Echocardiography in cardiac trauma
Overview
Cardiac injury as a result of blunt or penetrating chest trauma is common and associated with significant morbidity and mortality. Approximately 25% of traumatic deaths are caused by cardiac-related injuries, with the majority involving either cardiac or great-vessel damage.1 Most penetrating cardiac wounds are immediately fatal. For those arriving at the hospital alive, focused assessment with sonography for trauma (FAST) and transthoracic echocardiography (TTE) are the primary screening modalities. These injuries remain a challenge to trauma surgeons and are associated with high mortality. The incidence of blunt cardiac injury is unknown because of the lack of an accepted “gold standard” test for diagnosis. Blunt cardiac trauma can cause a wide spectrum of injuries (e.g., conduction abnormalities, valvular injuries, septum or free wall rupture, and coronary artery thrombosis).2
Patients with cardiac injury may have profound hypotension necessitating urgent surgery; however, a significant number of patients arrive at the emergency department without overt symptoms of heart injury.3 Regardless of the cause or the clinical picture, diagnosis should be made rapidly. If these patients are exposed to delays in diagnosis or treatment, deaths may occur that would otherwise have been classified as preventable.
The initial evaluation of patients who sustain cardiac trauma includes physical examination and chest radiography. The sensitivity and specificity of both modalities for diagnosing cardiac injury are low, however.4–6 Other diagnostic tools include subxiphoid exploration (SXE), two-dimensional TTE, transesophageal echocardiography (TEE), and FAST.
Diagnostic methods
Subxiphoid exploration
SXE is a time-tested technique that has proved to be accurate in diagnosing cardiac injuries. Disadvantages of its use relate to its lack of specificity for significant injury. Moreover, it is an operative procedure that subjects patients to the risks associated with surgery and general anesthesia. The rate of negative explorations approaches 75% to 80% in most series.7
Focused assessment with sonography for trauma
FAST has become an integral part of primary cardiac injury evaluation because it is valuable in the diagnosis of pericardial effusion (sensitivity, 92% to 100%; specificity, 99% to 100%).6,8 However, absence of pericardial fluid rules out tamponade, but it does not rule out cardiac injury. FAST cannot assess cardiac function or detect valvular injuries.
Transesophageal echocardiography
TEE identifies the presence of ventricular dysfunction in suspected cases of myocardial contusion9 and is sensitive in detecting thoracic aortic injury and evaluating valvular structure and function.10 However, TEE is a semiinvasive method that may require sedation, and it might sometimes prove difficult to perform the examination (e.g., cervical spine, facial, airway, or esophageal injuries). TEE is an operator-dependent imaging modality. It is difficult to find experienced operators to perform the examination in emergency environments; however, this does not apply to the intensive care unit (ICU).
Transthoracic echocardiography
TTE was introduced in the field of trauma surgery more than 30 years ago. This noninvasive diagnostic modality is readily available and portable and lacks ionizing radiation. TTE gained widespread acceptance in detecting cardiac injuries mainly because of its high sensitivity in identifying pericardial effusion. Jimenez et al11 prospectively compared TTE with SXE. They performed TTE in 73 stable patients with penetrating chest wounds. The reliability of TEE was comparable to that of SXE, with a sensitivity of 90%, specificity of 97%, and accuracy of 96%. Freshman et al5 performed TTE in 36 hemodynamically stable patients with penetrating chest injuries. Of the four patients with abnormal findings, three had small pericardial effusions. All three patients recovered without sequelae after a period of observation. The fourth patient had a large pericardial effusion, and sternotomy revealed significant left ventricular injury. The authors concluded that TTE is an adequate alternative to other conventional diagnostic tests. Beggs et al12 evaluated 40 patients with blunt chest trauma. Nine patients had abnormal echocardiograms, with findings of pericardial effusion in four, chamber enlargement in three, and echodense right ventricular areas in two. The authors concluded that TTE can be used as a noninvasive modality to complement other clinical tools in the detection of blunt cardiac injury.
Disorders
Cardiac tamponade
Echocardiography is the method of choice for diagnosing pericardial effusion and cardiac tamponade. Echocardiographic findings in patients with cardiac tamponade include cardiac chamber compression, inferior vena cava (IVC) plethora, Doppler flow velocity paradoxus, compression of the pulmonary trunk, compression of the thoracic IVC, paradoxic motion of the interventricular septum, and swinging motion of the heart in the pericardial sac.13 The thinner, more compliant right-sided chambers are usually the first to be compressed in the setting of cardiac tamponade. Right ventricular and atrial collapse is a commonly used clue for tamponade; however, neither is 100% sensitive or specific for tamponade.7
Traumatic valvular injury and dysfunction
Traumatic valvular dysfunction is relatively uncommon but should be considered if pulmonary edema develops after chest trauma. The aortic valve is the most commonly injured, followed by the mitral and tricuspid valves.14 Zakynthinos et al15 reported two patients with severe acute mitral valve and tricuspid valve insufficiency caused by valve rupture as a result of blunt chest trauma. TTE disclosed atrioventricular regurgitation in both patients.
