Chapter 12. Ears
Rationale
Ear disorders are disruptive to language, speech, and social development. Early screening and detection can assist in minimizing or eliminating hearing deficiencies and their effects. Temporary and correctable conditions such as otitis media are common in young children but might go undetected. Abnormalities of the external ear can be important in alerting health professionals to the presence of syndromes and should be reported. Assessment of the ear is performed in conjunction with the eye examination, because eye problems are nearly twice as common in children with hearing deficiencies.
Anatomy and Physiology
The ear consists of the external ear, middle ear, and inner ear. The outer ear consists of the auricle, cartilaginous shell, and external ear canal. In children younger than 3 years the canal points upward; in older children it is directed downward and forward. The lining of the external ear canal secretes cerumen, which protects the ear.
The middle ear consists of the tympanum (eardrum) and three bones (ossicles) that touch the tympanum on one side and the membrane covering the opening to the inner ear on the other side. Vibrations of the tympanum are transmitted through the ossicles to the inner ear. The middle ear also contains an opening to the eustachian tube. The eustachian tube allows secretions to pass from the middle ear to the nasopharynx and enables air to enter the middle ear from the throat. Equalization of air pressure between the external ear canal and middle ear is essential for proper functioning of the tympanic membrane. The shorter and less angled eustachian tube in infants and young children permits secretions from the nose and throat to readily enter the middle ear, predisposing this age group to more frequent ear infections.
The inner ear contains auditory nerve endings, which pick up sound waves from the middle ear and transmit them along the eighth cranial nerve, or auditory nerve, to the brain. Sound waves that contact the skull directly can also be picked up by the inner ear. The inner ear contains the structures for balance and hearing.
The three divisions of the ear develop in the embryo at the same time as other vital organs are developing, which is why deformities of the ears can provide clues to developmental aberrations elsewhere in the body. External ear development begins at about the fifth week of gestation, and middle ear development begins at around the sixth week. The ears are particularly vulnerable to developmental aberration in the ninth week of gestation.
Neonates are capable of sound discrimination at birth and respond more readily to high-pitched voices. The presence of mucus in the eustachian tube can limit hearing when the neonate is first born but clears shortly after birth. Vernix caseosa in the external ear canal can make visualization of the tympanic membrane difficult.
The young infant responds to loud noises with the startle reflex, blinking, or cessation of movement. Infants 6 months of age or older attempt to locate the source of the sound.
Equipment for Ear Assessment
▪ Otoscope
▪ Ear speculum
Preparation
Ask about family history of hearing problems, prenatal influences (infection, alcohol use), postnatal factors (mechanical ventilation, neonatal jaundice, asphyxia at birth), childhood infections (mumps, measles, ear and respiratory tract infections), surgery to the ear, use of ototoxic drugs, head trauma, and exposure to loud noises (e.g., music).
If an otoscopic examination is to be performed in a young child or infant, it is safer to restrain the child. Explain and demonstrate to the parent how to hold the child. The child can be placed on the side or abdomen, with the hands at the side and the head turned so that the ear to be examined points toward the ceiling. The parent can assist by placing one hand on the child’s head above the ear and the other on the child’s trunk. Alternatively, the child can sit on the parent’s lap with one arm tucked behind the parent’s back. The parent holds the child’s head against his or her shoulder and the child’s other, free arm (Figure 12-1).
 |
| Figure 12-1Position for restraining infant or child during otoscopic examination.(From Hockenberry MJ et al: Wong’s nursing care of infants and children, ed 7, St Louis, 2003, Mosby.)Elsevier Inc. |
| Assessment | Findings |
|---|---|
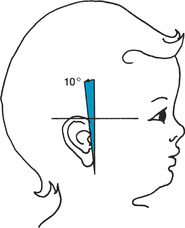
| Examine the ear for placement and position. | The top of the ear should cross an imaginary line from the inner eye to the occiput. The pinna should deviate no more than 10 degrees from a line perpendicular to the horizontal line. (Use of a pen or tongue blade can provide more concrete estimations of where the ear is positioned in relation to a vertical line.) Figure 12-2 illustrates normal placement and position of the ear. |
| Assessment | Findings | ||||
|---|---|---|---|---|---|
|
Clinical Alert
Low or obliquely set ears are sometimes seen in children with genitourinary or chromosomal abnormalities and in many syndromes.
|
|||||
| Observe the ears for protrusion or flattening. |
The ears of neonates are flat against the head.
