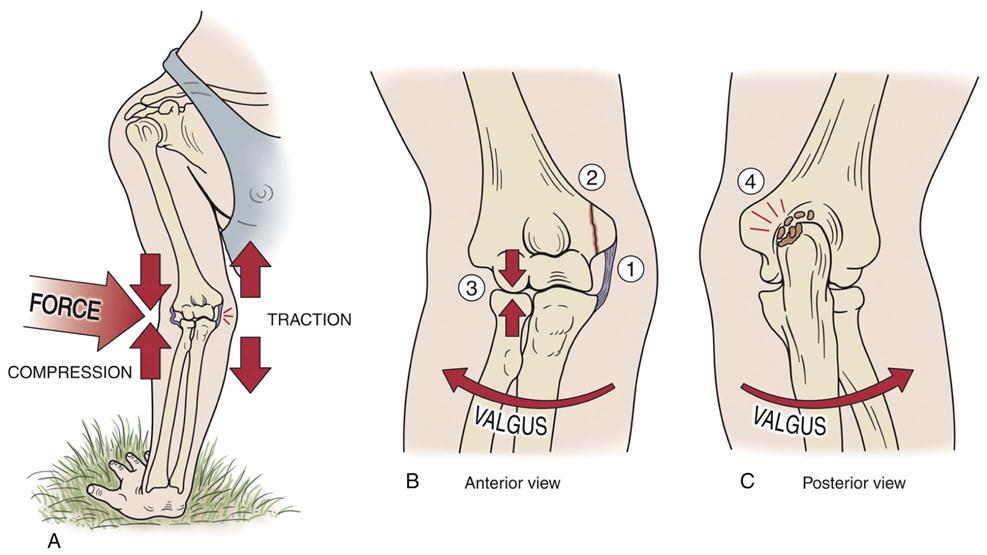
(A) Mechanism of injury. (B) Anterior view. (C) Posterior view. Injury may lead to 1) stretching of medial collateral ligament, 2) stress on epicondylar growth plate (pitcher’s or little leaguer’s elbow), 3) compression at radiohumeral joint, or 4) compression of the olecranon in the fossa, which may lead to osteophyte and loose body formation.
Observation
The patient must be suitably undressed so that both arms are exposed to allow the examiner to compare the two sides. If the history indicates an insidious onset of elbow problems, the examiner should take the time to observe full body posture, especially the neck and shoulder areas, for possible referral of symptoms.
The examiner first places the patient’s arm in the anatomical position to determine whether there is a normal carrying angle7 (see Figure 6-2). It is the angle formed by the long axis of the humerus and the long axis of the ulna and is most evident when the elbow is straight and the forearm is fully supinated (Figure 6-7). In the adult, this would be a slight valgus deviation between the humerus and the ulna when the forearm is supinated and the elbow is extended. In males, the normal carrying angle is 5° to 10°; in females, it is 10° to 15°. If the carrying angle is more than 15°, it is called cubitus valgus; if it is less than 5° to 10°, it is called cubitus varus (Figure 6-8). Because of the shape of the humeral condyles that articulate with the radius and ulna, the carrying angle changes linearly depending on the degree of extension or flexion. Cubitus valgus is greatest in extension. The angle decreases as the elbow flexes, reaching varus in full flexion.8 If there has been a fracture or epiphyseal injury to the distal humerus and a cubitus varus results, a gun stock deformity may occur in full extension (Figure 6-9, see Figure 6-8).

The carrying angle may be determined by noting the angle of intersection between a line connecting midpoints in the distal humerus and a line connecting midpoints in the proximal ulna.
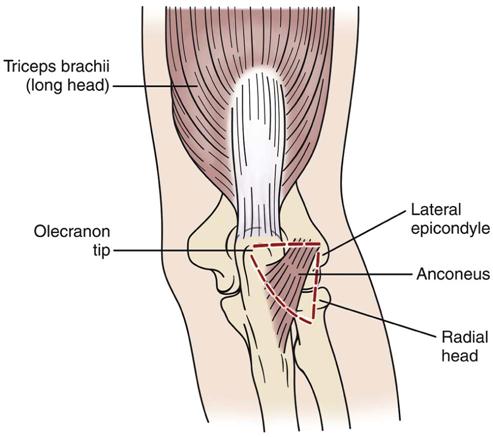
If swelling exists, all three joints of the elbow complex are affected because they have a common capsule. Joint swelling is often most evident in the triangular space between the radial head, tip of olecranon, and lateral epicondyle (Figure 6-10). Swelling resulting from olecranon bursitis (student’s elbow) is more discrete, being more sharply demarcated as a “goose egg” over the olecranon process (Figure 6-11). With swelling, the joint would be held in its resting position, with the elbow held in approximately 70° of flexion, because it is in the resting position that the joint has maximum volume.
The examiner should look for normal bony and soft-tissue contours anteriorly and posteriorly. Often, athletes (such as, pitchers, other throwers, and rodeo riders) have a much larger forearm because of muscle and bone hypertrophy on the dominant side.
The examiner should note whether the patient can assume the normal position of function of the elbow (Figure 6-12). A normal functional position is 90° of flexion with the forearm midway between supination and pronation.9 The forearm may also be considered to be in a functional position when slightly pronated, as in writing. From this position, forward flexion of the shoulder along with slightly more elbow flexion (up to 120°) enables the person to bring food to the mouth; supination of the forearm decreases the amount of shoulder flexion necessary to accomplish this. At 90° of elbow flexion, the olecranon process of the ulna and the medial and lateral epicondyles of the humerus normally form an isosceles triangle (Figure 6-13). When the arm is fully extended, the three points normally form a straight line.10 The isosceles triangle is sometimes called the triangle sign. If there is a fracture, dislocation, or degeneration leading to loss of bone or cartilage, the distance between the apex and the base decreases and the isosceles triangle no longer exists. The triangle can be measured on x-ray films.8
Examination
If the history indicates an insidious onset of elbow symptoms, and if the patient has complained of weakness and pain, the examiner may consider performing an examination of the cervical spine, which includes the upper limb peripheral joint scanning examination and myotome testing. Because of the potential referral of symptoms from the cervical spine and the necessity of differentiating nerve root symptoms from peripheral nerve lesions, the consideration of including cervical assessment is essential.
Active Movements
The examination is performed with the patient in the sitting position. As always, active movements are done first, and it is important to remember that the most painful movements are done last. In addition, structures outside the joint may affect range of motion (ROM). For example, with lateral epicondylitis, the long extensors of the forearm are often found to be tight or shortened, so the position of the wrist and fingers may affect movement.
Active elbow flexion is 140° to 150°. Movement is usually stopped by contact of the forearm with the muscles of the arm.
Active elbow extension is 0°, although up to a 10° hyperextension may be exhibited, especially in women. This hyperextension is considered normal if it is equal on both sides and there is no history of trauma. Normally, the movement is arrested by the locking of the olecranon process of the ulna into the olecranon fossa of the humerus. In some cases, under violent compressive loads (e.g., gymnastics, weight lifting), the olecranon process may act as a pivot, resulting in posterior dislocation of the elbow. This mechanism of injury is more likely to occur in someone with elbows that normally hyperextend (Figure 6-14). Loss of elbow extension is a sensitive indicator of intra-articular pathology. It is the first movement lost after injury to the elbow and the first regained with healing. However, terminal flexion loss is more disabling than the same degree of terminal extension loss because of the need of flexion for many activities of daily living (ADLs). Loss of either motion affects the area of reach of the hand, which in turn affects function.

Active supination should be 90° so that the palm faces up. The examiner should ensure that the shoulder is not adducted further in an attempt to give the appearance of increased supination or to compensate for a lack of sufficient supination (Figure 6-15).11
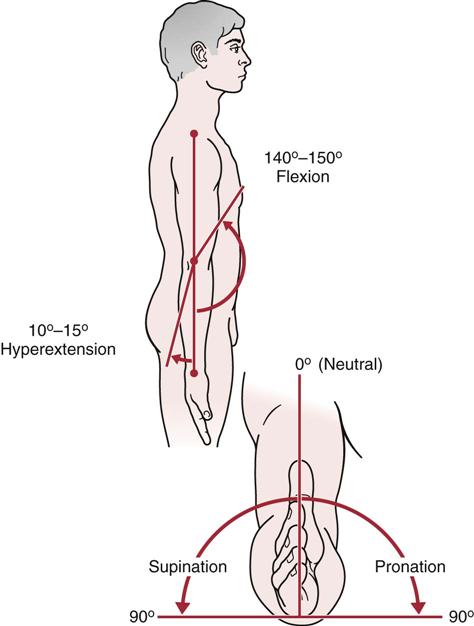
 Figure 6-15 Range of motion (ROM) at the elbow.
Figure 6-15 Range of motion (ROM) at the elbow.For active pronation, the ROM is approximately the same (80° to 90°) so that the palm faces down. The examiner should be sure that the patient does not abduct the shoulder in an attempt to increase the amount of pronation or to compensate for a lack of sufficient pronation.11 However, for both supination and pronation, only about 75° of movement occurs in the forearm articulations. The remaining 15° is the result of wrist action.
If, in the history, the patient has complained that combined movements, repetitive movements, or sustained positions cause pain, these specific movements should be included in the active movement assessment. If the patient has difficulty or cannot complete a movement, but it is pain free, the examiner must consider a severe injury to the contractile tissue (rupture) or a neurological injury, and further testing is necessary.
Passive Movements
If the ROM is full on active movements, overpressure may be gently applied to test the end feel in each direction. If the movement is not full, passive movements should be carried out carefully to test the end feel and to test for a capsular pattern.
It should be pointed out that although tissue approximation is the normal end feel of elbow flexion, in thin patients the end feel may be bone to bone as a result of the coronoid process hitting in the coronoid fossa. Likewise, in thin individuals, pronation may be bone to bone.
In addition to the end feel tests during passive movements, the examiner should note whether a capsular pattern is present. The capsular pattern for the elbow complex as a whole is more limitation of flexion than extension.
In some cases, the examiner may want to determine whether muscles crossing the elbow are tight. If the muscles are tight, the end feel will be a muscle stretch, and ROM at one of the joints that the muscle passes over will be restricted (usually the joint that is the last to be stretched). If the muscle is normal, the end feel will be the normal joint tissue stretch end feel and the ROM will be normal. To test biceps length (Figure 6-16, A), the patient is placed in supine with the shoulder to be tested off the edge of the bed. The shoulder is passively extended to end range and then the elbow is extended.12 Normally, elbow extension should be the same as that seen with active movement.