Complications of cardiac injuries
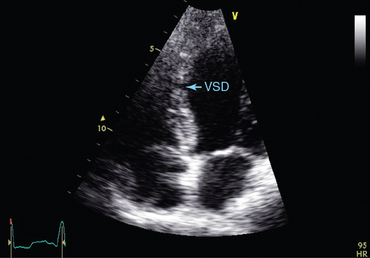
Echocardiography is useful not only in evaluating acute cardiac trauma but also in detecting potential complications. Patients who survive the cardiac injuries may suffer from short- and long-term complications, such as ischemia and posttraumatic acute myocardial infarction, defects in the ventricular septum or valves, arteriovenous fistula, foreign body, and thrombus. Demetriades et al16 assessed 44 survivors of penetrating cardiac injuries for late cardiac complications. TTE revealed abnormalities in 17 patients (39%). Ten patients (23%) had valvular or septal defects. Other abnormalities included pericardial effusion, ventricular and septal dysfunction, and ventricular dilatation. The authors concluded that the incidence of late sequelae after cardiac injury is high and recommended that follow-up be performed routinely in these patients. Mattox et al17 investigated delayed sequelae and complications of penetrating and blunt cardiac trauma in 204 patients. They reported complications in 4% to 56% of survivors. One hundred twenty-eight of these patients survived. Of the 90 who underwent cardiorrhaphy in the operating room, 78 survived. TTE was performed in 40 patients for suspected significant residual injury. Eight of the 40 required secondary cardiac operations. TTE demonstrated pericardial effusion, abnormal chamber enlargement, abnormal cardiac wall motion, an intracardiac missile, and intracardiac and pleural thrombosis. Pulsed Doppler findings included a VSD, tricuspid insufficiency, and right ventricular turbulence secondary to arteriovenous fistulas.
Pitfalls and limitations
Several authors have highlighted the pitfalls of TTE and FAST in the evaluation of cardiac injuries. Rozycki et al18 presented a series of 313 consecutive patients with penetrating precordial or transthoracic injuries. Two patients (0.6%) were found to have false-positive findings on pericardial FAST examination. Both patients had large left hemothoraces and blood in the mediastinum without associated heart injuries. The authors suggested that a massive hemothorax surrounding the pericardium may result in false-positive findings and therefore recommended repeating the examination after evacuation of the blood by tube thoracostomy. Massive hemothorax may also lead to false-negative results. In a cohort of 228 patients with penetrating wounds involving the precordial area, false-negative FAST and TTE results were found in 5 patients (2.2%). All five patients also had concurrent left hemothoraces.19 Meyer et al evaluated 145 hemodynamically stable patients for occult cardiac injury.20 All patients underwent TTE and SXE. TTE missed four significant injuries. When comparing SXE with TTE in patients without hemothorax, however, the sensitivity (100% vs. 100%), specificity (89% vs. 91%), and accuracy (90% vs. 91%) were comparable, thus suggesting that TTE is an acceptable diagnostic option for detecting cardiac injury but may have significant limitations in identifying cardiac injury in patients with concurrent hemothorax.
TTE is of limited diagnostic value in patients with aortic injury.21 Contrast-enhanced computed tomography (CECT) scans and TEE are considered the methods of choice for evaluating aortic injuries (see Section 8). Finally, the performance of TEE and TTE operators is based on their experience and technical skill.22,23 Blaivas et al24 asked residents and faculty members from an emergency medicine training program at a level 1 trauma center to view digitized video clips of ultrasound subxiphoid cardiac examinations in patients with chest trauma. The participants had difficulty distinguishing between epicardial fat pads and true pericardial effusions, which resulted in an overall sensitivity of 73% and specificity of 44%.
Pearls and highlights
• TTE is a readily available bedside examination that does not require transfer of patients to another facility.
• TTE in the acute trauma setting may allow detection of myocardial wall motion and valvular abnormalities, as well as pericardial effusions; however, it may be difficult to perform if the chest acoustic windows are obscured, and it is also subject to various other technical limitations.
• FAST examination is easily applicable and has become an integral part of the primary survey for cardiac trauma since it is valuable in diagnosing pericardial effusions.
• Multidetector CECT and TEE are both pivotal imaging modalities for the evaluation of patients with cardiac and aortic injuries. TEE has a limited role in acute trauma settings but is useful in the ICU to monitor for possible complications.