Clinical Alert
Flattened ears in older infants can suggest persistent side lying.
Protruding ears can indicate swelling related to insect bites or to conditions such as mastoiditis, postauricular abscess, or mumps.
|
||||
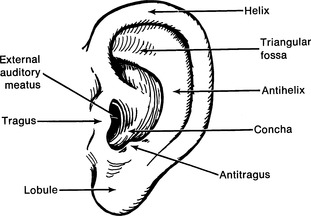
| Inspect the external ear for unusual structure and markings and the skin around the ear for sinuses and small openings. Figure 12-3 illustrates usual markings. |
Markings and structure of the external ear vary little from child to child. Variations can be normal but should be recorded. For example, a small skin tag on the tragus is a remnant of embryonic development and suggests no pathologic process. Skinfolds can be absent from the helix.
Parents and children might be sensitive about this abnormality.
Clinical Alert
|
||||
| Inspect the external ear canal for general hygiene, discharge, and excoriations. |
A sinus can indicate a fistula that drains into the ear or neck.
The skin of the external auditory meatus (see Figure 12-3) is normally flesh colored. Soft yellow-brown wax is normal. If cerumen is hard, it will appear dark, crusted, and dry.
|
| Assessment | Findings |
|---|---|
|
Absence of wax in the external ear can indicate overly vigorous cleaning. Hygienic measures can best be determined by commenting on how clean the ears are and then asking how the ears are cleaned. Parents might need teaching about the dangers of using sharp objects. Advise use of a soft washcloth.
Absence of wax can also be related to acute otitis media. If cleaning practices are acceptable, ask about ear pulling, irritability, and fever.
|
| Assessment | Findings |
|---|---|
|
Foul-smelling yellow or green discharge can indicate rupture of a tympanic membrane or recent insertion of myringotomy tubes.
Bloody discharge can indicate foreign body irritation, scratching, or trauma or rupture of tympanic membrane.
Serous discharge can indicate allergies.
Clear discharge can indicate a CSF leak from skull fracture.
|
|
| Pull on the auricle. |
Pulling normally produces no pain and does not produce pain in purulent otitis media.
Clinical Alert
Pain produced by pulling on the auricle can indicate otitis externa. Pain will not be produced in purulent otitis media.
|
| Palpate the bony protuberance behind the ear (mastoid) for tenderness. |
No pain or tenderness should be experienced when the mastoid is palpated.
Clinical Alert
Pain and tenderness over the mastoid process can indicate mastoiditis.
|
Assessment of Hearing Acuity
Hearing loss is the most common disability. The three types of hearing loss are conduction hearing loss, sensorineural loss, and mixed loss. Conduction hearing loss results from disruption of sound transmission through the outer and middle ear, most often as the result of serous otitis media. Sensorineural loss is a result of damage to the inner ear or auditory nerve. Mixed loss reflects both conduction and sensorineural hearing loss.
Assessment and detection of hearing impairments are critical components of a health evaluation. Assessment involves identifying children who are at risk for hearing impairments by virtue of their history, observing for behaviors that would suggest a hearing loss, and screening for hearing acuity.
Preparation
Inquire about weight at birth and presence of hyperbilirubinemia as a neonate. Ask if child was on prolonged mechanical ventilation as a neonate or required admission to neonatal intensive care for 48 hours or more, or if child has had meningitis, mumps, frequent ear infections, or experienced head trauma. Inquire about family history of hearing disorders or hearing loss. Ask about use of alcohol during pregnancy. Ask if parents have concerns about their child’s hearing, speech, or language. Inquire about use of hearing aids.