A, Biceps. B, Triceps. C, Long wrist extensors. D, Long wrist flexors.
To test triceps length (Figure 6-16, B), the patient is placed in sitting. The examiner passively forward flexes the arm to full elevation while the elbow is in extension. The elbow is then passively flexed.9 Normally, elbow flexion should be similar to that seen with active movement.
To test the length of the long wrist extensors (as one would want to do with lateral epicondylitis), the patient is placed in supine lying with the elbow extended (Figure 6-16, C). The examiner passively flexes the fingers and then flexes the wrist.12 Normally, wrist flexion and finger flexion should be the same as found with active movement.
To test the length of the long wrist flexors (Figure 6-16, D), the patient is placed in supine lying with the elbow extended. The examiner passively extends the fingers and then the wrist.12 Normally, wrist extension and finger extension should be the same as that found with active movement.
Resisted Isometric Movements
For proper testing of the muscles of the elbow complex, the movement must be resisted and isometric. Muscle flexion power around the elbow is greatest in the range of 90° to 110° with the forearm supinated. At 45° and 135°, flexion power is only 75% of maximum.9 Isometrically, research shows that men are two times stronger than women at the elbow; extension is 60% of flexion, and pronation is about 85% of supination.13 To perform the resisted isometric tests, the patient is seated (Figure 6-17 ). If the examiner finds that a particular movement or movements cause pain, Table 6-1 can be used to help differentiate the cause. Carrying out wrist extension and flexion is also necessary, because a large number of muscles act over the wrist as well as the elbow.
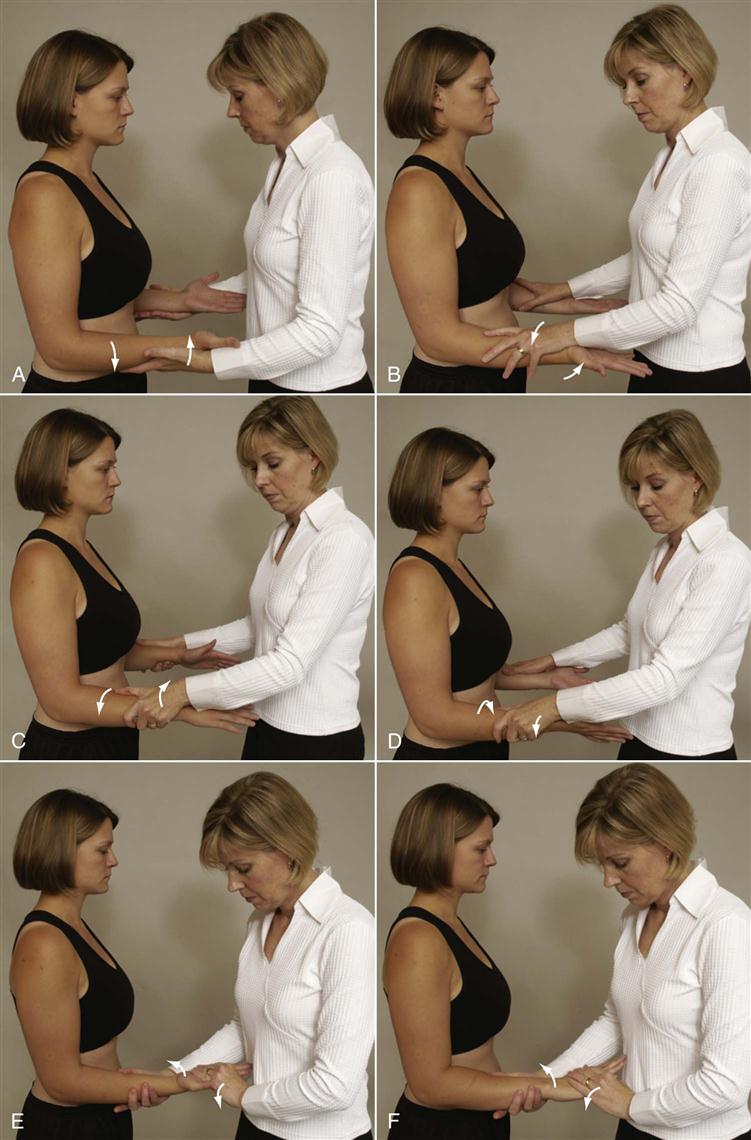
 Figure 6-17 Positioning for resisted isometric movements.
Figure 6-17 Positioning for resisted isometric movements.A, Elbow extension. B, Elbow flexion. C, Forearm supination. D, Forearm pronation. E, Wrist flexion. F, Wrist extension.
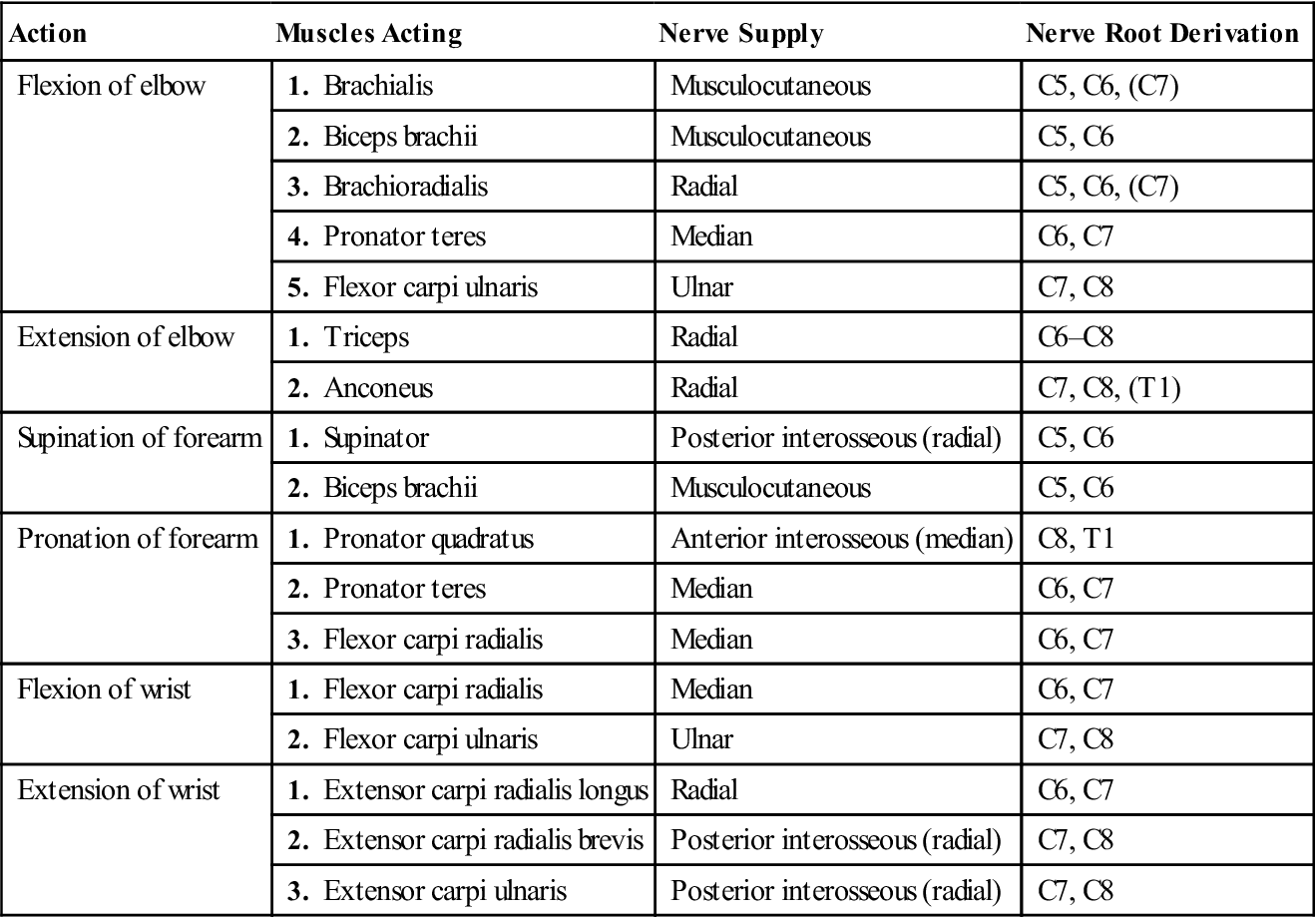
Table 6-1
Muscles about the Elbow: Their Actions, Nerve Supply, and Nerve Root Derivation
| Action | Muscles Acting | Nerve Supply | Nerve Root Derivation |
| Flexion of elbow | 1. Brachialis | Musculocutaneous | C5, C6, (C7) |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| 3. Brachioradialis | Radial | C5, C6, (C7) | |
| 4. Pronator teres | Median | C6, C7 | |
| 5. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Extension of elbow | 1. Triceps | Radial | C6–C8 |
| 2. Anconeus | Radial | C7, C8, (T1) | |
| Supination of forearm | 1. Supinator | Posterior interosseous (radial) | C5, C6 |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| Pronation of forearm | 1. Pronator quadratus | Anterior interosseous (median) | C8, T1 |
| 2. Pronator teres | Median | C6, C7 | |
| 3. Flexor carpi radialis | Median | C6, C7 | |
| Flexion of wrist | 1. Flexor carpi radialis | Median | C6, C7 |
| 2. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Extension of wrist | 1. Extensor carpi radialis longus | Radial | C6, C7 |
| 2. Extensor carpi radialis brevis | Posterior interosseous (radial) | C7, C8 | |
| 3. Extensor carpi ulnaris | Posterior interosseous (radial) | C7, C8 |
If, in the history, the patient has complained that combined movements under load, repetitive movements under load, or sustained positions under load cause pain, the examiner should carefully examine these resisted isometric movements and positions as well, but only after the basic movements have been tested isometrically. For example, the biceps is a strong supinator and flexor of the elbow, but its ability to generate force depends on the position of the elbow. The biceps play a greater role in elbow flexion when the forearm is supinated than when it is pronated. At 90° of elbow flexion, biceps makes its greatest contribution to supination.14 If the history indicates that concentric, eccentric, or econcentric movements have caused symptoms, these movements should also be tested with load or no load, as required.
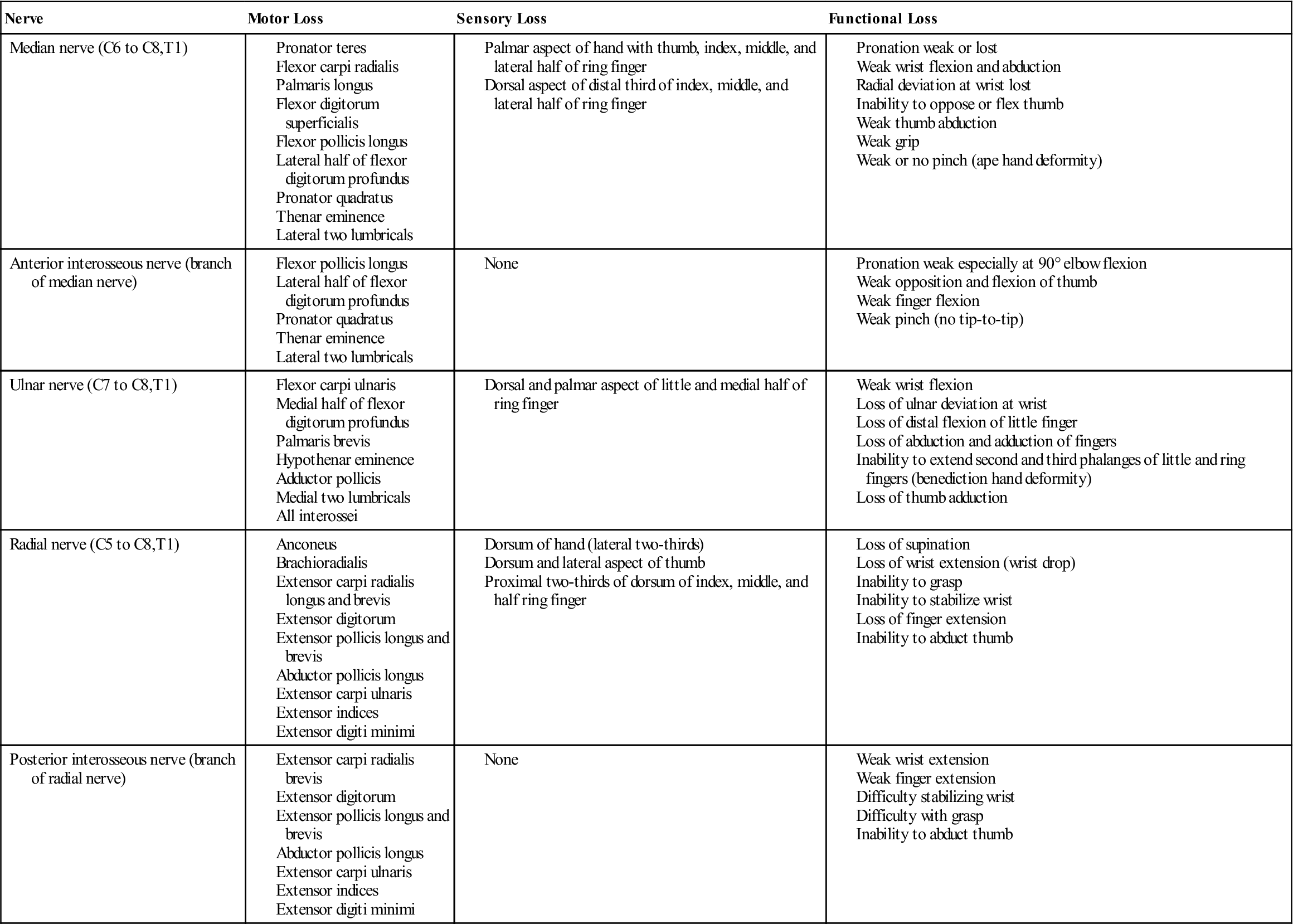
If the resisted isometric contraction is weak and pain free, the examiner must consider a major injury to the contractile tissue (third-degree strain) or neurological injury. For example, weakness of elbow flexion and supination may occur with a rupture of the distal biceps tendon, especially if these findings follow a sudden sharp pain in the antecubital fossa when an extension force is applied to the flexing elbow.14 If there is no history of trauma, the most likely cause is neurological, either a nerve root or peripheral nerve lesion. By selectively testing the muscles and sensory distribution (Table 6-2) and by having a knowledge of nerve compression sites (see the “Reflexes and Cutaneous Distribution” section), the examiner should be able to determine the neurological tissue injured and where the injury has occurred.
Table 6-2
Nerve Injuries About the Elbow
Functional Assessment
When assessing the elbow, it is important to remember that the elbow is the middle portion of an integral upper limb kinetic chain. It allows the hand to be positioned in space, helps stabilize the upper extremity for power and detailed work activities, and provides power to the arm for lifting activities.15 Motion in the elbow allows the hand to be positioned so that daily functions can be performed easily. Thus, functionally, the elbow is often one part of a functional assessment that may also involve the shoulder and/or hand. This is especially true for athletes who put several joints in the kinetic chain under stress at the same time. For example, the Kerlan-Jobe Orthopaedic Clinic (KJOC) shoulder and elbow score (Figure 6-18 ) is a function score that is designed to look at a functional outcome score involving the shoulder and elbow in overhead athletes.16,17
The full range of elbow movements is not necessary to perform these activities; most ADLs are performed at between 30° and 130° of flexion and between 50° of pronation and 50° of supination (Figures 6-19 and 6-20). To reach the head, approximately 140° of flexion is needed. The activities of combing or washing the hair, reaching a back zipper, and walking with crutches require a greater ROM. Activities, such as pouring fluid, drinking from a container, cutting with a knife, reading a newspaper, and using a screwdriver, require an adequate range of supination and pronation. Figures 6-21 and 6-22 show the ROM or arc of movement necessary to do certain activities or the ROM needed to touch parts of the body. Examiners must remember that elbow injuries may preclude lifting objects as light as a cup of coffee, owing to lifting mechanics. Because of the length of the lever arm of the forearm when the elbow is at 90°, loads at the hand are magnified tenfold at the elbow.18 Figure 6-23 is a numerical scoring assessment form that can be used to assess the elbow and includes an important functional component. Table 6-3 demonstrates functional tests of strength for the elbow.
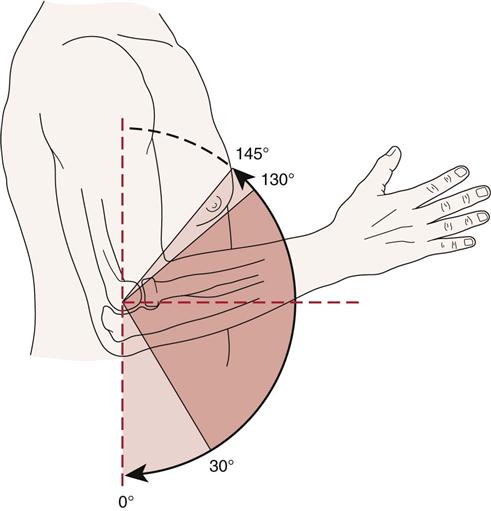
However, the functional arc of motion is somewhat less, and most activities can be performed with flexion of 30° to 130°. (Redrawn from Regan WD, Morrey BF: The physical examination of the elbow. In Morrey BF, editor: The elbow and its disorders, ed 2, Philadelphia, 1993, WB Saunders, p. 81.)
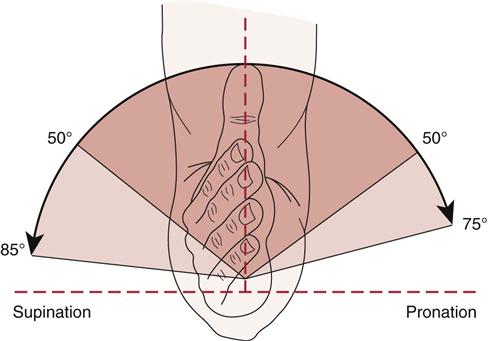
Most activities of daily living (ADLs), however, can be accomplished with 50° of each motion. (Redrawn from Regan WD, Morrey BF: The physical examination of the elbow. In Morrey BF, editor: The elbow and its disorders, ed 2, Philadelphia, 1993, WB Saunders, p. 81.)
Table 6-3
Functional Testing of the Elbow
| Starting Position | Action | Functional Test* |
| Sitting | Bring hand to mouth lifting weight (elbow flexion) | |
| Standing 90 cm from wall, leaning against wall | Push arms straight (elbow extension) | |
| Standing, facing closed door | Open door starting with palm down (supination of arm) | |
| Standing, facing closed door | Open door starting with palm up (pronation of arm) |
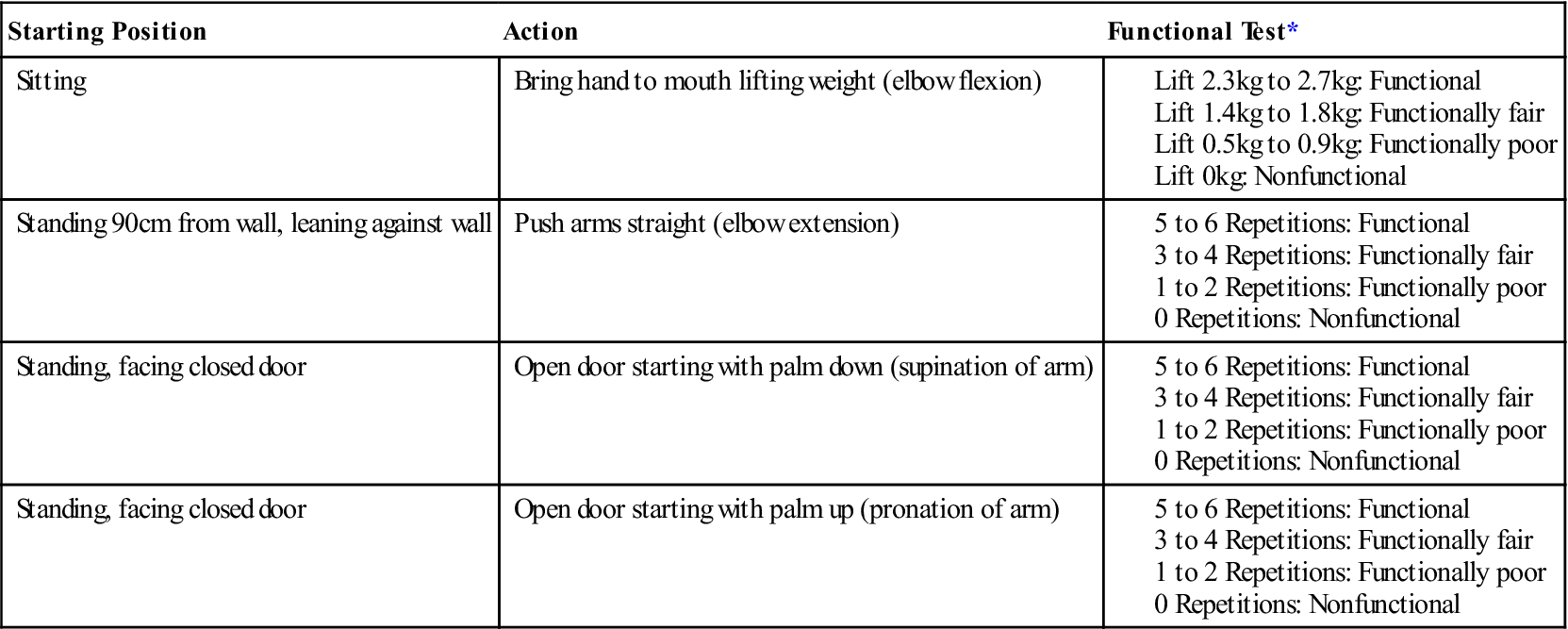
*Younger patients should be able to lift more (2.7 kg to 4.5 kg) more often (6 to 10 repetitions). With age, weight and repetitions decrease.
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 109–111.
Special Tests
An examiner should perform only those special tests that have relevance or will help to confirm the diagnosis. If the history has not indicated any trauma or repetitive movement that could be associated with problems, the examiner, depending on the age of the patient, may want to include some of the nerve root compression tests (see Chapter 3) to rule out the possibility of referred symptoms from the cervical spine or the possibility of a “double crush” injury.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the elbow joint are available on the Evolve website.
APPENDIX 6-1
Reliability, Validity, Specificity and Sensitivity of Special/Diagnostic Tests Used in the Elbow
| MOVING VALGUS STRESS TEST | |
| Specificity | Sensitivity |
| PATIENT-RELATED FOREARM EVALUATION QUESTIONNAIRE | |
| Reliability | |
| PRESSURE PROVOCATIVE TEST | ||
| Specificity | Sensitivity | Odds Ratio |
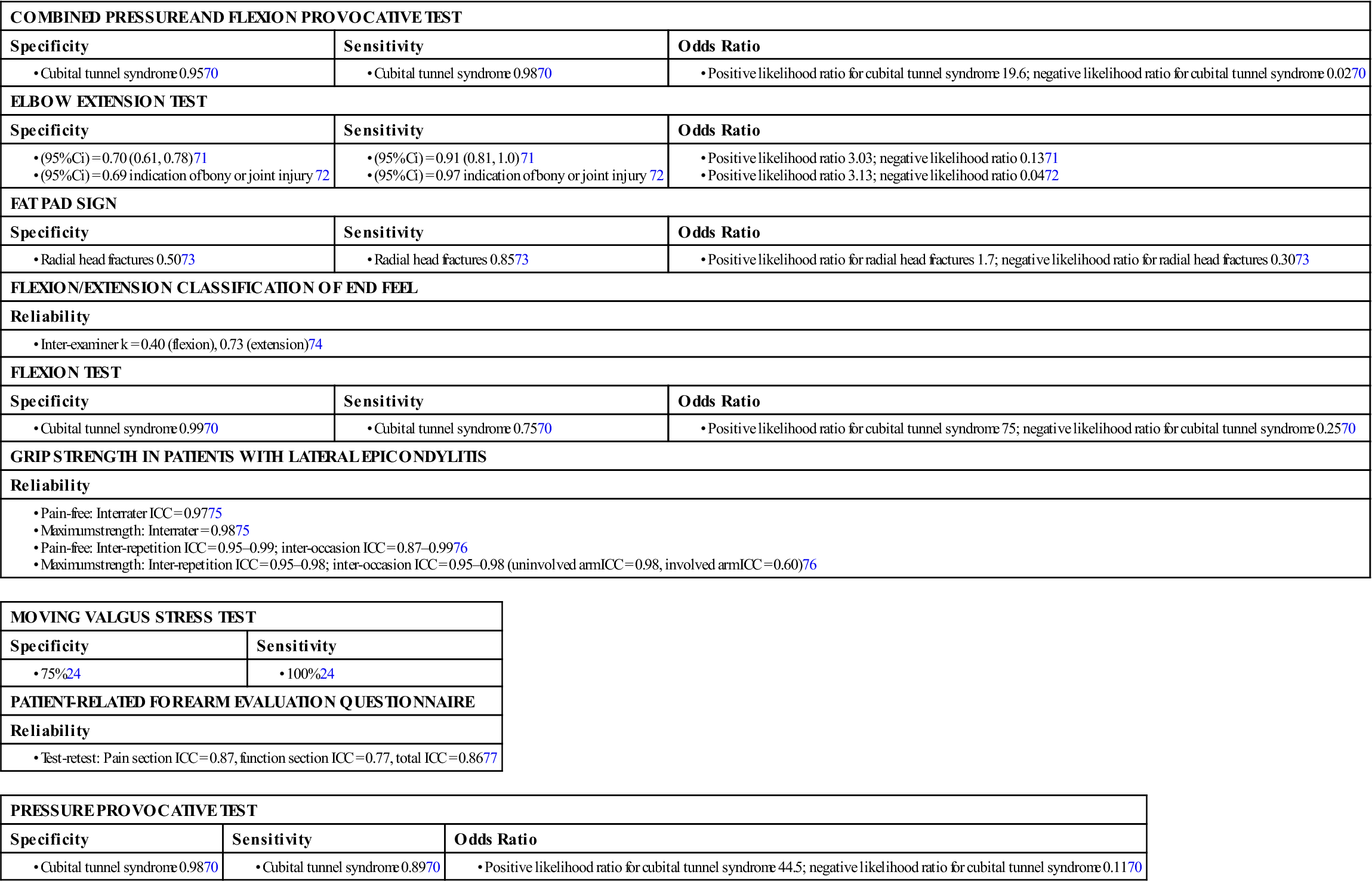
Ci, Curie; ICC, intraclass correlation coefficient; k, kappa.
Tests for Ligamentous Instability
These tests are designed to test for valgus and varus instability in the elbow.
 Lateral Pivot Shift Test of the Elbow.2,21
Lateral Pivot Shift Test of the Elbow.2,21
The patient lies supine with the arm to be tested overhead. The examiner grasps the patient’s wrist and forearm with the elbow extended and the forearm fully supinated.22 The patient’s elbow is then flexed while a valgus stress and axial compression is applied to the elbow while maintaining supination. This causes the radius (and ulna) to sublux off the humerus leading to a prominent radial head posterolaterally and a dimple between the radial head and capitellum (Figure 6-24, A).2,22 If the examiner continues flexing the elbow, at about 40° to 70°, there is a sudden reduction (clunk) of the joint, which can be palpated and seen (Figure 6-24, B).23 If the patient is unconscious, subluxation and a clunk on reduction when the elbow is extended may occur, but these symptoms seldom present in the conscious patient.
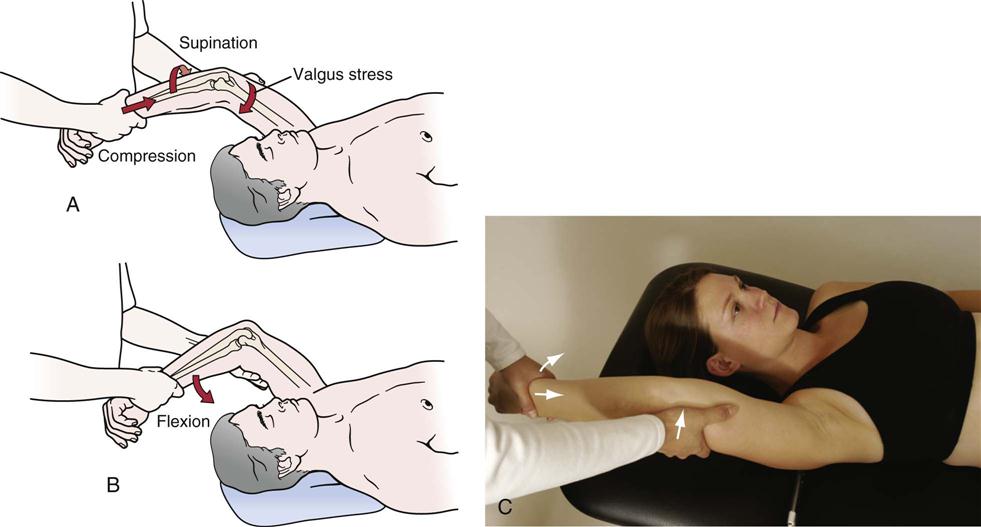
 Figure 6-24 Posterolateral pivot-shift apprehension test of the elbow.
Figure 6-24 Posterolateral pivot-shift apprehension test of the elbow.A, The patient lies supine with the arm overhead. A mild supination force is applied to the forearm at the wrist. The patient’s elbow is then flexed while a valgus stress and compression is applied to the elbow. B, If the examiner continues flexing the elbow at about 40° to 70°, subluxation and a clunk on reduction when the elbow is extended may occur, but usually only in the unconscious patient. C, Actual test with elbow positioned to resemble knee.
 Ligamentous Valgus Instability Test.
Ligamentous Valgus Instability Test.
To test for valgus instability, the patient’s arm is stabilized with one of the examiner’s hands at the elbow and the other hand placed above the patient’s wrist. An abduction or valgus force at the distal forearm is applied to test the medial collateral ligament (valgus instability) while the ligament is palpated (Figure 6-25, B).2 Regan and Morrey advocate doing the valgus stress test with the humerus in full lateral rotation.18 The examiner should note any laxity, decreased mobility, or altered pain that may be present compared with the uninvolved elbow.
 Ligamentous Varus Instability Test.
Ligamentous Varus Instability Test.
With the patient’s elbow slightly flexed (20° to 30°) and stabilized with the examiner’s hand, an adduction or varus force is applied by the examiner to the distal forearm to test the lateral collateral ligament (varus instability) while the ligament is palpated (Figure 6-25, A). Normally, the examiner feels the ligament tense when stress is applied. Regan and Morrey advocated doing the varus stress test with the humerus in full medial rotation.18 The examiner applies the force several times with increasing pressure while noting any alteration in pain or ROM. If excessive laxity is found when doing the test or a soft end feel is felt, it indicates injury to the ligament (1°, 2°, or 3° sprain) and may, especially with a 3° sprain, indicate posterolateral joint instability. Posterolateral elbow instability is the most common pattern of elbow instability in which there is displacement of the ulna (accompanied by the radius) on the humerus, so the ulna supinates or laterally rotates away from or off the trochlea.21
 Milking Maneuver.2
Milking Maneuver.2
The patient sits with the elbow flexed to 90° or more and the forearm supinated. The examiner grasps the patient’s thumb under the forearm and pulls it imparting a valgus stress to the elbow (Figure 6-26). Reproduction of symptoms indicates a positive test and a partial tear of the medial collateral ligament.
 Moving Valgus Stress Test.2,24
Moving Valgus Stress Test.2,24
The patient lies supine or stands with the arm abducted and elbow flexed fully. While maintaining a valgus stress, the examiner quickly extends the patient’s elbow. Reproduction of the patient’s pain between 120° to 70° indicates a positive test and a partial tear of the medial collateral ligament (Figure 6-27).
 Posterolateral Rotary Apprehension Test.2,21–23,25,26
Posterolateral Rotary Apprehension Test.2,21–23,25,26
The patient lies supine with the arm to be tested overhead. The elbow is supinated at the wrist, and a valgus stress is applied to the elbow while the examiner flexes the elbow. This movement (between 20° and 30° flexion) and stress cause the patient to be apprehensive that the elbow will dislocate while reproducing the patient’s symptoms. In the conscious patient, actual subluxation is rare. A positive test indicates posterolateral rotary instability (Figure 6-28).