• Oftentimes, diagnostic modalities are of limited importance in the acute phase of cardiac injury because patients may need to be transferred urgently to the operating room.
References
1. Symbas, PN. Cardiothoracic trauma. Curr Probl Surg. 1991; 28:741–797.
2. Pasquale, MD, Nagy, K, Clarke, J. Eastern Association for the Surgery of Trauma. Practice management guidelines for screening of blunt cardiac injury. J Trauma. 1998; 44:94–956.
3. Moreno, C, Moore, EE, Majure, JA, et al, Pericardial tamponade: a critical determinant for survival following penetrating cardiac wounds. J Traum. 1986; 26:821.
4. Ivatury, RR. The injured heart. In: Moore EE, Mattox KL, Feliciano DV, eds. The injured heart. ed 4. San Francisco: McGraw-Hill; 2000:545–558.
5. Freshman, S, Wisner, D, Weber, C, 2-D echo: emergent use in the evaluation of penetrating precordial trauma. J Traum. 1991; 31:902–906.
6. Kelley, J, Henderson, S, Newton, K. Bedside ultrasound in delayed traumatic pericardial effusion. Am J Emerg Med. 1999; 17:313–331.
7. Thorson, C, Namias, N, Van Haren, R, et al. Does hemopericardium after chest trauma mandate sternotomy. J Trauma Acute Care Surg. 2012; 72:1518–1527.
8. Spodick, DH. Acute cardiac tamponade. N Engl J Med. 2003; 349:684–690.
9. Weiss, RL, Brier, JA, O’Connor, W, et al. The usefulness of transesophageal echocardiography in diagnosing cardiac contusions. Chest. 1996; 109:73–77.
10. Nekkanti, R, Aaluri, SR, Nanda, NC, Mukhtar, O. Transesophageal echocardiographic diagnosis of traumatic rupture of the noncoronary cusp of the aortic valve. Echocardiography. 2001; 18:189–190.
11. Jimenez, E, Martin, M, Krukenkamp, I, et al, Subxiphoid pericardiotomy versus echocardiography: a prospective evaluation of the diagnosis of occult penetrating cardiac injury. Surger. 1990; 108:676.
12. Beggs, C, Helling, T, Evans, LE, et al. Evaluation of cardiac injury by two-dimensional echocardiography in patients suffering blunt chest trauma. Ann Emerg Med. 1987; 16:542–545.
13. Restrepo, CS, Lemos, DF, Lemos, JA, et al. Imaging findings in cardiac tamponade with emphasis on CT,. Radiographics. 2007; 27:1595–1610.
14. Kan, CD, Yang, YJ. Traumatic aortic and mitral valve injury following blunt chest injury with a variable clinical course. Heart. 2005; 9:568–570.
15. Zakynthinos, E, Vassilakopoulos, T, Routsi, C, et al, Early- and late-onset atrioventricular valve rupture after blunt chest trauma: the usefulness of transesophageal echocardiography. J Traum. 2002; 52:990–996.
16. Demetriades, D, Charalambides, C, Sareli, P, Pantanowitz, D. Late sequelae of penetrating cardiac injuries. Br J Surg. 1990; 77:813–814.
17. Mattox, KL, Limacher, MC, Feliciano, DV, et al. Cardiac evaluation following heart injury. J Trauma. 1985; 25:758–765.
18. Rozycki, GS, Ballard, R, Feliciano, DV, et al, Surgeon-performed ultrasound for assessment of truncal injuries: lessons learned from 1,540 patients. Ann Sur. 1998; 228:16–28.
19. Ball, C, Williams, B, Wyrzykowski, A, et al. A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. J Trauma. 2009; 67:1123–1124.
20. Meyer, D, Jessen, ME, Grayburn, PA, The use of echocardiography to detect cardiac injury after penetrating thoracic trauma: a prospective study. J Traum. 1995; 39:902–907.
21. Weiss, RL, Brier, JA, O’Conner, W, et al. The usefulness of transoesophageal echocardiography in diagnosing cardiac contusions. Chest. 1996; 109:73–77.
22. Dente, CJ, Rozycki, GS. Surgeon-performed ultrasound in trauma and surgical critical care. In: Feliciano DV, Mattox KL, Moore EE, eds. Trauma. ed 6. New York: McGraw-Hill; 2008:321.
23. Speight, J, Sanders, M. Pericardial tamponade with a positive abdominal FAST scan in blunt chest trauma. J Trauma. 2006; 61:743–745.
24. Blaivas, M, DeBehnke, D, Phelan, MB. Potential errors in the diagnosis of pericardial effusion on trauma ultrasound for penetrating injuries. Acad Emerg Med. 2000; 7:1261–1266.