Equipment for Assessment of Hearing Acuity
▪ Noisemakers (squeeze toy, rattle, bell, paper)
▪ Tuning fork
▪ Tympanometer
▪ Audiometer
| Assessment | Findings |
|---|---|
| Infant | |
| Assume that parents’ impressions of their infant’s hearing difficulties are correct unless otherwise proven. | |
| Assessment | Findings |
|---|---|
| Ask if infant wakes in response to loud noises, if infant turns to an interesting sound, or if infant is beginning to repeat some of the sounds that parents make. | |
|
Stand behind the infant and ring a small bell, move a rattle, snap fingers, clap hands, or rustle paper.
Be careful not to bump the examining table or to cause an air stream because this evokes a false response from the infant.
|
The infant younger than 4 months evidences a startle reflex. Infants 6 months of age or older try to locate the sound by shifting their eyes or turning their heads. The infant might also cease sucking or other movement in response to sound. Infants older than 12 months will localize to all sounds beside, below, and above.
Clinical Alert
Suspect hearing loss in a young infant who does not startle or cease movement or who has been premature and in intensive care.
Suspect hearing loss in an older infant who does not attempt to localize sound.
|
|
Preschool-Age Child
Stand 0.6 to 0.9 m (2 to 3 ft) in front of the child and give commands, such as “Please give me the doll.”
School-Age Child or Adolescent
Stand about 0.3 m (1 ft) behind the child. Instruct the child to cover one ear.
|
| Assessment | Findings |
|---|---|
|
Ask the child to repeat what is heard while you whisper numbers in random order.
Repeat the process with the other ear.
|
|
| Rinne’s Test (to compare air and bone conduction) | |
|
Strike the tuning fork against your palm, then hold the stem to the child’s mastoid process. When the child indicates that the sound is no longer audible, hold the prongs near the external meatus of one ear and ask the child if the sound can be heard.
Repeat the process with the other ear.
Not useful in toddlers because the test requires the cooperation and ability of the child to signal when the sound is no longer audible.
|
Normally the child can hear the sound of the tuning fork at the external meatus after it is no longer audible at the mastoid process (positive test result) because air conduction is better than bone conduction.
Sound should be heard equally well in both ears (positive test result).
Clinical Alert
Interference with conduction of air through the external and middle chambers causes the child to experience sound better through bone conduction.
|
| Weber’s Test (to differentiate conduction from sensorineural deafness) | |
|
Strike the tuning fork against the palm and hold the stem in the midline of the child’s head. Ask the child where sound is heard best.
Not useful for young children because of difficulty discriminating among “better, more, less.”
|
Clinical Alert
With air conduction loss the sound is heard best in the affected ear. The sound is heard best in the unaffected ear if loss is sensorineural.
|
| Assessment | Findings |
|---|---|
| Tympanometry | |
|
Tympanometry is used to evaluate middle ear infection in children older than 7 months, although some sources suggest that it is not useful as a screening tool in a health examination. Tympanometry provides information about the presence of fluid in the middle ear, mobility of the tympanic membrane, and ear canal volume. It is quick, painless, and is not influenced by environmental noise. Some sources recommend training by an audiologist in this procedure.
Before placing the tympanometer, examine the ear with the otoscope to ensure that the path to the drum is clear. If child is older, warn that a noise will be heard after the tympanometer is placed, but that the test is not uncomfortable. Place the portable tympanometer in the ear. A soft tone will be transmitted through the probe while pressure is changed in the outer canal. Results will be recorded on a graph or tympanogram.
|
An A curve is considered normal in a tympanogram.
Clinical Alert
If the tympanogram shows an
As curve, the stapes might be partially immobilized.
If the tympanogram shows an Ad curve, this indicates flaccidity of the tympanic membrane and separation of middle ear bones.
If the tympanogram shows a B (flat) curve, this indicates fluid in the eardrum.