 Figure 6-28 Posterolateral rotary apprehension test.
Figure 6-28 Posterolateral rotary apprehension test. Posterolateral Rotary Drawer Test.2
Posterolateral Rotary Drawer Test.2
The patient lies supine with the arm to be tested overhead and the elbow flexed 40° to 90° while the examiner holds the forearm and arm similar to doing a drawer test at the knee. As the humerus is stabilized and the radius and ulna are pushed posterolaterally, the radius and ulna rotate around an intact medial collateral ligament indicating a tear of the lateral collateral ligament and posterolateral instability at the elbow (Figure 6-29).

 Figure 6-29 Posterolateral rotary drawer test.
Figure 6-29 Posterolateral rotary drawer test. Pushup Test.27
Pushup Test.27
The patient, in supine, attempts to do a pushup—first with the forearms maximally supinated and then repeated with the forearms maximally pronated (Figure 6-30). The test is positive for posterolateral rotary instability if symptoms occur when the forearms are supinated but not pronated.
 Stand Up Test.2,4
Stand Up Test.2,4
The patient is seated in a chair without arms. The patient is asked to push up on the seat with his or her hands with the forearms fully supinated into standing. If the patient’s symptoms are reproduced, the test is positive for injury to the posterior band of the medial collateral ligament (Figure 6-31).
Tests for Biceps Rupture (Third-Degree Strain)
 Biceps Squeeze Test.27,28
Biceps Squeeze Test.27,28
The patient’s elbow is flexed to between 60° and 80°. The examiner then squeezes the biceps muscle belly (Figure 6-32). If the biceps tendon is ruptured, the patient’s forearm will not supinate.
 Hook Test.27,29
Hook Test.27,29
The patient abducts the shoulder to 90° with the elbow flexed to 90° and the arm supinated so that the thumb faces up (Figure 6-33). The patient is then asked to actively supinate the forearm against resistance of the examiner. With the index finger of the other hand, the examiner attempts to “hook” underneath the biceps tendon, “hooking” from lateral to medial at the same time. If no cord like structure can be hooked, the test is positive for a rupture of the distal biceps.

 Figure 6-33 Hook test for biceps rupture at the elbow.
Figure 6-33 Hook test for biceps rupture at the elbow.Tests for Epicondylitis
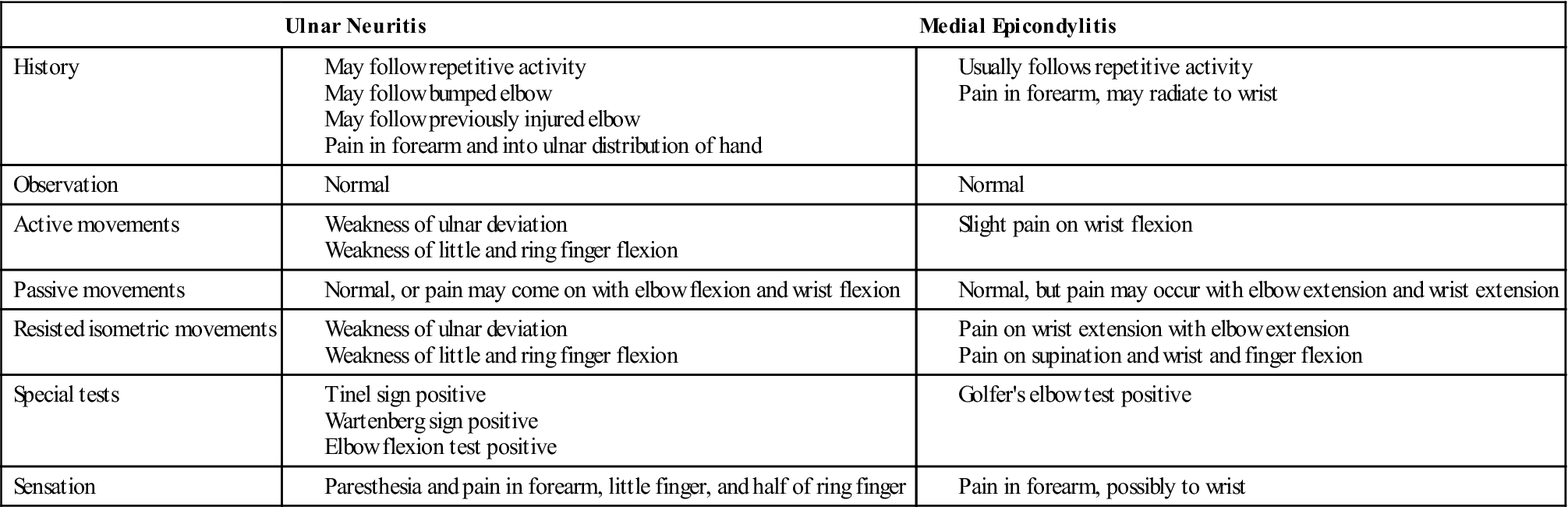
Chronic overuse injury to the extensor (tennis elbow, or lateral epicondylitis) or flexor (golfer’s elbow, or medial epicondylitis) tendons at the elbow result from repeated microtrauma to the tendon leading to disruption and degeneration of the tendon’s internal structure (tendinosus).30 It appears to be a degenerative condition in which the tendon has failed to heal properly after repetitive microtrauma injury.30,31
When testing for epicondylitis, whether medial or lateral, the examiner must keep in mind that there may be referral of pain from the cervical spine or peripheral nerve involvement. If the epicondylitis does not respond to treatment, the examiner would be wise to check for neurological pathology.
 Lateral Epicondylitis (Tennis Elbow or Cozen’s) Test (Method 1).
Lateral Epicondylitis (Tennis Elbow or Cozen’s) Test (Method 1).
The patient’s elbow is stabilized by the examiner’s thumb, which rests on the patient’s lateral epicondyle (Figure 6-34). The patient is then asked to actively make a fist, pronate the forearm, and radially deviate and extend the wrist while the examiner resists the motion. A sudden severe pain in the area of the lateral epicondyle of the humerus is a positive sign. The epicondyle may be palpated to indicate the origin of the pain.
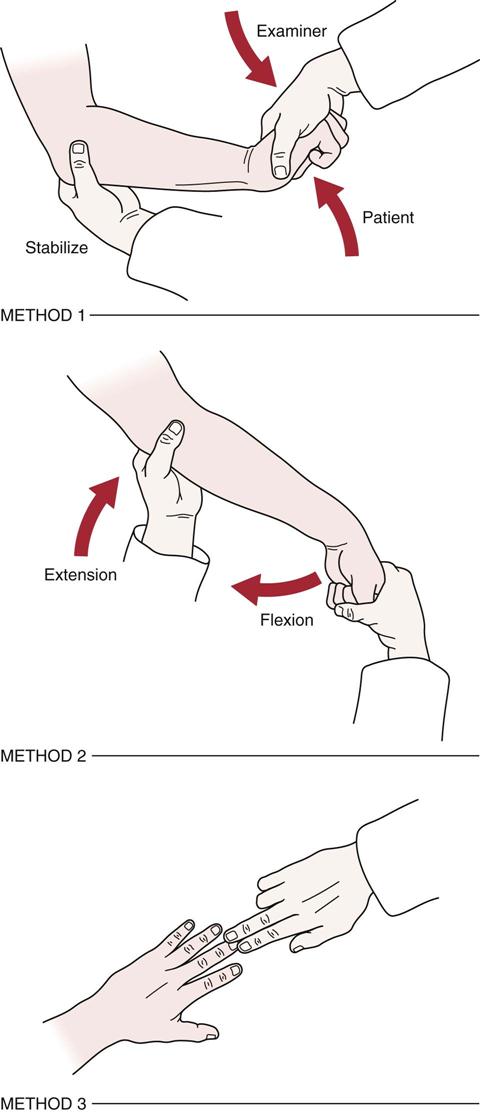
 Figure 6-34 Tests for tennis elbow.
Figure 6-34 Tests for tennis elbow. Lateral Epicondylitis (Tennis Elbow or Mill’s) Test (Method 2).
Lateral Epicondylitis (Tennis Elbow or Mill’s) Test (Method 2).
While palpating the lateral epicondyle, the examiner passively pronates the patient’s forearm, flexes the wrist fully, and extends the elbow (see Figure 6-34). Pain over the lateral epicondyle of the humerus indicates a positive test. This maneuver also puts stress on the radial nerve and, in the presence of compression of the radial nerve, causes symptoms similar to those of tennis elbow.32 Electrodiagnostic studies help differentiate the two conditions.
 Lateral Epicondylitis (Tennis Elbow or Maudsley’s) Test (Method 3).
Lateral Epicondylitis (Tennis Elbow or Maudsley’s) Test (Method 3).
The examiner resists extension of the third digit of the hand distal to the proximal interphalangeal joint, stressing the extensor digitorum muscle and tendon (see Figure 6-34). A positive test is indicated by pain over the lateral epicondyle of the humerus.
 Medial Epicondylitis (Golfer’s Elbow) Test.
Medial Epicondylitis (Golfer’s Elbow) Test.
While the examiner palpates the patient’s medial epicondyle, the patient’s forearm is passively supinated and the examiner extends the elbow and wrist. A positive sign is indicated by pain over the medial epicondyle of the humerus.
Tests for Plica
 Plica Impingement Test.27,33
Plica Impingement Test.27,33
The examiner applies a valgus load to the elbow while passively flexing the elbow with the forearm held in pronation (Figure 6-35, A). Pain or snapping between 90° and 110° of flexion indicates a positive test for the anterior radiocapitellar plica (flexion-pronation plica test ![]() ). To test the posterior radiocapitellar plica, the examiner applies a valgus load to the elbow while passively extending the elbow with the forearm held in supination (Figure 6-35, B) (extension-supination plica test
). To test the posterior radiocapitellar plica, the examiner applies a valgus load to the elbow while passively extending the elbow with the forearm held in supination (Figure 6-35, B) (extension-supination plica test ![]() ). Pain or a snap would indicate a positive test indicating a possible plica problem or radiocapitellar chondromalacia.
). Pain or a snap would indicate a positive test indicating a possible plica problem or radiocapitellar chondromalacia.
Tests for Posterior Impingement
 Arm Bar Test.27
Arm Bar Test.27
The patient rests the hand of the test arm on the examiner’s shoulder with the elbow extended and shoulder medially rotated. The examiner pulls down on the olecranon to simulate forced extension (Figure 6-36). Reproduction of pain especially posteromedially along the olecranon is a positive test for posterior impingement. The patient may also lack full extension.

 Figure 6-36 Arm bar test for posterior impingement.
Figure 6-36 Arm bar test for posterior impingement. Extension Impingement Test.27
Extension Impingement Test.27
The examiner applies a valgus stress to the elbow while quickly extending and flexing the elbow from 20° to 30° flexion to terminal flexion repeatedly (Figure 6-37). The test is then repeated without the valgus stress while the posteromedial olecranon is palpated for tenderness. This palpation differentiates tender impingement due to instability from pain over the medial olecranon without instability.

 Figure 6-37 Extension impingement test.
Figure 6-37 Extension impingement test.Valgus stress shown.
Tests for Joint Dysfunction
If the patient complains of pain in the elbow joint, especially on elbow movement, the examiner can perform two tests to differentiate between the radiohumeral and ulnohumeral joints. To test the radiohumeral joint ![]() , the examiner positions the elbow joint at the position of pain and then radially deviates the wrist to compress the radial head against the humerus. The production of pain would be considered a positive test. To test the ulnohumeral joint
, the examiner positions the elbow joint at the position of pain and then radially deviates the wrist to compress the radial head against the humerus. The production of pain would be considered a positive test. To test the ulnohumeral joint ![]() , the examiner again positions the elbow joint at the position of discomfort and causes compression of the ulnohumeral joint by ulnar deviation at the wrist.6 Again, pain indicates a positive test.
, the examiner again positions the elbow joint at the position of discomfort and causes compression of the ulnohumeral joint by ulnar deviation at the wrist.6 Again, pain indicates a positive test.
 Active Radiocapitellar Compression Test.27
Active Radiocapitellar Compression Test.27
The examiner applies an axial (compression) load to the elbow in full extension. The patient is asked to actively supinate and pronate the forearm while the compression is maintained (Figure 6-38). Pain in the lateral compartment of the elbow is a positive test and may indicate an osteochondritis dissecans of the capitellum.
Tests for Neurological Dysfunction
 Elbow Flexion Test.
Elbow Flexion Test.
The patient is asked to fully flex the elbow with extension of the wrist and shoulder girdle abduction (90°) and depression34,35 and to hold this position for 3 to 5 minutes (Figure 6-39). Ochi, et al.36 modified the test to include medial rotation of the shoulder calling it the shoulder internal (medial) rotation elbow flexion test ![]() (Figure 6-40). They state that symptoms should develop in less than 5 seconds. Tingling or paresthesia in the ulnar nerve distribution of the forearm and hand indicates a positive test. The test helps to determine whether a cubital tunnel (ulnar nerve) syndrome is present. The test may be modified by the examiner applying direct pressure over the ulnar nerve with the index and middle finger between the posteromedial olecranon and the medial epicondyle (elbow flexion compression test or cubital tunnel compression test
(Figure 6-40). They state that symptoms should develop in less than 5 seconds. Tingling or paresthesia in the ulnar nerve distribution of the forearm and hand indicates a positive test. The test helps to determine whether a cubital tunnel (ulnar nerve) syndrome is present. The test may be modified by the examiner applying direct pressure over the ulnar nerve with the index and middle finger between the posteromedial olecranon and the medial epicondyle (elbow flexion compression test or cubital tunnel compression test ![]() ) (Figure 6-41).
) (Figure 6-41).

 Figure 6-39 Elbow flexion test for ulnar nerve pathology.
Figure 6-39 Elbow flexion test for ulnar nerve pathology.
Medial rotation of the shoulder, maximum elbow flexion, maximum forearm supination, and maximum wrist extension.