If the tympanogram shows a C curve, this indicates a retracted eardrum and decreased pressure in the eardrum.
|
| Assessment | Findings |
|---|---|
| Audiometry | |
| Audiometry is used to assess the threshold of hearing for pure tone frequencies (measured in hertz or Hz) at varying levels of loudness (measured in decibels or dB). In threshold acuity, the child is presented with a sound that is easily heard. The sound is gradually reduced in loudness until it is no longer audible to the child. The child usually wears headphones and is instructed to hold up a hand or push a button when the sound is heard. Audiometry is not considered reliable for children younger than 5 years, although young children might be able to respond if they practice with the equipment. | |
Otoscopic Examination
The apprehension many children feel about the otoscopic examination can be lessened by letting them see and handle the otoscope and to turn the light on and off. Reassure that the examination might tickle but does not hurt. Playing a game such as “let’s look for the elephant in your ear” can help allay fear (after the examination, it is important to explain that “the elephant” was only pretend). Demonstrating on a doll can also reduce apprehension. It is helpful to move the speculum around the outer rim of the meatus to allow the child to adjust to the feel of the speculum. Restrain infants to prevent sudden movement.
| Assessment | Findings | ||
|---|---|---|---|
|
Select the largest speculum that fits comfortably into the ear canal. Hold the otoscope in an inverted position.
Check the canal opening for foreign bodies and scratches.
Straighten the ear canal. In children younger than 3 years, pull the earlobe gently down and out. In children older than 3 years, pull the pinna up and back.
Place the speculum in the canal. In children younger than 3 years, direct the speculum upward; in children older than 3 years, direct it downward and forward.
Avoid sudden movement. In otoscopes with a pneumonic attachment, air can be introduced and removed from the ear canal by squeezing a rubber bulb during otoscopic examination.
Inspect the ear canal for lesions, discharge, cerumen, and foreign bodies. Inspect the tympanic membrane for bony landmarks, color, fluid level, bubbles, scarring, holes, and vesicles.
|
The ear canal is normally pink, but can be more pigmented in dark-skinned children, and has minute hairs.
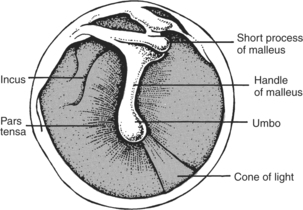
The tympanic membrane is translucent and pearly pink or gray. Slight redness is normal in newborns and can be normal in older children and infants who have been crying. The tenseness of the membrane causes the otoscopic light to reflect at the 5 o’clock (right ear) or 7 o’clock (left ear) position. The light reflex is a cone-shaped reflection pointing away from the face. The umbo (tip of the malleus) appears as a small, round, concave spot near the middle of the eardrum. The manubrium (handle of the malleus) appears as a whitish line up from the umbo to the membrane margin. A sharp, knoblike protrusion at the 1 o’clock position represents the short process of the malleus (Figure 12-4).
Clinical Alert
A red, bulging tympanic membrane, dull or absent light reflex, and obscured bony landmarks can indicate acute otitis media (erythema itself does not indicate acute otitis media).
|
| Assessment | Findings |
|---|---|
|
A dull yellow or gray tympanic membrane can indicate serous otitis media.
An ashen-gray membrane can suggest scarring from a previous rupture or perforation.
A black area on the tympanic membrane suggests a perforation that has not yet healed. An area of thin-appearing membrane suggests a healed perforation.
Absence of movement of the tympanic membrane with the introduction of air can indicate chronic ear infection.
An apparent line that changes position with movement suggests fluid is present. Circles or rings behind the membrane suggest bubbles in the fluid. Vesicles on the membrane are suggestive of viral infections.
|
Related Nursing Diagnoses
Pain: related to infection.
Impaired social interaction: related to communication barriers.
Social isolation: related to inability to engage in satisfying personal relationships.
Impaired verbal communication: related to physical barrier, anatomic defect, alteration of central nervous system.
Impaired parenting: related to lack of resources, lack of knowledge about health maintenance, physical illness.
Altered family processes: related to shift in health status of family member.
Disorganized infant behavior: related to illness, congenital or genetic disorders, teratogenic exposure, sensory deprivation, cue misreading.
Sensory/perceptual alterations (visual, auditory): related to altered sensory perception, altered sensory reception.
Hyperthermia: related to illness affecting temperature regulation.
Chronic low self-esteem: related to perception of disability.
Risk for altered development: related to hearing impairment or frequent otitis media.