 MacKinnon’s Scratch Collapse Test.
MacKinnon’s Scratch Collapse Test.
The patient stands with the elbow flexed to 90° and by the side. The patient is asked to laterally rotate and abduct the forearms against resistance and then relaxes (Figure 6-42). The examiner then scratches along the course of the ulnar nerve at the elbow and then asks the patient to repeat the movement against resistance. If the patient cannot momentarily laterally rotate against the examiner, it is considered a positive test.37,38
 Pinch Grip Test.
Pinch Grip Test.
The patient is asked to pinch the tips of the index finger and thumb together. Normally, there should be a tip-to-tip pinch. If the patient is unable to pinch tip-to-tip and instead has an abnormal pulp-to-pulp pinch of the index finger and thumb, this is a positive sign for pathology to the anterior interosseous nerve, which is a branch of the median nerve (Figure 6-43). This finding may indicate an entrapment of the anterior interosseous nerve as it passes between the two heads of the pronator teres muscle.39
 Test for Pronator Teres Syndrome.18
Test for Pronator Teres Syndrome.18
The patient sits with the elbow flexed to 90°. The examiner strongly resists pronation as the elbow is extended. Tingling or paresthesia in the median nerve distribution in the forearm and hand indicates a positive test.
 Tinel Sign (at the Elbow).
Tinel Sign (at the Elbow).
The area of the ulnar nerve in the groove (between the olecranon process and medial epicondyle) is tapped. A positive sign is indicated by a tingling sensation in the ulnar distribution of the forearm and hand distal to the point of compression of the nerve (Figure 6-44). The test indicates the point of regeneration of the sensory fibers of a nerve. The most distal point at which the patient feels the abnormal sensation represents the limit of nerve regeneration.
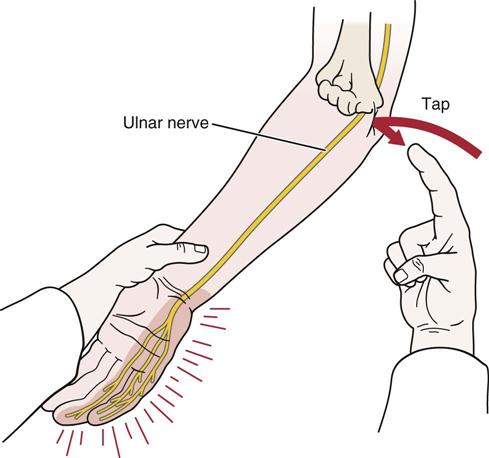
 Figure 6-44 Tinel sign at the elbow for the ulnar nerve.
Figure 6-44 Tinel sign at the elbow for the ulnar nerve. Wartenberg Sign.
Wartenberg Sign.
The patient sits with his or her hands resting on the table. The examiner passively spreads the fingers apart and asks the patient to bring them together again. Inability to squeeze the little finger to the remainder of the hand indicates a positive test for ulnar neuropathy.18,37
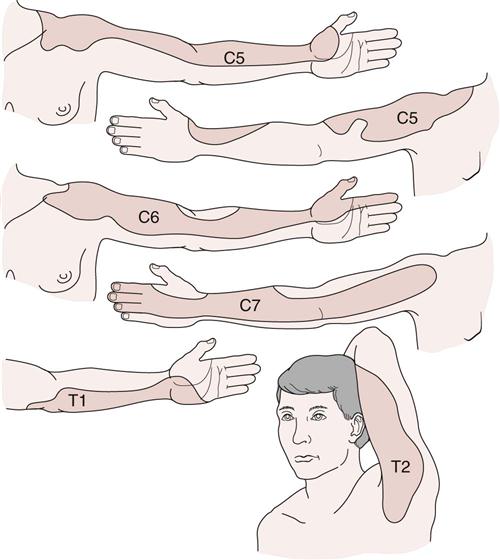
Reflexes and Cutaneous Distribution
The reflexes around the elbow that are often checked (Figure 6-45) include the biceps (C5–C6), brachioradialis (C5–C6), and triceps (C7–C8). The examiner should also assess the dermatomes around the elbow and the cutaneous distribution of the various nerves, noting any difference (Figures 6-46 and 6-47). When looking at the dermatomes, the examiner should realize there is a great deal of variability in the distribution patterns. Except for T2 dermatome, which commonly ends at the elbow, all other dermatomes extend distally to the forearm, wrist, and hand; therefore, the elbow cannot be looked at in isolation when viewing dermatomes. Similarly, the peripheral nerves extend into the forearm, wrist, and hand, and so testing for sensory loss must involve the whole upper limb, not just the elbow. Pain may be referred to the elbow and surrounding tissues from the neck (often mimicking tennis elbow), the shoulder, or the wrist (Figure 6-48; Table 6-4).
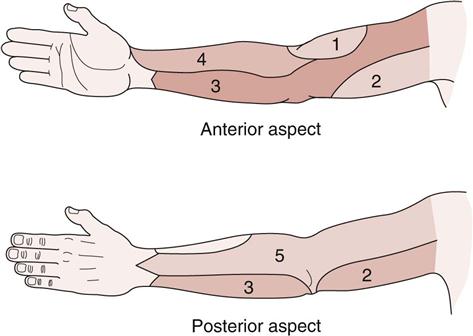
1, Lower lateral cutaneous nerve of arm (radial): 2, medial cutaneous nerve of arm; 3, medial cutaneous nerve of forearm; 4, lateral cutaneous nerve of forearm (musculocutaneous nerve); 5, posterior cutaneous nerve of forearm (radial nerve).
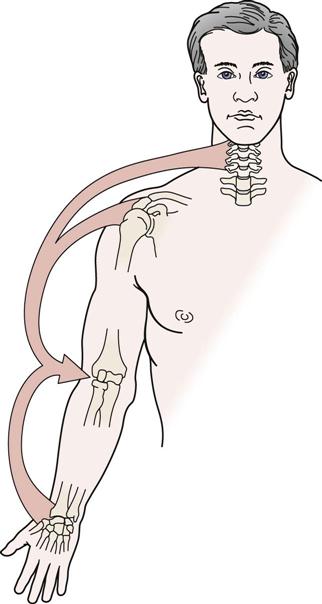
Table 6-4
Elbow Muscles and Referral of Pain
| Muscles | Referral Pattern |
| Biceps | Upper shoulder (bicipital groove) to anterior elbow |
| Brachialis | Anterior arm, elbow to lateral thenar eminence |
| Triceps | Posterior shoulder, arm, elbow, and forearm to medial two fingers, medial epicondyle |
| Brachioradialis | Lateral epicondyle, lateral forearm to posterior web space between thumb and index finger |
| Anconeus | Lateral epicondyle area |
| Supinator | Lateral epicondyle and posterior web space between thumb and index finger |
| Pronator teres | Anterior forearm to wrist and part of anterior thumb |
| Extensor carpi ulnaris | Medial wrist |
| Extensor carpi radialis brevis | Posterior forearm to posterior wrist |
| Extensor carpi radialis longus | Lateral epicondyle to posterolateral wrist |
| Extensor indices | Posterior forearm to appropriate digit |
| Palmaris longus | Anterior forearm to palm |
| Flexor digitorum superficialis | Palm to appropriate digit |
| Flexor carpi ulnaris | Anteromedial wrist |
| Flexor carpi radialis | Anteromedial wrist |
In the extremities, the neurological tissues (nerve roots and peripheral nerves) play a significant role in function. Injury, pinching, or stress to these structures can have dire consequences functionally for the patient. The next section is a review of the peripheral nerves and how and where they may be traumatized about the elbow.
Peripheral Nerve Injuries About the Elbow
Median Nerve (C6–C8, T1).
In the elbow region, the median nerve proper can be injured by trauma (e.g., lacerations, fractures, dislocations), by systemic disease, and especially by compression and/or traction.40–42
The median nerve may also be pinched or compressed above the elbow as it passes under the ligament of Struthers, an anomalous structure found in approximately 1% of the population (Figure 6-49).43 The ligament runs from an abnormal spur on the shaft of the humerus to the medial epicondyle of the humerus. Because the brachial artery sometimes accompanies the nerve through this tunnel, it may also be compressed, resulting in possible vascular as well as neurological symptoms. In this case, the neurological involvement would include weakness of the pronator teres muscle and of those muscles affected by the pronator syndrome (see later discussion). The condition may also be called the humerus supracondylar process syndrome. Pressure in the ligament of Struthers area leads to motor loss (see Table 6-2) and sensory loss (see Figure 7-81) of the median nerve. Initially, the patient complains of pain and paresthesia in the elbow and forearm; abnormality of motor function is secondary. With time, however, motor function is also affected, with wrist and finger flexion as well as thumb movements being most affected.
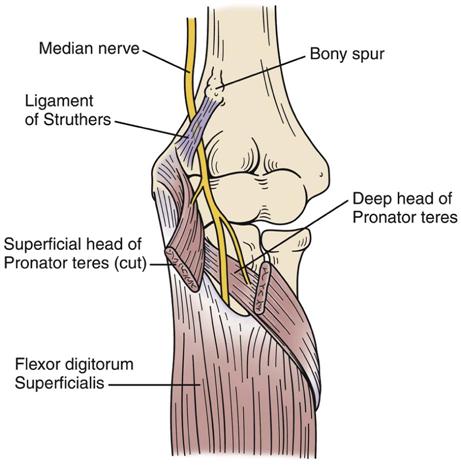
In the pronator syndrome, the median nerve may be kinked against the flexor digitorum superficialis muscle or compressed by the forceful action or structural hypertrophy of the deep head of the pronator teres. Compression of the nerve above the elbow (ligament of Struthers) leads to weakness of the pronator teres while this muscle is spared in the pronator syndrome, because the branches to the two heads of the pronator teres arise proximally to the muscle.
A second area of compression of the median nerve as it passes through the elbow occurs where it passes through the two heads of pronator teres (pronator syndrome). In this case, the pronator teres remains normal, but the other muscles supplied by the median nerve (see Table 6-2 ) are affected, as is its sensory distribution. Pronation is possible, but weakness is evident as pronation is loaded. If the elbow is flexed to 90° and pronation is tested, noticeable weakness occurs, because in this position the action of pronator teres is minimized.
Butlers and Singer44 reported four possible ways of eliciting median nerve symptoms if the nerve is suffering from pathology:
• Resisted pronation with elbow and wrist flexion for 30 to 60 seconds
• Resisted elbow flexion and supination
• Resisted long finger flexion at the proximal interphalangeal joint
• Direct pressure over the proximal aspect of pronator teres during pronation
It is interesting to note that one of the tests is similar to Mill’s test for lateral epicondylitis. The results should be compared with the good side, and production of the patient’s symptoms is considered a positive test.
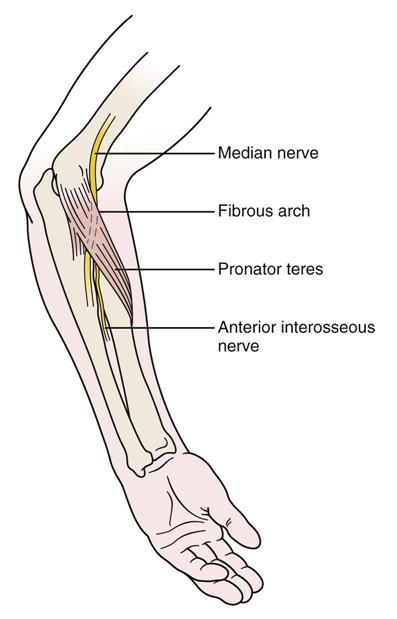
Anterior Interosseous Nerve.
The anterior interosseous nerve, which is a branch of the median nerve, is sometimes pinched or entrapped as it passes between the two heads of the pronator teres muscle, leading to pain and functional impairment of the flexor pollicis longus, the lateral half of the flexor digitorum profundus, and the pronator quadratus muscles. The condition is called anterior interosseous nerve syndrome or Kiloh-Nevin syndrome (Figure 6-50)45,46 and is characterized by a pinch deformity (see Figure 6-43). The deformity results from the paralysis of the flexors of the index finger and thumb. This leads to extension of the distal interphalangeal joint of the index finger and the interphalangeal joint of the thumb. The resulting pinch is pulp to pulp rather than tip to tip. It has been reported that the nerve may also be injured with a forearm fracture (Monteggia fracture).47 With anterior interosseous syndrome, there is no sensory loss, because the anterior interosseous nerve is a motor nerve; signs and symptoms of the condition are related to motor function.
Ulnar Nerve (C7–C8, T1).
In the elbow region, the ulnar nerve is most likely to be injured, compressed, or stretched in the cubital tunnel (see Figure 6-4, A).37,42,43,48–52 In fact, it is a common entrapment neuropathy, second only to carpal tunnel syndrome. The ulnar nerve may be injured or compressed as a result of swelling (e.g., trauma, pregnancy), osteophytes, arthritic diseases, trauma, or repeated microtrauma. This tunnel, which is relatively long, can compress the nerve as the nerve passes through the tunnel or between the two heads of the flexor carpi ulnaris muscle. Compression is altered as the elbow moves from extension (decreased) to flexion (increased), causing traction on the nerve, and is further enhanced if a significant cubitus valgus is present.53,54 Symptoms therefore are more likely to occur when the elbow is flexed. It is usually in the cubital tunnel area that the ulnar nerve is affected, leading to tardy ulnar palsy. If the problem is the result of restriction in the cubital tunnel, direct pressure over the tunnel may reproduce or exacerbate the symptoms (see “Cubital Tunnel Compression Test”).42
Tardy ulnar palsy implies that the symptoms of nerve injury come on long after the patient has been injured; this delayed reaction seems to be unique to the ulnar nerve. Although most common in adults, it has been reported in children, and in children the delay has been up to 29 months.55 In adults, the possibility of a double crush injury (at cervical spine and elbow) should always be considered.
Injury to the ulnar nerve in the cubital tunnel affects the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus in the forearm, the hypothenar eminence in the hand (flexor digiti minimi, abductor digiti minimi, opponens digiti minimi, and adductor pollicis), the interossei, and the third and fourth lumbrical muscles (see Table 6-2). Commonly, patients cannot fully adduct the little finger and hold the finger abducted and extended, because the denervated palmar interosseous muscle cannot oppose the abductor digiti minimi (see “Wartenberg Sign”).37 Although these muscles show weakness and atrophy over time, the earliest and most obvious symptoms are sensory with pain and paresthesia in the medial elbow and forearm and paresthesia in the ulnar sensory distribution of the hand (see Figure 7-81).
Calfee, et al.56 recommended testing for a hypermobile ulnar nerve which is reported to be found in over 30% of the population (hypermobile ulnar nerve test ![]() ). The patient maximally flexes the elbow with the forearm supinated. The examiner then places a finger on the proximal, posteromedial aspect of the medial epicondyle. While holding the finger in place, the patient is asked to extend the elbow. If the ulnar nerve stays anterior to the examiner’s finger, it is said to dislocate. If the nerve is below the examiner’s finger, it is perched on the medial humeral epicondyle. If the nerve cannot be palpated, it is stable in the groove.
). The patient maximally flexes the elbow with the forearm supinated. The examiner then places a finger on the proximal, posteromedial aspect of the medial epicondyle. While holding the finger in place, the patient is asked to extend the elbow. If the ulnar nerve stays anterior to the examiner’s finger, it is said to dislocate. If the nerve is below the examiner’s finger, it is perched on the medial humeral epicondyle. If the nerve cannot be palpated, it is stable in the groove.
Radial Nerve (C5–C8, T1).
The radial nerve may be injured near the elbow if there is a fracture of the shaft of the humerus. The nerve may be damaged as it winds around behind the humerus in the radial groove. Injury may occur at the time of the fracture, or the nerve may get caught in the callus of fracture healing. Because the radial nerve supplies all of the extensor muscles of the arm, only the triceps is spared with this type of injury, and even it may show some weakness.
The major branch of the radial nerve in the forearm is the posterior interosseous nerve, which is given off in front of the lateral epicondyle of the humerus.43,57 This branch may compress as it passes between the two heads of the supinator in the arcade or canal of Frohse, a fibrous arch in the supinator muscle occurring in 30% of the population (Figure 6-51). Compression can lead to functional involvement of the forearm extensor muscles (see Table 6-2) and functional wrist drop, and so the patient has difficulty or is unable to stabilize the wrist for proper hand function. Diagnosis of this condition is often delayed because there is no sensory deficit. Direct pressure over the supinator muscle while resisting supination may elicit weakness of supination or tenderness (supinator compression test ![]() ).42 This compression zone is one of five sites in the tunnel through which the radial nerve passes. The nerve may also be compressed at the entrance to the tunnel anterior to the head of the radius, near where the nerve supplies brachioradialis and extensor carpi radialis longus, between the ulnar half of the tendon of extensor carpi radialis brevis and its fascia, and at the distal border of supinator.58,59 This condition, sometimes called radial tunnel syndrome, may mimic tennis elbow.32,58,60–63 If the patient has a persistent form of tennis elbow, a possible nerve lesion or cervical problem should be considered.
).42 This compression zone is one of five sites in the tunnel through which the radial nerve passes. The nerve may also be compressed at the entrance to the tunnel anterior to the head of the radius, near where the nerve supplies brachioradialis and extensor carpi radialis longus, between the ulnar half of the tendon of extensor carpi radialis brevis and its fascia, and at the distal border of supinator.58,59 This condition, sometimes called radial tunnel syndrome, may mimic tennis elbow.32,58,60–63 If the patient has a persistent form of tennis elbow, a possible nerve lesion or cervical problem should be considered.
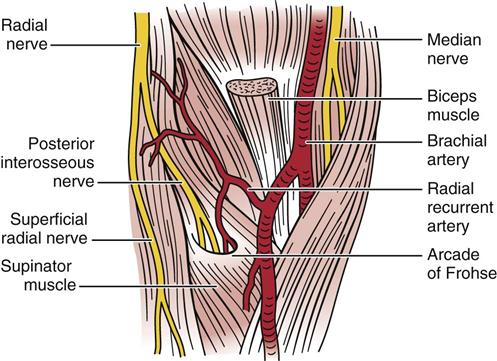
A third area of pathology is compression of the superficial branch of the radial nerve as it passes under the tendon of the brachioradialis. This branch is sensory only, and the patient complains primarily of nocturnal pain along the dorsum of the wrist, thumb, and web space. Trauma, a tight cast, any swelling in the area, or forearm pronation with wrist flexion and ulnar deviation may cause the compression and produce paresthesia.42 Direct pressure at the junction of extensor carpi radialis longus and brachioradialis may also reproduce the paresthesia or numbness.42 The condition is referred to as cheiralgia paresthetica or Wartenberg disease/sign.51
Joint Play Movements
When examining the joint play movements (Figure 6-52), the examiner must compare the injured side with the normal side.
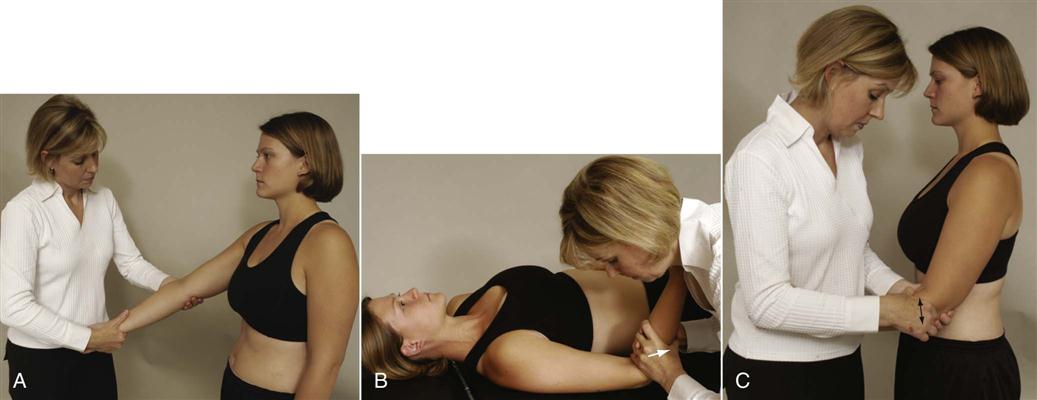
 Figure 6-52 Joint play movements of the elbow complex.
Figure 6-52 Joint play movements of the elbow complex.A, Radial and ulnar deviation of the ulna on the humerus. B, Distraction of the olecranon process from the humerus. C, Anteroposterior movement of the radius.
Radial and ulnar deviations of the ulna and radius on the humerus are performed in a fashion similar to those in the collateral ligament tests but with less elbow flexion. The examiner stabilizes the patient’s elbow by holding the patient’s humerus firmly and places the other hand above the patient’s wrist, abducting and adducting the forearm (see Figure 6-52, A). The patient’s elbow is almost straight (extended) during the movement, and the end feel should be bone-to-bone.
To distract the olecranon from the humerus, the examiner flexes the patient’s elbow to 90°. Wrapping both hands around the patient’s forearm close to the elbow, the examiner then applies a distractive force at the elbow, ensuring that no torque is applied (see Figure 6-52, B). If the patient has a sore shoulder, counter force should be applied with one hand around the humerus.
To test anteroposterior glide of the radius on the humerus, the examiner stabilizes the patient’s forearm. The patient’s arm is held between the examiner’s body and arm. The examiner places the thumb of his or her hand over the anterior radial head while the flexed index finger is over the posterior radial head. The examiner then pushes the radial head posteriorly with the thumb and anteriorly with the index finger (see Figure 6-52, C). Commonly, posterior movement is easier to obtain with anterior movement in normal clients, being the result of the radial head returning to its normal position with a tissue stretch end feel. This movement must be performed with care, because it can be very painful as a result of pinching of the skin between the examiner’s digits and the bone. In addition, pain may result from the force being applied even in the normal arm, so both sides must be compared.
The anterior and posterior glide of the radius may be tested in a slightly different way as well. To do anteroposterior glide of the head of the radius, the patient is placed in supine with the arm by the side. The examiner stands beside the patient, facing the patient’s head, and holds the patient’s arm slightly flexed by holding the hand between the examiner’s thorax and elbow. The examiner places the thumbs over the head of the radius and carefully applies an anteroposterior pressure to the head of the radius feeling the amount of movement and end feel. To do posteroanterior glide, the patient is in supine lying with the arm at the side and the hand resting on the stomach. The examiner places the thumbs over the posterior aspect of the radial head and carefully applies a posteroanterior pressure (Figure 6-53).
Palpation
With the patient’s arm relaxed, the examiner begins palpation on the anterior aspect of the elbow and moves to the medial aspect, the lateral aspect, and finally the posterior aspect (Figure 6-54). The patient may sit or lie supine, whichever is more comfortable. The joint line is located about 2 cm below an imaginary line joining the two epicondyles.4 The examiner is looking for any tenderness, abnormality, change in temperature or in texture of the tissues, or abnormal bumps. As with all palpation, the injured side must be compared with the normal or uninjured side.
A, Olecranon fossa. B, Posterolateral aspect of the elbow. C, Posteromedial aspect of the elbow.
Anterior Aspect
Cubital Fossa.
The fossa is bound by the pronator teres muscle medially, the brachioradialis muscle laterally, and an imaginary line joining the two epicondyles superiorly. Within the fossa, the biceps tendon, brachialis, and brachial artery may be palpated. After crossing the elbow joint, the brachial artery divides into two branches, the radial artery and the ulnar artery. The examiner must be aware of the brachial artery, because it has the potential for being injured as a result of severe trauma at the elbow (e.g., fracture, dislocation). Trauma to this area may lead to compartment syndromes, such as Volkmann ischemic contracture. The median and musculocutaneous nerves are also found in the fossa, but they are not palpable. Pressure on the median nerve may cause symptoms in its cutaneous distribution.
Coronoid Process and Head of Radius.
Within the cubital fossa, if the examiner palpates carefully so as not to hurt the patient, the coronoid process of the ulna and the head of the radius may be palpated. Palpation of the radial head is facilitated by supination and pronation of the forearm. The examiner may palpate the head of the radius from the posterior aspect at the same time by placing the fingers over the head on the posterior aspect and the thumb over it on the anterior aspect. In addition to the muscles previously mentioned, the biceps and brachialis muscles may be palpated for potential abnormality. If the patient is complaining of pain and/or tenderness along the anteromedial humerus, radius, or ulna especially after repeated stress, the examiner should palpate the specific area. This tenderness or pain may be due to periostitis resulting in humeral shin splints or “forearm splints,” which may be precursors to stress fractures.
Medial Aspect
Medial Epicondyle.
Originating from the medial epicondyle are the wrist flexor-forearm pronator groups of muscles. Both the muscle bellies and their insertions into bone should be palpated. Tenderness over the epicondyle where the muscles insert is sometimes called golfer’s elbow or tennis elbow of the medial epicondyle.
Medial (Ulnar) Collateral Ligament.
This fan-shaped ligament may be palpated, because it extends from the medial epicondyle to the medial margin of the coronoid process anteriorly and to the olecranon process posteriorly.
Ulnar Nerve.
If the examiner moves posteriorly behind the medial epicondyle, the fingers will rest over the ulnar nerve in the cubital tunnel (proximal part). Usually, the nerve is not directly palpable, but pressure on the nerve often causes abnormal sensations in its cutaneous distribution. It is this nerve that is struck when someone hits his or her “funny bone.”
Lateral Aspect
Lateral Epicondyle.
The wrist extensor muscles originate from the lateral epicondyle, and their muscle bellies as well as their insertions into the epicondyle should be palpated. It is at this point of insertion of the common extensor tendon that lateral epicondylitis originates. When palpating, the examiner should remember that the extensor carpi radialis longus muscle inserts above the epicondyle along a short ridge extending from the epicondyle to the humeral shaft. The examiner palpates the brachioradialis and supinator muscles on the lateral aspect of the elbow at the same time. If the examiner palpates the lateral epicondyle, the posterior radial head and the olecranon tip, the anconeus “soft spot” will be found within this triangle (Figure 6-55).27
Lateral (Radial) Collateral Ligament.
This cordlike ligament may be palpated as it extends from the lateral epicondyle of the humerus to the annular ligament and lateral surface of the ulna.
Annular Ligament.
Distal to the lateral epicondyle, the annular ligament and head of the radius may be palpated if this has not previously been done. The palpation is facilitated by supination and pronation of the forearm.
Posterior Aspect
Palpation of posterior structures is shown in Figure 6-54.
Olecranon Process and Olecranon Bursa.
The olecranon process is best palpated with the elbow flexed to 90°. If the examiner then grasps the skin overlying the process, the olecranon bursa can be palpated. Normally, it just feels like slippery tissue as the skin is moved. The examiner should note any synovial thickening, swelling, or the presence of any rice bodies, which are small seeds of fragmented fibrous tissue that can act as further irritants to the bursa should it be affected.
Triceps Muscle.
The triceps muscle, which inserts into the olecranon process, should be palpated both at its insertion and along its length for any signs of abnormality.
Diagnostic Imaging
Plain Film Radiography
Anteroposterior View.
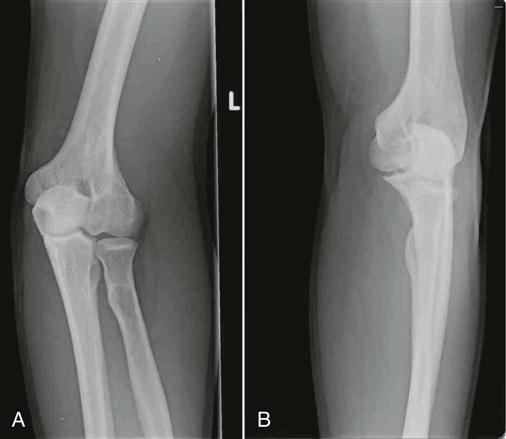
The examiner should note the relation of the epicondyles, trochlea, capitulum, radial head, radial tuberosity, coronoid process, and olecranon process (Figure 6-56). Any loose bodies, calcification, myositis ossificans, joint space narrowing, or osteophytes should be identified. If the patient is a young child, the examiner should check the epiphyseal plate to see if it is normal for each bone.
Lateral View.
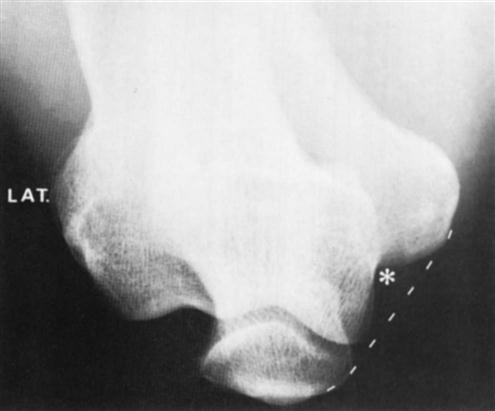
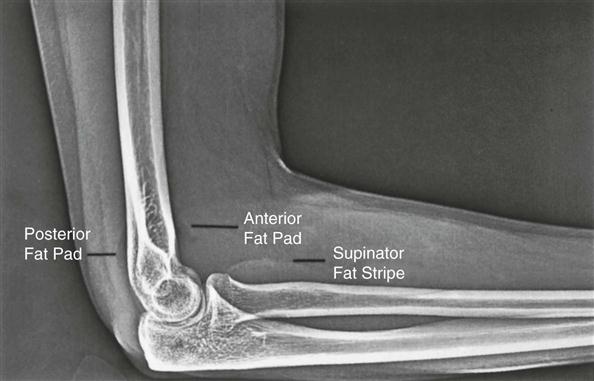
The examiner should note the relation of the epicondyles, trochlea, capitulum, radial head, radial tuberosity, coronoid process, and olecranon process. As with the anteroposterior view, any loose bodies, calcifications in or around the joint (Figure 6-58), myositis ossificans, dislocations (Figure 6-59), joint space narrowing, or osteophytes should be noted. The presence of the fat pad sign (Figure 6-60) occurs with elbow joint effusion and may indicate, for example, a fracture, acute rheumatoid arthritis, infection, or osteoid osteoma.64 Plain radiographs may also be used to visualize the cubital tunnel (Figure 6-61) and to measure the carrying angle (see Figure 6-7).

The posterior fat pad (arrows) is shown clearly on this lateral view with the arm flexed to 90°, indicating joint effusion. The anterior fat pad (open arrow) is clearly visible. There is a fracture of the coronoid process (curved arrow) and a loose body (arrowhead). (From Weissman BNW, Sledge CB: Orthopedic radiology, Philadelphia, 1986, WB Saunders, p. 179.)
Axial View.
This view is taken with the elbow flexed to 45°. It shows the olecranon process and epicondyles. It is useful for showing osteophytes and loose bodies.39
Arthrography
Figure 6-62 illustrates the views seen in normal elbow arthrograms. With the advent of magnetic resonance imaging (MRI), this technique is seldom used today.

Anteroposterior (A), external oblique (B), and lateral (C) views in extension show the normal annular (a), anterior (A), and posterior (P) recesses. D, Lateral tomogram with the arm extended. The area of the trochlea that is devoid of cartilage (arrow) is shown. (From Weissman BNW, Sledge CB: Orthopedic radiology, Philadelphia, 1986, WB Saunders, p. 178.)
Magnetic Resonance Imaging
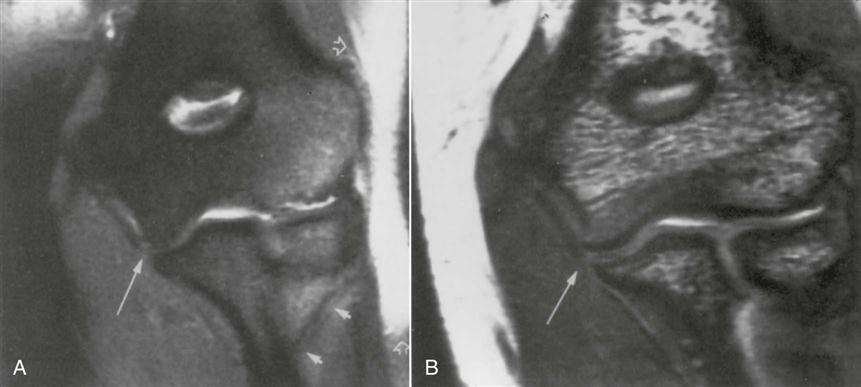
MRI is used to differentiate bone and soft tissues. Because of its high soft-tissue contrast, MRI, a noninvasive technique, is able to discriminate among bone marrow, cartilage, tendons, nerves, and vessels without the use of a contrast medium (Figures 6-63 to 6-65).65,66 The technique is used to demonstrate tendon ruptures, collateral ligament ruptures, cubital tunnel pathology, epicondylitis, and osteochondritis dissecans.67–69
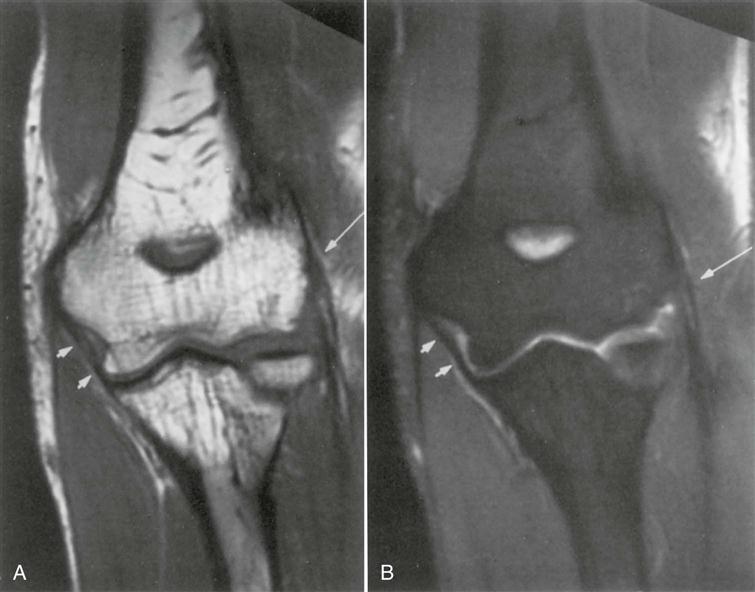
A, Oblique coronal T1-weighted A spine echo and fat-saturated proton density. B, Fast spin echo image demonstrates the normal, smooth, thin contour and low signal of the common extensor tendon (long arrow) and anterior bundle of the MCL (short arrows). (From Schenk M, Dalinka MK: Imaging of the elbow: an update. Orthop Clin North Am 28:519, 1997.)
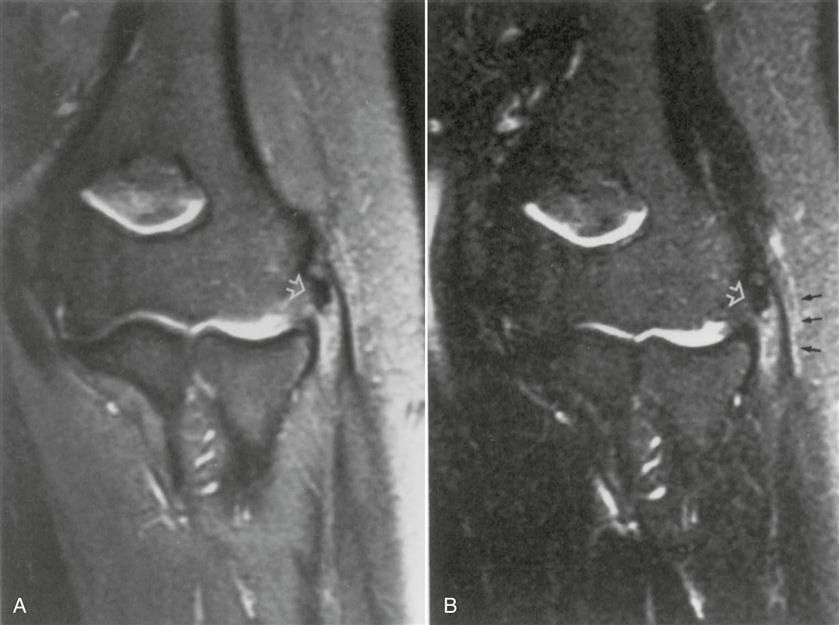
Oblique coronal fat-saturated proton density (A) and T2-weighted (B) fast spin echo images. Focal calcification within the common extensor tendon (white arrow). There is a moderately increased signal within the tendon, without fiber disruption. Note the edema in the peritendinous tissues (black arrows), suggesting active inflammation. (From Schenk M, Dalinka MK: Imaging of the elbow: an update. Orthop Clin North Am 28:524, 1997.)
Xerography
Figure 6-66 illustrates the detailed borders of the various structures around the elbow.

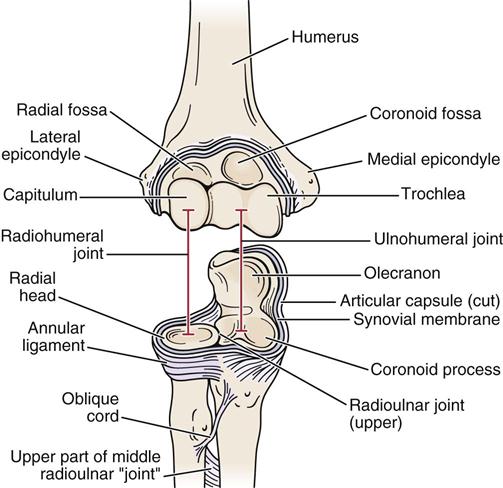
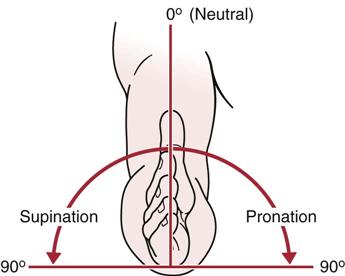

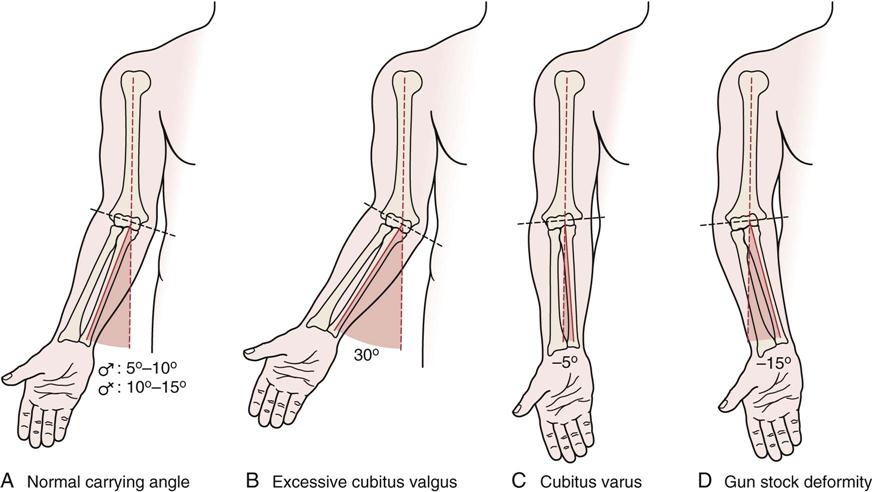
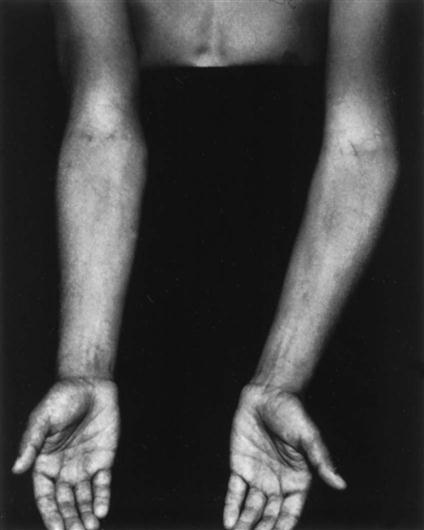
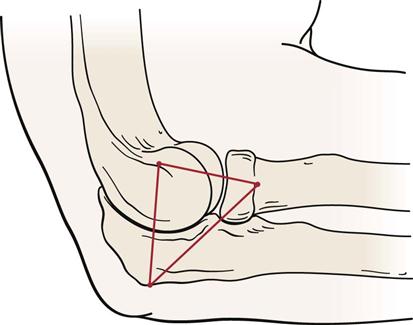
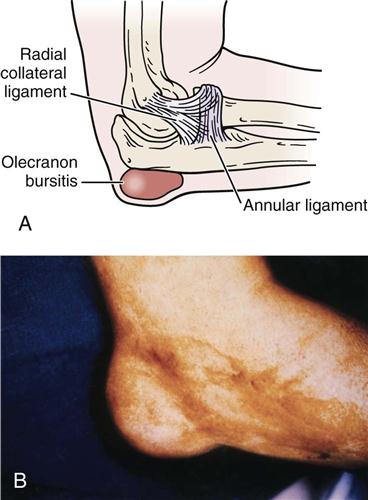

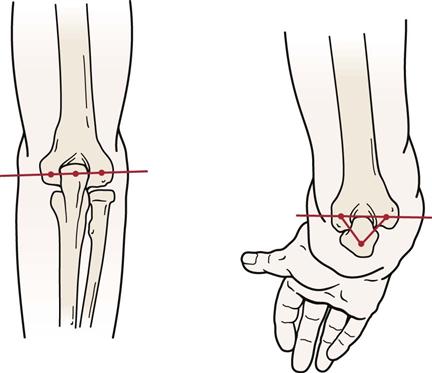
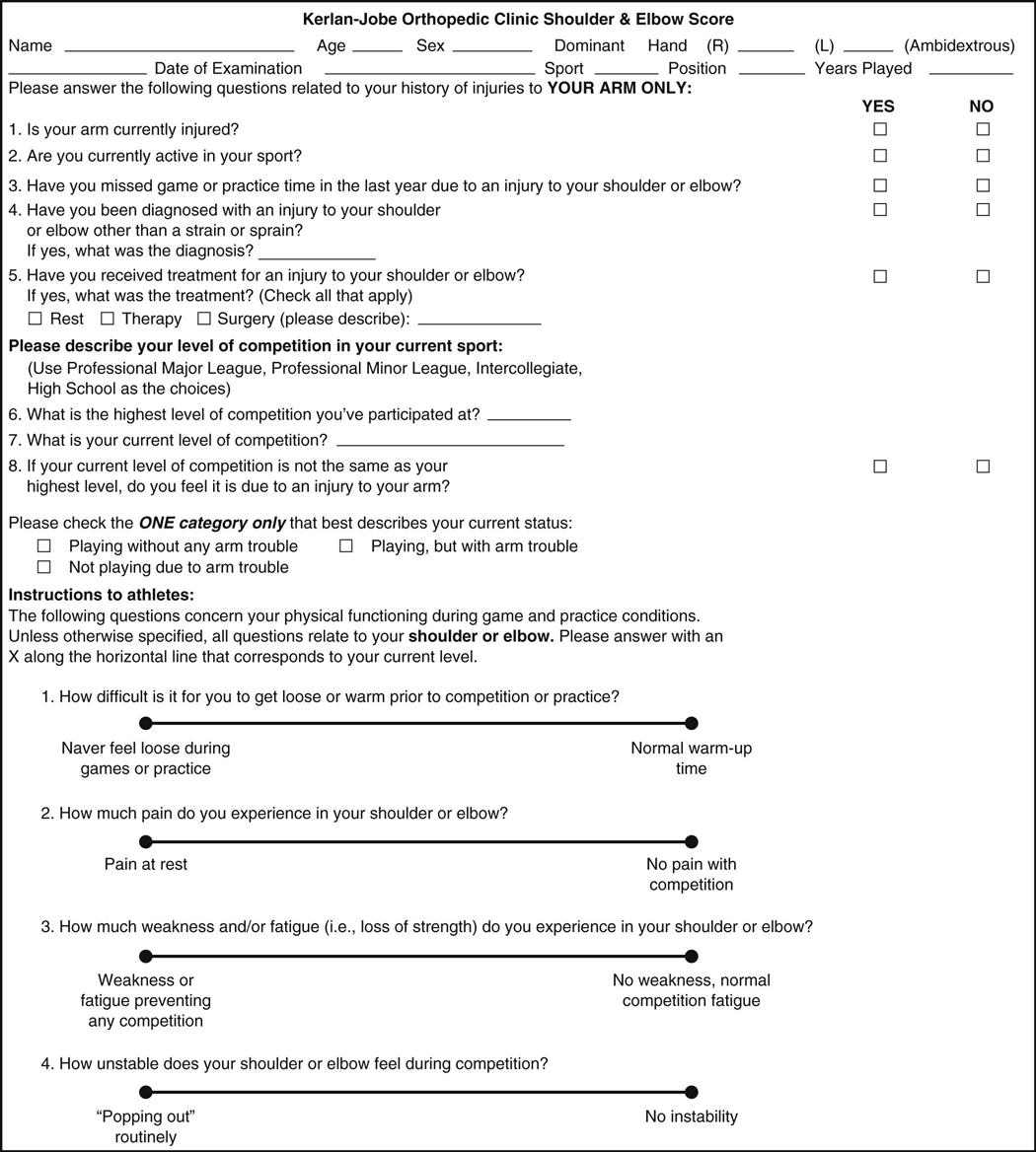
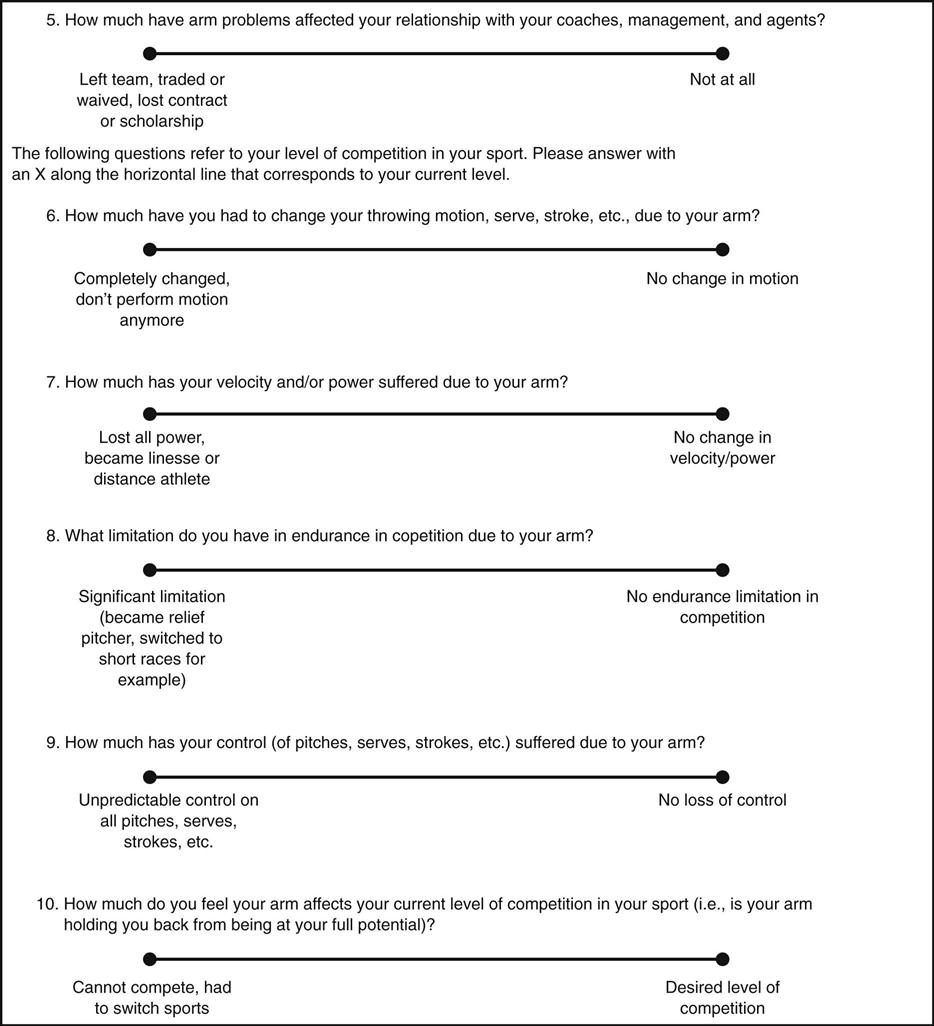
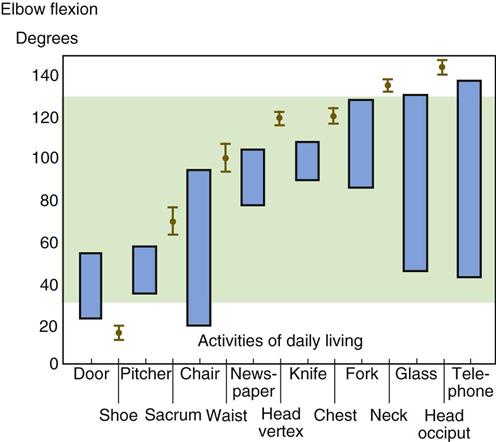
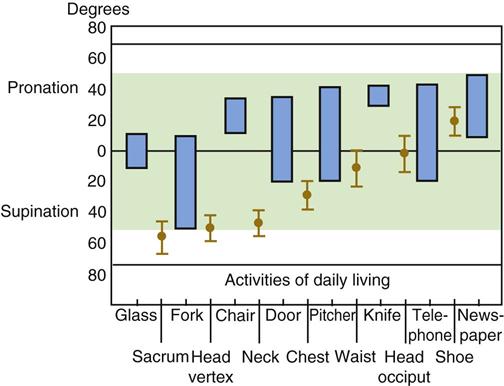
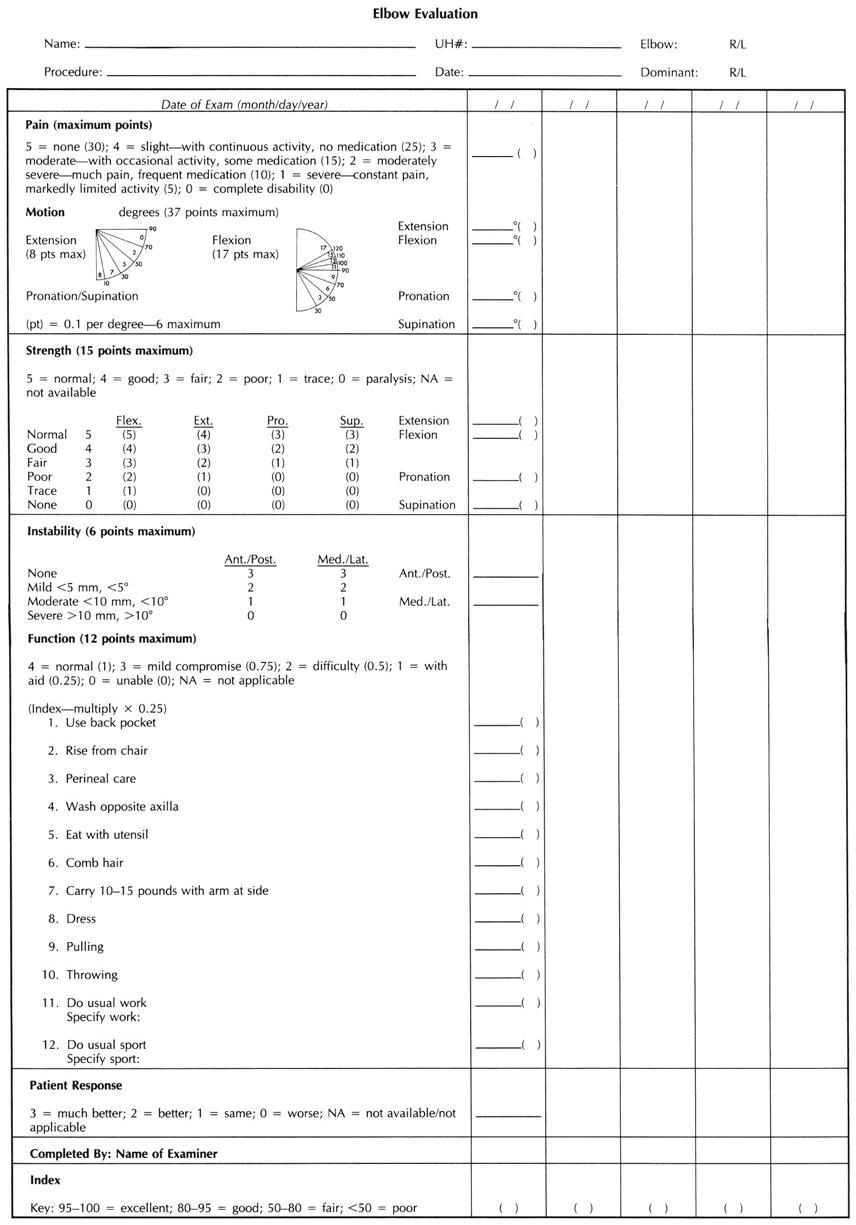
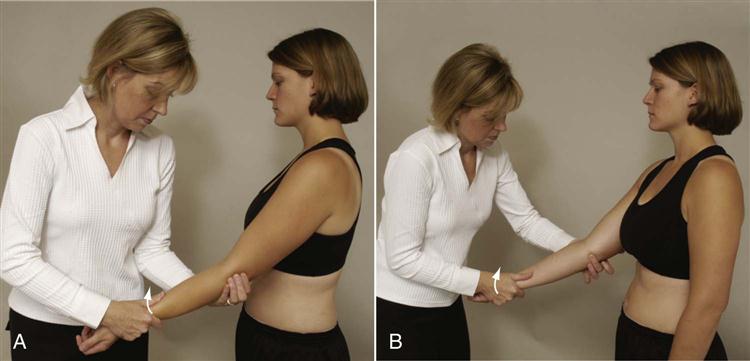
 Figure 6-25
Figure 6-25
 Figure 6-26
Figure 6-26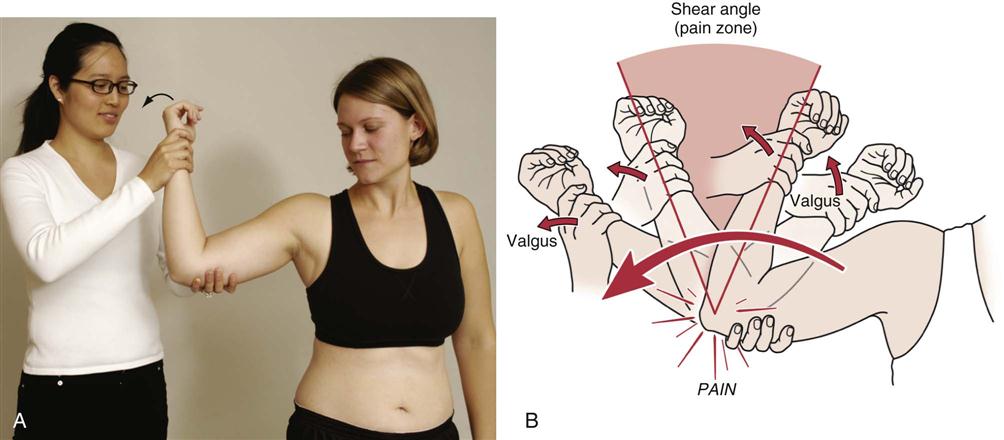
 Figure 6-27
Figure 6-27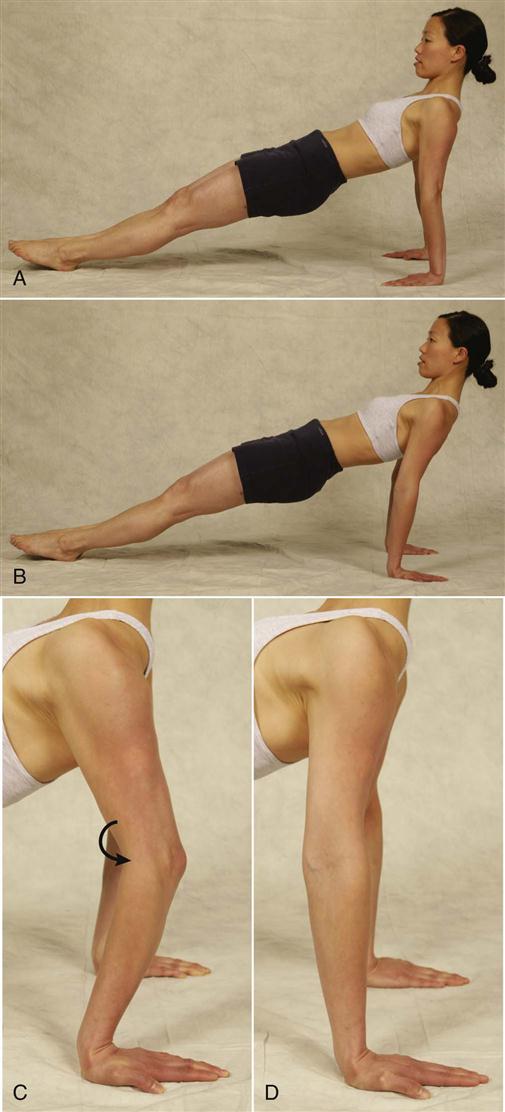
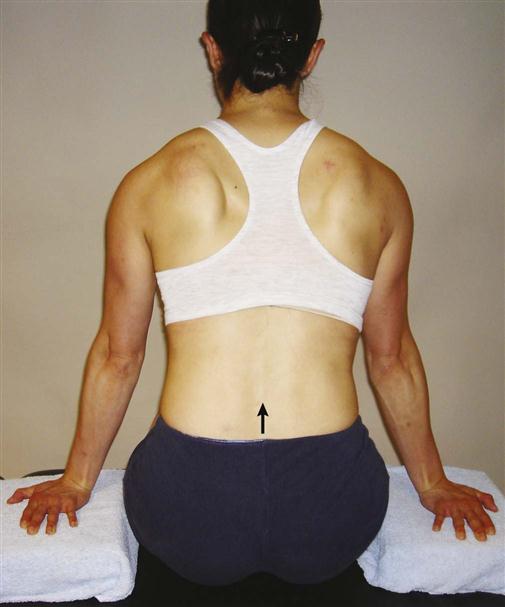

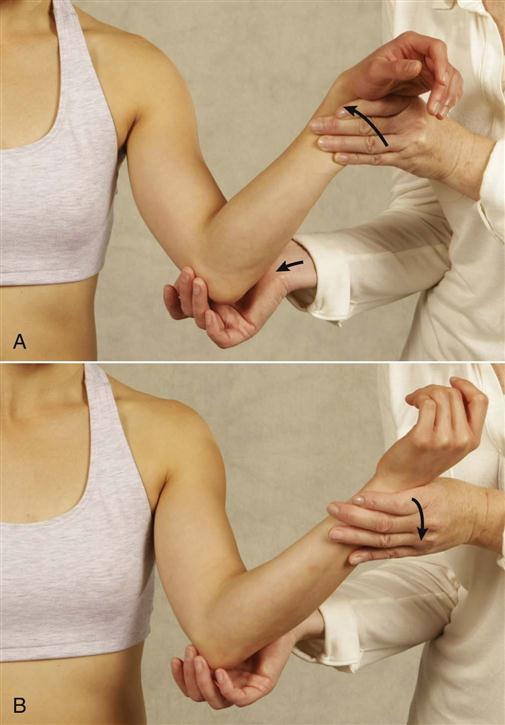
 Figure 6-35
Figure 6-35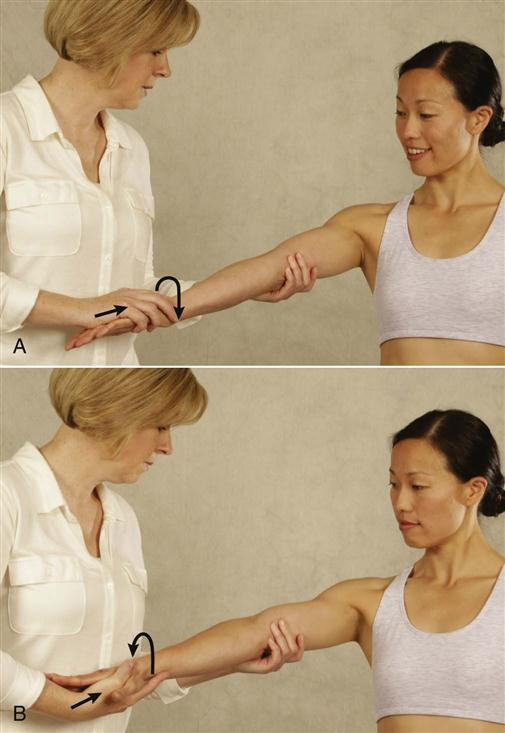
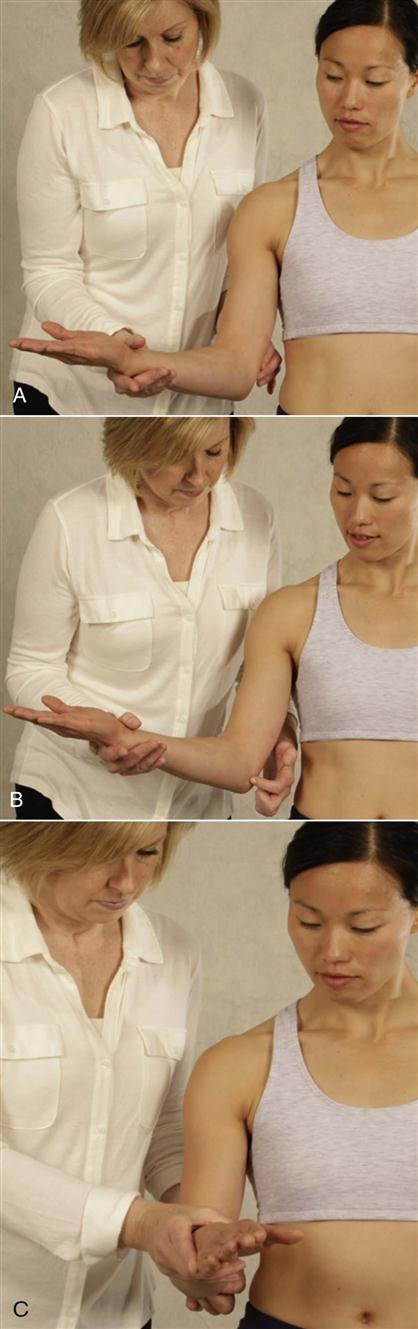
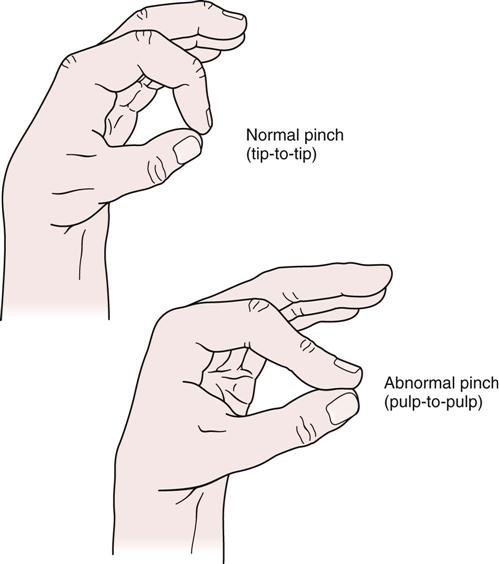
 Figure 6-43
Figure 6-43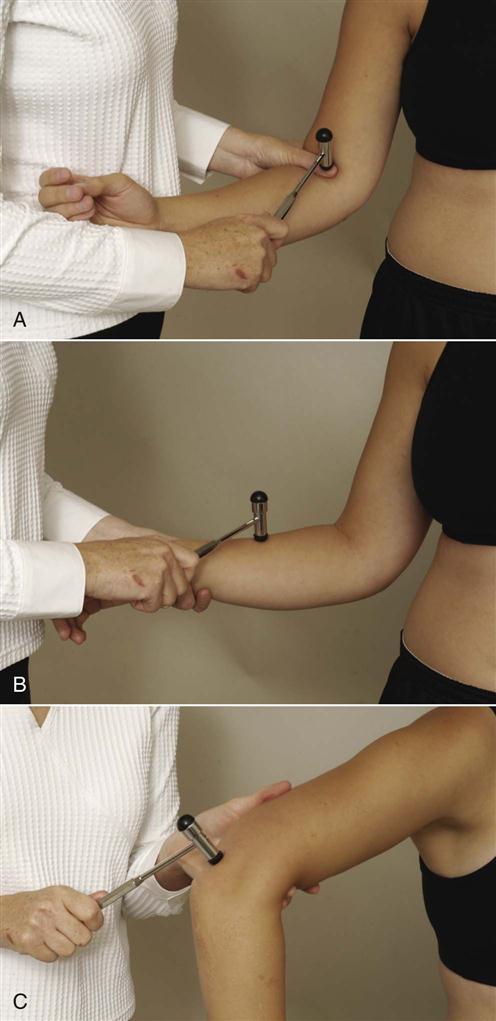

 Figure 6-53
Figure 6-53